Abstract
Introduction
Survivors of cancer may experience lingering adverse skeletal effects such as osteoporosis and osteomalacia. Skeletal disorders are often associated with advancing age, but these effects can be exacerbated by exposure to cancer and its treatment. This review will explore the cancer and cancer treatment-related causes of skeletal disorders.
Methods
We performed a comprehensive search, using various Internet-based medical search engines such as PubMed, Medline Plus, Scopus, and Google Scholar, for published articles on the skeletal effects of cancer and cancer therapies.
Results
One-hundred-forty-two publications, including journal articles, books, and book chapters, met the inclusion criteria. They included case reports, literature reviews, systematic analyses, and cohort reports. Skeletal effects resulting from cancer and cancer therapies, including hypogonadism, androgen deprivation therapy, estrogen suppression, glucocorticoids/corticosteroids, methotrexate, megestrol acetate, platinum compounds, cyclophosphamide, doxorubicin, interferon-alpha, valproic acid, cyclosporine, vitamin A, NSAIDS, estramustine, ifosfamide, radiotherapy, and combined chemotherapeutic regimens, were identified and described. Skeletal effects of hyperparathyroidism, vitamin D deficiency, gastrectomy, hypophosphatemia, and hyperprolactinemia resulting from cancer therapies were also described.
Discussion/Conclusions
The publications researched during this review both highlight and emphasize the association between cancer therapies, including chemotherapy and radiotherapy, and skeletal dysfunction.
Implications for cancer survivors
These studies confirm that cancer survivors experience a more rapid acceleration of bone loss than their age-matched peers who were never diagnosed with cancer. Further studies are needed to better address the skeletal needs of cancer survivors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer survivors have become an important component of mainstream society, as nearly 4% of the United States population has been diagnosed with cancer and survived [1]. Following great innovations in therapy and detection, the number of cancer survivors has grown to more than 10.8 million individuals. Therapy regimens used to treat cancer have undergone tremendous change over the past four decades, and adjuvant chemotherapy and hormone therapy have become more widely used. Toxic chemotherapeutic drugs, radiotherapy, surgery, hormone therapy, and tumor activity itself may result in undesired long-term effects, including cardiovascular, neurologic, integumentary, pulmonary, musculoskeletal, gastrointestinal, and endocrinologic problems.
In recognition of the challenges facing cancer survivors, the Institute of Medicine and the National Research Council released recommendations for long-term follow-up care and research in this field [2]. The Life After Cancer Care (LACC) program at The University of Texas M. D. Anderson Cancer Center was established to study the long-term health profiles of cancer survivors and to develop recommendations for their health care. Several studies on the long-term health effects of cancer survivors have been published by the LACC team [3–12].
One of the most prevalent long-term health effects in cancer survivors is bone loss, including osteoporosis and osteomalacia. Osteoporosis is a systemic skeletal disorder defined by low bone mineral density and deterioration of the bone tissue microarchitecture, which may result in an increased propensity to fracture [13, 14]. It has been recognized as a major health threat for an estimated 44 million Americans, or 55% of people 50 years of age and older. In the United States, at least 10 million people have osteoporosis, and an additional 34 million are estimated to have low bone mass, placing them at increased risk for osteoporosis [15, 16] . Of the 10 million people estimated to have osteoporosis, 80% are women. Osteopenia is defined as bone mineral density (BMD) values between 1 and 2.5 standard deviations (SD) below the young adult mean value. Osteoporosis reflects BMD values more than 2.5 SD below the young adult mean value, and severe osteoporosis includes BMD values more than 2.5 SD below the young adult mean value in the presence of one or more fragility fractures [17].
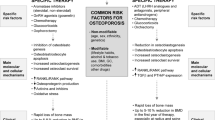
Osteomalacia is a condition defined by incomplete mineralization of bone structure [13], otherwise known as softening of the bones. There are several groups of survivors who have been recognized to be at particularly high risk for osteoporosis. Women with breast cancer treated with cytotoxic chemotherapy frequently experience early menopause and cannot receive estrogen replacement therapy. Men with prostate cancer who are on antiandrogenic therapy and become hypogonadal are at equivalent risk for developing osteoporosis. A third group at risk for bone loss is patients with lymphoma, myeloma, or leukemia. The common mechanisms shared by these groups include the production of bone-resorbing cytokines secreted by neoplastic cells and the use of high-dose glucocorticoids in treatment regimens [18]. A number of other drugs can induce osteoporosis, including methotrexate and various cytotoxic drugs that cause renal loss of calcium, magnesium, or phosphorous (e.g., platinum compounds, cyclophosphamide, and ifosfamide). These agents can have significant impact on bone density, especially at high dosages [18]. In most cases, it is undetermined whether bone loss in cancer survivors stems directly from the therapy itself, from the underlying disease process (including the impact of cachexia, malnutrition, and poor calcium and vitamin D intake), or from a combination of the two [19]. In addition to hormone therapy and cytotoxic drugs, radiation therapy and surgical castration can lead to loss of bone density [20].
Accelerated loss of bone mineral density, with consequential complications of pain, risk of compression, and pathological and traumatic fractures, becomes more important with increased duration of survival [21]. Disease-related skeletal complications are associated with shorter overall survival and a decreased quality of life [22].
The health effects reported by cancer survivors are numerous, but medical research and published literature on the topic are scarce, especially for adult survivors. Published literature on the risk, incidence, and detection of cancer treatment-induced bone loss in survivors of cancers other than breast or prostate cancer remains limited [16]. Most studies of cancer treatment-induced bone loss focused on survivors of childhood cancers. Those studies show varied, sometimes conflicting, results, and it is, therefore, challenging for researchers to reach explicit conclusions.
This review focuses on the skeletal sequelae of cancer and cancer treatments in survivors of pediatric and adult cancers. We conducted an intensive and current search using several medical Internet search engines, including PubMed, Medline Plus, Scopus, and Google Scholar. Since we wanted to focus on skeletal effects of cancer and cancer therapies, our criteria included search terms such as osteoporosis, osteomalacia, effects of cancer therapies, drug-induced skeletal disorders, effects of hormone replacement therapies, and skeletal effects of endocrine disorders. We excluded effects of bone metastases and skeletal effects of endocrine disorders not attributed to cancer therapies.
One-hundred-forty-two publications, mostly journal articles, met the inclusion criteria and were used for this review. The following analysis chronicles the many skeletal complications experienced by cancer survivors and observed in clinical studies.
Hypogonadism
The primary cause of cancer treatment-induced bone loss in both men and women survivors is hypogonadism induced by chemotherapy, irradiation, hormone therapy, or surgical castration [20]. Osteoporosis stemming from hypogonadism is frequently seen in survivors of breast and prostate cancer, as therapeutic hypogonadism is an important strategy for controlling these hormone-dependent tumors [23]. The risk of osteoporosis induced by hypogonadism is not limited to survivors of these cancers, however. Bone loss has been observed in lymphoma survivors who received therapy regimens including corticosteroids, alkylating agents, and radiation therapy, all of which can cause hypogonadism [13, 16]. Bone loss was also observed in patients made hypogonadic by cytotoxic drugs used in hematopoietic stem cell transplantations as part of their treatment regimens for certain cancers [24].
Researchers began highlighting the association between estrogen deficiency and lower bone mass in postmenopausal women as early as 1941 [25]. Estrogen deficiency, either due to menopause or surgical castration, can lead to increased osteoclastic bone resorption resulting in significant bone loss [13, 26]. The association between hypogonadism and osteoporosis has been more extensively studied in women than in men. Approximately 20% of men with spinal osteoporosis have hypogonadism [27], but the exact mechanism by which hypogonadism causes bone loss in men treated for prostate cancer is less clear. However, in hypogonadal prostate cancer patients, decreased circulating testosterone and estrogen levels cause a decrease in osteoblastic bone formation and an increase in osteoclastic bone resorption, resulting in accelerated bone loss [16]. (Table 1)
Chemotherapy-induced menopause and hypogonadism
Chemotherapy-induced menopause has been determined to be a more important cause of osteoporosis than the direct effects of cytotoxic agents and glucocorticoids [19]. Cytotoxic drugs used as adjuvant therapy for breast cancer may induce ovarian failure, which can ultimately hasten loss of bone mineral density in postmenopausal patients. Permanent ovarian failure was observed following individual therapeutic doses of cyclophosphamide, L-phenylalanine mustard, busulfan, chlorambucil, and mitomycin-C. Bines et al. reported that cyclophosphamide is the most common agent implicated in chemotherapy-related amenorrhea and that premature menopause was dependent on its cumulative dose [28].
The use of chemotherapy for prostate cancer is usually reserved in cases of advanced or recurring prostate cancer and studies on its effect on bone density are limited. However, chlorambucil and cyclophosphamide taken individually have been observed to cause prolonged azoospermia in male patients [29]. In addition, gonadal toxicity was evident in patients, especially those with testicular cancer, receiving a cumulative dose of cisplatinum greater than 400 mg/m2 [30]. The effects of cyclophosphamide and cisplatinum on bone will be discussed later in this review.
Radiation-induced hypogonadism
Both female and male cancer survivors who received irradiation to the cranium [29, 31], ovaries, or testes have displayed hypogonadism [20, 27, 32–35]. Daniell et al. highlighted the association between male hypogonadism and osteoporosis through reports of fractures occurring after external-beam radiation therapy to the prostate bed for prostate cancer [27, 34]. An older report by Grigsby et al. also demonstrated hypogonadism following radiation to the prostate bed [36].
Hormone treatment-induced hypogonadism
Treatment regimens for metastatic or locally advanced nonmetastatic prostate cancer increasingly involve the use of hormone therapy such as androgen deprivation therapies (ADT; i.e., bilateral orchiectomy, leuprolide, and other GnRH analogues). ADT induces severe hypogonadism characterized by loss of libido, impotence, gynecomastia, reduction of muscle mass, and loss of bone mineral density [23]. The most common type of ADT is the use of gonadotropin-releasing hormone (GnRH) agonists [37, 38]. The use of ADTs, particularly GnRH agonists, instead of surgical castration as part of the treatment regimen for cancer has been and is preferred by a large number of patients, especially those with prostate cancer [39–43].
Direct effects of cancer therapies
Androgen deprivation therapy (ADT)
Like many hormone replacement therapies, ADT is used as a palliative agent rather than as a treatment to cure the cancer itself and is taken over an extended period of time. Numerous studies, including retrospective audits, have demonstrated the association between ADT and osteoporosis [14, 40, 43–47].
The rate of BMD loss that occurs with ADT is significantly greater (as much as 10-fold higher) than that due to normal aging or female menopause [16, 39]. Kiratli et al. reported a trend towards decreased hip BMD with increasing years of ADT; this increase was more dramatic in patients who had undergone surgical castration than in those receiving medical ADT [47].
GnRH analogues were reported in a study by Smith et al. [48] to be an independent risk factor for fracture and were associated with an increased risk of any clinical fractures, with an odds ratio of 1.13 (95% CI, 1.02–2.26, p = 0.024). Maillefert et al. reported reductions in bone density from 3% to as high as 10% after 18 months of therapy with GnRH agonists [49].
Homes-Walker et al. demonstrated that the frequency of fractures in prostate cancer patients was dependent on the number of doses of gonadotropin-releasing hormone received during the first 12 months after diagnosis of cancer and on the age of the patient [50]. GnRH analogues suppress the secretion of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) by the pituitary gland. These effects and hypoestrogenemia may result in decreased BMD and osteoporosis [51]. However, the review by McLeod et al. demonstrates that the mechanism of bone loss due to ADT in male survivors of cancer is not well understood. Theories include the absence of circulating testosterone, which bonds to androgen receptors on osteoblasts, mediating their proliferation, and reduced substrate for the peripheral conversion of testosterone to estrogen, which positively maintains bone mass [52].
Estrogen suppression
Aromatase inhibitors (AIs)
The most common estrogen suppressors used in the treatment of cancer are aromatase inhibitors (AIs). AIs do not exert estrogen agonist or antagonist activity; they can, however, cause bone loss by suppressing aromatase activity and interfering with the conversion of adrenal and other androgens to estrogen, thereby reducing both circulating and tissue levels of estrogen [16, 53]. A retrospective longitudinal analysis of a large cohort of patients with breast cancer determined that AIs were independently associated with a 27% increase in risk of bone loss and a 21% increase in clinical fractures, after controlling for age, comorbidities, income, geographic location, and health plan type [54].
Nonsteroidal (anastrozole and letrozole) and steroidal (exemestane) AIs may have different effects on bone. Exemestane has a structure similar to androstenedione, an androgen precursor. It is presumed to have more bone-protective qualities than anastrozole or letrozole because of the increased bone formation seen with androgen excess [23]. However, both types of AIs may result in similar degrees of bone loss regardless of whether they are steroidal or nonsteroidal. The overall effects of nonsteroidal versus steroidal AIs on bone health are controversial [55]. Osteoporosis was more frequent in patients receiving exemestane, but the fracture rate was only slightly higher than in those taking tamoxifen, and the difference did not reach statistical significance. A British study also found no statistically significant differences between the three agents in terms of effects on bone turnover markers in postmenopausal women [56].
Tamoxifen
Tamoxifen, a selective estrogen receptor modulator (SERM), has been shown to both cause and prevent bone loss, depending on the menopausal status of the woman. In premenopausal women with high estrogen levels, it works as a bone antagonist, whereas in postmenopausal women with low estrogen levels, it works as a bone agonist and seemingly protects against bone loss [57, 58].
Powles et al. determined that while tamoxifen treatment has been associated with a significant loss of BMD in premenopausal women, the effects of tamoxifen on bone actually have not been adequately studied in these women [59]. Many treatment regimens for breast cancer involve adjuvant therapy with aromatase inhibitors after two or three years of tamoxifen therapy, and measuring the effect of both therapies on bone health has posed challenges for researchers studying bone turnover because prior, or concurrent, administration of tamoxifen exerts a protective effect on bone in postmenopausal women treated with AIs.
Glucocorticoids, cytotoxic chemotherapy, and other agents
Glucocorticoids
The majority of therapeutic regimens for many hematopoietic based malignancies involve high-dose glucocorticoids, usually administered over extended periods of time. Glucocorticoids, which are often used as a pain adjuvant, palliative agent, antiemetic, or as part of the treatment, suppress the activity of osteoblasts and, therefore, reduce bone formation [20]. Prolonged exposure to corticosteroids is the third leading cause of osteoporosis, after loss of sex steroids and old age in the normal population [60]. Osteoporosis develops in approximately half of the patients on long-term treatment with glucocorticoids [13, 60]. In fact, the risk of fracture increases by 50–100% in recipients of oral corticosteroids [61, 62].
The mechanisms underlying the negative effects of glucocorticoids on bone include (i) direct inhibitory effects on osteoblast function, (ii) reduction in the production of estrogen and testosterone along with the inhibition of anabolic action of sex steroids, and (iii) enhanced effects of parathyroid hormone [62].
There appears to be a defined relationship between the rate of bone loss and the dose of corticosteroid drug. The risk of corticosteroid-induced osteoporosis increases as the cumulative corticosteroid dose increases [63].
Methotrexate
The association between methotrexate and bone loss was reported as early as 1970 in a study of children on long-term methotrexate therapy for acute leukemia [64], and several publications have since confirmed the association [65, 66]. The review by Pfeilschifter et al. documented incidences of skeletal fractures in leukemic children ranging from 12% to 45% [13]. Methotrexate increases bone resorption and suppresses matrix mineralization, which reduces bone formation [20, 67].
Megestrol acetate
Megestrol acetate, a progestational agent used to treat metastatic breast cancer and endometrial carcinoma, has been implicated in osteoporosis and fractures in some patients. Its glucocorticoid-like activity may lead to the development of osteoporosis as well as other comorbidities. Wermers et al. documented the first possible association between megestrol and osteoporosis in two patients. This finding suggested that megestrol, especially at higher doses, may negatively affect bone density and potentially be associated with bone loss and the development of fractures [68].
Platinum-based therapy regimens
Published literature on the effects of platinum-based therapy regimens on bone is limited and primarily focused on animal studies. Platinum compounds are often administered in conjunction with other cytotoxic agents, so it has been challenging for researchers to differentiate between their effects on bone turnover and those of other agents. Cisplatinum is known for its hypomagnesemic effects, which include cessation of bone growth with suppressed osteoblast activity, inhibited bone formation, and osteopenia [18, 69, 70]. A Welsh study concluded that exposure to 6-mercaptopurine and cisplatin was associated with a reduction in hip bone mineral content in children treated for acute lymphoblastic leukemia [71].
Cyclophosphamide
Besides its role in hypogonadism, cyclophosphamide suppresses bone formation and resorption by directly arresting the cell division of preosteoblasts and osteoclasts, which in turn, results in fewer osteoblasts and osteoclasts on the bone surface [13, 16, 20]. This mechanism was also observed in an older study involving rats [72]. At the time of Wang’s writing (1986), the long-term effects of cyclophosphamide on the human skeleton had not yet been determined [72]. While adjuvant taxane-containing regimens (e.g., AC [doxorubicin/cyclophosphamide] followed by paclitaxel) may elicit menopause, it remains unknown whether cyclophosphamide or the combination of a taxane and alkylating agent causes the loss of bone density [16].
Doxorubicin
Both in vitro studies and animal studies of doxorubicin have demonstrated that the agent inhibits the proliferation and differentiation of osteoblasts and selectively reduces the rate of bone formation by altering the interaction of parathyroid hormone with the osteoblast receptor [16, 20, 73, 74]. Studies demonstrating doxorubicin’s effect on bone’s biomechanical properties are limited [69].
Interferon-alpha
Interferon-alpha (INF-α), one of the earliest known cytokine agents, is used to treat certain cancers such as hematologic malignancies, especially hairy cell leukemia, and solid tumors. Treatment with this agent may suppress bone formation; however, the consequences of its effects on bone mass remain undetermined. The review by Pfeischifter et al. described that recombinant INF-α transformed the cellular functions of both osteoblastic and osteoclastic lineages [13]. Beresford et al. suggested that INF-α suppressed proliferation of normal human bone-derived cells but did not appear to enhance differentiation [75]. The majority of studies demonstrating interferon’s effects on bone were conducted in in vitro models, and the exact mechanism remains incompletely understood [76, 77]. However, some of the in vitro studies suggest that INF-α causes decreased bone turnover, with decreased resorption by osteoclasts but increased differentiation of osteoblasts [77].
Solis-Herruzo et al. observed severe osteoporosis in a patient treated with ribavirin plus interferon for a year. This was the first published report of the effect of this therapy on bone mineral metabolism [78]. Another study concluded that male patients treated with interferon for multiple sclerosis demonstrated a decrease in bone mineral density [79]. In contrast, Lehmann et al. reported a case in which INF-α was instrumental in reversing some of the osteoporotic effects brought about by systemic mast cell disease [80] whereas it was suggested that INF-α inhibited the accretion of mast cells in bone marrow.
Valproic acid
In addition to its role as a mood stabilizer and anti-convulsant, the role of valproic acid (valproate) as a histone-deacetylase inhibitor renders it cytotoxic to many different types of cancer, including multiple myeloma, glioma, and melanoma. Osteopenia and osteoporosis were often reported in patients with chronic mental illness treated with long-term valproate therapy [81]. Sato et al. found that 37% of patients on valproate for epilepsy displayed osteopenia [82]. Sixty-eight percent of patients receiving chronic treatment with valproate in a study showed either osteoporosis or osteopenia compared to 22% in the control group. Furthermore, the longer an individual was on valproate, the worse the bone health; at 6-month follow-up, all lumbar spine and femoral bone density measures had worsened [81].
The mechanism behind how valproate adversely affects bone microarchitecture remains unidentified [83]. Valproate has, however, been associated with reversible Fanconi syndrome, suggesting that valproate may cause renal tubular dysfunction with increased urinary loss of calcium and phosphorus, leading to decreased mineral substrates for bone formation [84].
Cyclosporine
The immunosuppressant cyclosporine has been shown to stimulate osteoclasts, suppress osteoblasts, and inhibit mineral apposition and bone formation rates [85]. It has been hard to pinpoint the actual role of cyclosporine in bone density because it is almost always used in conjunction with other agents, such as corticosteroids, that are known to induce bone loss. Severe bone loss is often experienced by patients who undergo allogeneic or autologous hematopoietic stem cell transplantation. While post-transplantation osteopenia was brought about in part by hypogonadism, which can be prevented by hormone replacement, glucocorticoids and cyclosporine appear to be major components of bone loss in recipients, as bone loss was shown to be dependent on both the glucocorticoid dose and duration of cyclosporine therapy [86, 87].
Furthermore, in renal transplant patients, histomorphometric studies demonstrated increased bone turnover and delayed repair of renal osteodystrophy, suggesting that the effect of cyclosporine on bone turnover is independent of corticosteroids [88]. In addition, a follow-up study of patients more than six years after allogeneic bone marrow transplantation demonstrated that increased bone turnover was mainly present in patients who took cyclosporine during treatment [89].
Vitamin A
Excessive intake of vitamin A or retinoic acid was shown to be effective in the treatment of certain cancers and is suspected of inducing osteoporosis in humans [90, 91], but data are limited. In multivariate analysis, retinol intake was negatively associated with bone mineral density. For every 1-mg increase in daily intake of retinol, risk for hip fracture increased by 68% [92].
Nonsteroidal anti-inflammatory drugs
There are conflicting reports on the effect of nonsteroidal anti-inflammatory drugs (NSAIDs) on bone health. NSAIDs, which are used in various cancer therapies, inhibit the production of prostaglandins that modulate bone metabolism. Most published studies on NSAIDs’ effects on bone were performed in uncontrolled settings or in animals. A study of ovariectomized rats on long-term indomethacin treatment demonstrated reduced lumbar vertebral bone mass and compressive strength [93]. In another study, Goodman et al. [94] reported that NSAIDs were associated with delayed fracture healing and bone growth in humans; however, these effects may be reversible after discontinuation of treatment. Van Staa et al. showed that regular NSAID users experienced a higher risk of fracture compared with non-NSAID controls [95]. A Japanese study demonstrated that 60% of women taking NSAIDs had BMD scores less than 80% of the nation’s age-matched mean values [96].
In contrast to most data highlighting the negative effect of NSAIDs on bone health, a cohort study suggested that the use of COX-2-selective NSAIDs with aspirin was associated with higher BMD levels in various skeletal sites in both men and women [97]. Likewise, Bauer et al. found that regular use of aspirin or NSAIDs may exert a modest but beneficial effect on BMD in postmenopausal women [98].
Estramustine
Estramustine, an estrogen derivative used in prostate cancer therapy regimens, has been reported to increase bone resorption and at the same time induce hypocalcemia, hypophosphatemia, secondary hyperparathyroidism, and osteomalacia [18, 99]. It has been suggested that estramustine owes part of its therapeutic action and toxicity to a high-dose estrogen effect. Citrin et al. confirmed that estramustine was associated with significant changes in calcium and phosphate metabolism similar to those previously observed with high-dose estrogen therapy [100]. It was suggested that castration resulted in increased bone turnover and decreased BMD, but these changes may be exacerbated by using estramustine phosphate rather than bicalutamide [101].
Ifosfamide
Ifosfamide, used in many different cancer therapeutic regimens, including those for solid tumors in children, induces more sex-hormone-independent negative effects on the skeletal system than any other alkylating agent [13]. The effects of ifosfamide on the skeletal and renal systems have been well studied in the pediatric population, but a dearth of literature exists on its effects in adults [102]. Toxic effects of ifosfamide include tubular damage (e.g., Fanconi syndrome) that leads to renal phosphate wasting, hypophosphatemia, and rickets/osteomalacia [18, 103, 104]. Other associations between hypophosphatemia and Fanconi syndrome resulting from cancer therapies and bone health will be discussed later in this review.
Radiotherapy
Skeletal effects of radiation therapy may include altered bone growth and damaged or necrotic osteoblasts, which can result in secondary or uncontrolled resorption of the bone matrix [105, 106]. Bone alterations or damages caused by radiation are called radiation osteitis and radiation osteonecrosis, or osteoradionecrosis [106]. The study by Williams et al., conducted in Britain [106], suggests that radiation damage to bone in children usually involves altered bone growth patterns, wherein radiation affects the immature skeleton by disrupting the chondrogenesis and reabsorption of calcified cartilage. The authors of that study also reported that in adult skeletons, radiation may result in decreased matrix formation resulting from affected osteoblasts. However, Hopewell did not find a direct association between local radiotherapy to bone and reduced bone density in childhood cancer patients, even though the review documented other investigations that suggested reduced bone mineral density and increased fragility in mature bone [107].
Risk factors for developing radiation-associated fractures include radiation doses higher than 3,000 cGy, high-energy radiation beams, and underlying osteoporosis, especially in postmenopausal patients [105]. The effect of radiation therapy is dependent on the field of radiation, as cranial, rib, and pelvic irradiation each may result in different lingering effects.
Cranial irradiation has been studied as a prominent cause of osteopenia [13], and osteopenia was observed amongst 26 long-term survivors of cancer who were treated with cranial irradiation [108]. Therapy for tumors requiring radiation to the cranium, including acute lymphoblastic leukemia and nasopharyngeal carcinomas, can often inhibit the secretion of growth hormone and gonadotropins, which may result in hypogonadism. However, depending on the age at which treatment was received, hypopituitarism brought about by radiation can result in lack of skeletal growth and reduced BMD [109]. The mandible is particularly vulnerable to the effects of radiation, and osteoradionecrosis may occur within a year of treatment [106, 110]. As mentioned in this review, gonadotropin deficiency has been observed in patients treated with cranial irradiation, and subsequent hypogonadism may affect bone mineral density.
The literature suggests that radiation to the chest area for breast cancer and other cancers, including Hodgkin’s lymphoma, can result in radiation osteotitis involving the ribs, clavicles, and scapulae [107, 111, 112]. Pierce et al. determined that among a cohort of 1624 patients treated with irradiation for early-stage breast cancer, 1.8% experienced rib fractures an average of 12 months after treatment [113]. However, a Danish study demonstrated that 19% of post-mastectomy patients treated with a large dose per fraction of radiation experienced bone damage between one and six years after treatment [114].
Pelvic irradiation for ovarian/cervical cancer and prostate cancer is a common predisposing factor for sacral and femoral neck fractures [110, 115]. Bonfiglio [115] reported back in 1953 that femoral neck fractures were observed in 2% of cervical cancer patients who received orthovoltage radiation therapy. Another study published in 1981 reported several cases of slipped upper femoral epiphysis among childhood cancer patients treated with pelvic irradiation [116]. The effects of pelvic irradiation on bones, including demineralization and osteopenia, may develop following one year after therapy, and the effects may be progressive [117]. Bone changes resulting from pelvic irradiation may not be a direct consequence of the radiation itself but rather an indirect effect of radiation-induced hypogonadism.
Combination regimens
Combination therapy regimens can also exert negative effects on bone. As mentioned previously, it has been a challenge for researchers to study the toxicity of individual agents because most cancer treatments are administered as multi-agent regimens. Determining the actual incidences of skeletal damage for individual cancer therapies is often not possible because most protocols contain multiple agents and are subject to frequent revisions, and studies involving large numbers of patients and long-term follow-up remain scarce. In childhood cancer patients, van Leeuwen et al. concluded that it was difficult to distinguish the effect of one single agent on the growing skeleton [118]. However, some combination adjuvant chemotherapy regimens (including regimens with 5-fluorouracil, cyclophosphamide, and doxorubicin or methotrexate) have been associated with low bone mass [18].
Effect of age
While bone loss and osteoporosis are common signs of advancing age, survivors of cancer may experience bone loss at a more accelerated rate than their age-matched controls. Estrogen and androgen production decreases with age, and most anti-cancer therapeutic regimens leave cancer patients with little or no remaining estrogen and/or androgen. If these levels are not increased by ongoing estrogen replacement therapy, the patient’s rate of bone loss will rapidly accelerate with age. The Women’s Health Initiative Observational Study showed that female survivors of breast cancer had a 15% higher rate of all fractures, regardless of treatment received, than age-matched women without any history of cancer [119]. The rate of bone loss in a study of prostate cancer survivors was nearly 10-fold greater than that reported for a group of age-matched healthy elderly men [39].
Indirect effects of cancer therapies
It has been noted in this review that chemotherapy, irradiation, and hormone therapy may indirectly affect the skeleton through the mechanism of hypogonadism. There are, however, other indirect effects on bone health that result from cancer therapies. These effects include hyperparathyroidism, hypovitaminosis D, hypophosphatemia/Fanconi syndrome, gastrointestinal complications, and hyperprolactinemia.
Hyperparathyroidism
Hyperparathyroidism has long been associated with osteoporosis in which the parathyroid hormone (PTH) activates osteoblasts, which in turn matures the osteoclasts. Osteoclasts release hydrochloric acid, which dissolves bone mineral, causing osteopenia and osteoporosis [120, 121]. Incidences of secondary hyperparathyroidism associated with glucocorticoid intake have been demonstrated variably in both human and animal studies. The review by Reid showed that in some studies, patients receiving long-term glucocorticoid therapy exhibited PTH levels 50–100% higher than those of control subjects [122]. On the other hand, Pearce et al. [63] could not determine an effect of hyperparathyroidism on bone amongst a cohort of men treated with prednisolone to reduce antisperm antibodies.
Nonetheless, the role of hyperparathyroidism on bone mineral density in patients who have undergone organ transplantation, including autologous stem cell transplantation, has not been fully studied [123]. Heaf et al. concluded that ongoing hyperparathyroidism was a major cause of bone loss after renal transplantation [124]. In the review by Conde et al. [14] corticosteroid-related hypocalcemia directly stimulates PTH secretion, which can lead to increased osteoclastic bone resorption. Immunosuppressive therapy involving cyclosporine and tacrolimus can both directly and indirectly influence bone health, resulting in secondary hyperparathyroidism and increased bone resorption [125].
Radiotherapy has been associated with hyperparathyroidism, but few studies have been published on its effect on bone density [126–128]. In a study of patients with radiation-associated hyperparathyroidism, mean lumbar spine bone mineral density was found to be lower in women whose hyperparathyroidism was induced by radiation than in women with no history of radiation exposure [129].
Vitamin D deficiency
Hypovitaminosis D, or vitamin D deficiency, can lead to alterations in calcium intake and phosphorous homeostasis, secondary hyperparathyroidism, osteomalacia, and osteoporosis, as well as an increase in fracture risk [43, 50, 79, 130–133]. The association between hypovitaminosis D and high-dose or long-term glucocorticoid therapy has been pointed out in recent studies [134, 135]. Fifteen percent of a cohort of patients treated with bone marrow transplantation displayed hypovitaminosis D more than five years after treatment [87], and associated secondary hyperparathyroidism leading to increased bone turnover was evident in these patients.
Hypophosphatemia
Varying degrees of hypophosphatemia, with associated changes in bone and mineral metabolism, have been observed in up to 45% of patients taking tyrosine kinase inhibitors such as imatinib, sunitinib, and sorafenib [136–140]. However, Grey et al. suggested that hypophosphatemia from imatinib use resulted from secondary hyperparathyroidism [137]. One suggested explanation for the abnormalities in bone and mineral metabolism seen in patients taking imatinib is that the drug itself affects the formation and resorption of bone by inhibiting the platelet-derived growth factor receptor [138].
Hypophosphatemia, due to vitamin D deficiency and secondary hyperparathyroidism or primary renal tubular defects with phosphate wasting, is the most common cause of osteomalacia [103]. Hypophosphatemic osteomalacia has been reported among prostate cancer patients, which suggests that prostate cancer itself may be a cause of tumor-induced osteomalacia [100].
Osteomalacia resulting from hypophosphatemia associated with Fanconi syndrome has been observed in patients [103], and that study suggested that cisplatin and ifosfamide were well-recognized etiologies of the syndrome. Ifosfamide has been a well-recognized risk factor for Fanconi syndrome, and tubular damage was most commonly associated with doses of ifosfamide greater than 50 g/m2 and with concurrent use of cisplatin [19, 102, 103].
Gastrectomy
Patients who undergo gastrectomy for gastric carcinoma may develop osteoporosis or osteomalacia [141–144]. A German study documented that the overall rate of vertebral fractures or osteopenia in a cohort of post-gastrectomy patients was as high as 55% [142]. It has been suggested that patients who undergo gastrectomy may experience hypocalcemia and low vitamin D levels because their intake of dairy products is limited and essential nutrients are malabsorbed as a result of the adverse effects of the surgery, which may result in bone loss, and ultimately, fracture [142, 144, 145]. A recently published study conducted in Korea confirmed a high rate of osteoporosis amongst patients with gastric adenocarcinoma following gastrectomy [146].
Hyperprolactinemia
Hyperprolactinemia and subsequent central hypogonadism have been associated with the development of osteoporosis [147–150]. Hyperprolactinemia caused by prolactinomia in women influences bone metabolism unfavorably, primarily owing to the impact on the activity of bone turnover markers [151].
Cranial irradiation for brain malignancies may result in hyperprolactinemia, as dopamine released from the cellular damage and degeneration of the hypothalamus is unable to inhibit prolactin secretion from the pituitary gland. Hyperprolactinemia can be observed following radiotherapy doses of greater than 40 Gy [150] and is more common in young women [152, 153]. In one study, seven of eight patients who received chemotherapy including carmustine, vincristine, and methotrexate concurrent with radiotherapy for brain malignancies exhibited hyperprolactinemia [150].
Conclusions
This is a descriptive and inclusive review of scientific literature on bone and mineral metabolic disorders to which cancer survivors are prone. This review demonstrates that dysfunctions of the skeletal system are amongst the adverse effects of anti-cancer therapy. Some effects may not develop immediately after completion of therapy, and may be compounded with advancing age. Bone loss that occurs with cancer therapy is generally more rapid and severe than postmenopausal bone loss in women or normal age-related osteoporosis in men.
Bone recovery is poor once bone loss has occurred. Therefore early intervention is crucial to improving outcomes as osteoporosis therapy, or bone maintenance therapy, is most effective at preventing deterioration of bone.
The American Society of Clinical Oncology (ASCO) in 2003 established evidence-based guidelines for clinicians for the treatment of cancer-treatment-induced bone loss in patients with breast cancer. However, guidelines still do not exist for survivors of other cancers who are experiencing bone loss, including men who survived prostate cancer. At the time of this writing, no consensus statement or societal recommendation exists advising clinicians which men should receive therapy. The lack of guidelines for survivors of cancers other than breast cancer is due, in part, to the dearth of published evidence on cancer survivorship and its follow-up strategies [2]. As of 2004, there have been 374 PubMed citations on adult cancer survivorship research compared to 23,736 citations on adult cancer treatment research [2]. However, there has been a recent surge in published studies on bone loss caused by anti-cancer therapies, and it is with hope that successful follow-up strategies will encourage more guidelines on treatment-induced bone loss in survivors of other cancers such as prostate and ovarian cancer, multiple myeloma, and other hematologic malignancies. One of the recommendations issued by the Institute of Medicine in 2005 was to refine existing guidelines on the late effects of cancer and its treatment, and to develop new ones [154]. In fact, in 2005, one of the topics that ASCO assigned several panel subgroups was to study osteoporosis in long-term cancer survivorship. Hopefully the findings from the subgroups will be published in the near future [154].
As indicated in this review, further studies on cancer treatment-induced bone loss to answer these questions and to help clinicians better address the skeletal needs of cancer survivors are highly encouraged. Studies that isolate the effects of cancer and its treatments from the effects of normal aging on bone will be extremely useful. Hopefully with new cancer survivorship programs established at various referral cancer centers, researchers will be able to follow survivors over even longer periods of time. In the meantime until appropriate guidelines are developed, clinicians and other health care providers who treat cancer survivors should: (1) be aware of the patient’s full treatment history and exposure to cytotoxic agents, (2) identify the potential side effects of treatment agents/regimens, (3) identify other common risk factors not related to their treatments such as aging, family history of osteoporosis, lack of estrogen replacement therapy, a previous history of fractures, and others that may suggests an increased risk for bone loss, (4) provide diligent surveillance of patients’ bone density evaluation and measurements of kidney, liver, and thyroid function studies, a complete evaluation of mineral metabolism including serum measurements of parathyroid hormone, vitamin D metabolites, calcium, phosphate, albumin, and markers of bone turnover, and other hormones such as testosterone in men, (5) educate the individual patient on how to prevent bone loss and fractures by having adequate dietary calcium and vitamin D intake, sun exposure, exercise, prevention of falls, and the elimination of important risk factors for osteoporosis such as alcohol abuse and smoking, and (6) finally, if necessary, refer the patient to a cancer survivorship clinic.
References
NCI.SEER Cancer Statistics Review, 1975–2005. 2007; Available from: http://seer.cancer.gov/csr/1975_2005/.
Hewitt MGS, Stovall E. From cancer patient to cancer survivor, lost in transition. 1st ed. Washington, DC: National Academies; 2006.
Schultz PN, Beck ML, Stava C, Vassilopoulou-Sellin R. Health profiles in 5836 long-term cancer survivors. Int J Cancer. 2003;104(4):488–95. doi:10.1002/ijc.10981.
Schultz PN, Klein MJ, Beck ML, Stava C, Sellin RV. Breast cancer: relationship between menopausal symptoms, physiologic health effects of cancer treatment and physical constraints on quality of life in long-term survivors. J Clin Nurs. 2005;14(2):204–11. doi:10.1111/j.1365-2702.2004.01030.x.
Schultz PN, Stava C, Beck ML, Vassilopoulou-Sellin R. Ethnic/racial influences on the physiologic health of cancer survivors. Cancer. 2004;100(1):156–64. doi:10.1002/cncr.11897.
Schultz PN, Stava C, Vassilopoulou-Sellin R. Health profiles and quality of life of 518 survivors of thyroid cancer. Head Neck. 2003;25(5):349–56. doi:10.1002/hed.10217.
Stava C, Beck M, Schultz PN, Vassilopoulou-Sellin R. Hearing loss among cancer survivors. Oncol Rep. 2005;13(6):1193–9.
Stava C, Beck M, Vassilopoulou-Sellin R. Cataracts among cancer survivors. Am J Clin Oncol. 2005;28(6):603–8. doi:10.1097/01.coc.0000175291.51232.48.
Stava C, Beck M, Weiss LT, Lopez A, Vassilopoulou-Sellin R. Health profiles of 996 melanoma survivors: the M. D. Anderson experience. BMC Cancer. 2006;6:95. doi:10.1186/1471-2407-6-95.
Stava C, Weiss LT, Vassilopoulou-Sellin R. Health profiles of 814 very long-term breast cancer survivors. Clin Breast Cancer. 2006;7(3):228–36. doi:10.3816/CBC.2006.n.034.
Stava CJ, Lopez A, Vassilopoulou–Sellin R. Health profiles of younger and older breast cancer survivors. Cancer. 2006;107(8):1752–9. doi:10.1002/cncr.22200.
Stava C, Beck M, Feng L, Lopez A, Busaidy N, Vassilopoulou-Sellin R. Diabetes mellitus among cancer survivors. Journal of Cancer Survivorship. 2007;1:102–15.
Pfeilschifter J, Diel IJ. Osteoporosis due to cancer treatment: pathogenesis and management. J Clin Oncol. 2000;18(7):1570–93.
Conde FA, Aronson WJ. Risk factors for male osteoporosis. Urol Oncol. 2003;21(5):380–3. doi:10.1016/S1078-1439(03) 00109-1.
National Osteoporosis Foundation.Osteoporosis: Fast Facts. 2007; Available from: http://www.nof.org/osteoporosis/diseasefacts.htm.
Michaud LB, Goodin S. Cancer-treatment-induced bone loss, part 1. Am J Health-Sys Pharm. 2006;63(5):419–30. doi:10.2146/ajhp050045.p1.
World Health Organization.Prevention and Management of Osteoporosis: Report of a WHO Scientific Group (Technical Report Series 921). In A WHO Scientific Group on Prevention and Management of Osteoporosis. 2000. Geneva.
Yeung SC, Gagel RF. Endocrine complications. In: Holland JF, Bast Jr RC, Kufe DW, Pollock RE, Weischelbaum RR, editors. Cancer medicine. Hamilton, Ontario: BC Decker; 2000. p. 2389–98.
Yeung SC, Chiu AC, Vassilopoulou-Sellin R, Gagel RF. The endocrine effects of nonhormonal antineoplastic therapy. Endocr Rev. 1998;19(2):144–72. doi:10.1210/er.19.2.144.
Aksnes LH, Bruland OS. Some musculo-skeletal sequelae in cancer survivors. Acta Oncol (Stockholm, Sweden). 2007;46(4):490–6.
Ottery F. Issues in nutrition, weight and cancer. US Oncol Rev, 2005, 2004.
Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999;353(9156):878–82. doi:10.1016/S0140-6736(98)09075-8.
Hu MI, Gagel RF, Jimenez C. Bone loss in patients with breast or prostate cancer. Cur Osteoporos Rep. 2007;5(4):170–8.
Weilbaecher KN. Mechanisms of osteoporosis after hematopoietic cell transplantation. Biol Blood Marrow Transplantation. 2000;6(2A):165–74. doi:10.1016/S1083-8791(00)70039-5.
Albright F, Smith P, Richardson AM. Postmenopausal Osteoporosis. JAMA. 1941;116:2465–74.
Miyaura C. Mechanism of bone resorption induced by estrogen deficiency. J Bone and Miner Met. 1994;12(Suppl 2):S3–7. doi:10.1007/BF02383388.
Daniell HW. Osteoporosis after orchiectomy for prostate cancer. J Urol. 1997;157(2):439–44. doi:10.1016/S0022-5347(01)65165-6.
Bines J, Oleske DM, Cobleigh MA. Ovarian function in premenopausal women treated with adjuvant chemotherapy for breast cancer. J Clin Oncol. 1996;14(5):1718–29.
Meistrich ML, Vassilopoulou-Sellin R, Lipschultz L. Gonadal dysfunction: effects of cytotoxic agents on adult men. In: DeVita VT, Hellman S, Rosenberg SA, editors. Cancer: principles & practice of oncology. Philadelphia, PA: Williams & Wilkin; 1997. p. 2758–73.
Bokemeyer C, Berger CC, Kuczyk MA, Schmoll HJ. Evaluation of long-term toxicity after chemotherapy for testicular cancer. J Clin Oncol. 1996;14(11):2923–32.
Collet-Solberg PF, Sernyak H, Satin-Smith M, Katz LL, Sutton L, Molloy P, et al. Endocrine outcome in long-term survivors of low-grade hypothalamic/chiasmatic glioma. Clin Endocrinol (Oxf). 1997;47(1):79–85. doi:10.1046/j.1365-2265.1997.2211032.x.
Brydoy M, Fossa SD, Dahl O, Bjoro T. Gonadal dysfunction and fertility problems in cancer survivors. Acta Oncol (Stockholm, Sweden). 2007;46(4):480–9. doi:10.1080/02841860601166958.
Livesey EA, Brook CG. Gonadal dysfunction after treatment of intracranial tumours. Arch Dis Child. 1988;63(5):495–500. doi:10.1136/adc.63.5.495.
Daniell HW, Clark JC, Pereira SE, Niazi ZA, Ferguson DW, Dunn SR, et al. Hypogonadism following prostate-bed radiation therapy for prostate carcinoma. Cancer. 2001;91(10):1889–95. doi:10.1002/1097-0142(20010515)91:10<1889::AID-CNCR1211>3.0.CO;2-U.
Howell S, Shalet S. Gonadal damage from chemotherapy and radiotherapy. Endocrinol Metab Clin North Am. 1998;27(4):927–43. doi:10.1016/S0889-8529(05)70048-7.
Grigsby PW, Perez CA. The effects of external beam radiotherapy on endocrine function in patients with carcinoma of the prostate. J Urol. 1986;135(4):726–7.
Goldray D, Weisman Y, Jaccard N, Merdler C, Chen J, Matzkin H. Decreased bone density in elderly men treated with the gonadotropin-releasing hormone agonist decapeptyl (D-Trp6-GnRH). J Clin Endocrinol Metab. 1993;76(2):288–90. doi:10.1210/jc.76.2.288.
Garrett TJ, Vahdat LT, Kinne DW. Systemic adjuvant therapy of breast cancer. J Surg Oncol;. 1997;64(2):167–72. doi:10.1002/(SICI) 1096-9098(199702)64:2<167::AID-JSO16>3.0.CO;2-3.
Wei JT, Gross M, Jaffe CA, Gravlin K, Lahaie M, Faerber GJ, et al. Androgen deprivation therapy for prostate cancer results in significant loss of bone density. Urology. 1999;54(4):607–11. doi:10.1016/S0090-4295(99)00301-5.
Basaria S, Lieb J, Tang AM, DeWeese T, Carducci M, Eisenberger M, et al. Long-term effects of androgen deprivation therapy in prostate cancer patients. Clin Endocrinol (Oxf). 2002;56(6):779–86. doi:10.1046/j.1365-2265.2002.01551.x.
Mittan D, Lee S, Miller E, Perez RC, Basler JW, Bruder JM. Bone loss following hypogonadism in men with prostate cancer treated with GnRH analogs. J Clin Endocrinol Metab. 2002;87(8):3656–61. doi:10.1210/jc.87.8.3656.
Manni A, Santen R, Harvey H, Lipton A, Max D. Treatment of breast cancer with gonadotropin-releasing hormone. Endocr Rev. 1986;7(1):89–94. doi:10.1210/edrv-7-1-89.
Allain TJ. Prostate cancer, osteoporosis and fracture risk. Gerontology. 2006;52(2):107–10. doi:10.1159/000090956.
Diamond TH, Higano CS, Smith MR, Guise TA, Singer FR. Osteoporosis in men with prostate carcinoma receiving androgen-deprivation therapy: recommendations for diagnosis and therapies. Cancer. 2004;100(5):892–9. doi:10.1002/cncr.20056.
Shahinian VB, Kuo YF, Freeman JL, Goodwin JS. Risk of fracture after androgen deprivation for prostate cancer. N Engl J Med. 2005;352(2):154–64. doi:10.1056/NEJMoa041943.
Brown JE, Ellis SP, Silcocks P, Blumsohn A, Gutcher SA, Radstone C, et al. Effect of chemotherapy on skeletal health in male survivors from testicular cancer and lymphoma. Clin Cancer Res. 2006;12(21):6480–6. doi:10.1158/1078-0432.CCR-06-1382.
Kiratli BJ, Srinivas S, Perkash I, Terris MK. Progressive decrease in bone density over 10 years of androgen deprivation therapy in patients with prostate cancer. Urology. 2001;57(1):127–32. doi:10.1016/S0090-4295(00)00895-5.
Smith MR, Boyce SP, Moyneur E, Duh MS, Raut MK, Brandman J. Risk of clinical fractures after gonadotropin-releasing hormone agonist therapy for prostate cancer. J Urol. 2006;175(1):136–9. doi:10.1016/S0022-5347(05)00033-9. discussion 139.
Maillefert JF, Sibilia J, Michel F, Saussine C, Javier RM, Tavernier C. Bone mineral density in men treated with synthetic gonadotropin-releasing hormone agonists for prostatic carcinoma. J Urol. 1999;161(4):1219–22. doi:10.1016/S0022-5347(01)61639-2.
Holmes-Walker DJ, Woo H, Gurney H, Do VT, Chipps DR. Maintaining bone health in patients with prostate cancer. Med J Aust. 2006;184(4):176–9.
Makita K, Ishitani K, Ohta H, Horiguchi F, Nozawa S. Long-term effects on bone mineral density and bone metabolism of 6 months’ treatment with gonadotropin-releasing hormone analogues in Japanese women: comparison of buserelin acetate with leuprolide acetate. J Bone Miner Metab. 2005;23(5):389–94. doi:10.1007/s00774-005-0618-3.
McLeod N, Huynh CC, Rashid P. Osteoporosis from androgen deprivation therapy in prostate cancer treatment. Aust Fam Physician. 2006;35(4):243–5.
Ramaswamy B, Shapiro CL. Osteopenia and osteoporosis in women with breast cancer. Semin Oncol. 2003;30(6):763–75. doi:10.1053/j.seminoncol.2003.08.028.
Mincey BA, Duh MS, Thomas SK, Moyneur E, Marynchencko M, Boyce SP, et al. Risk of cancer treatment-associated bone loss and fractures among women with breast cancer receiving aromatase inhibitors. Clin Breast Cancer. 2006;7(2):127–32. doi:10.3816/CBC.2006.n.021.
Guise TA. Bone loss and fracture risk associated with cancer therapy. Oncologist. 2006;11(10):1121–31. doi:10.1634/theoncologist.11-10-1121.
McCloskey EV, Hannon RA, Lakner G, Fraser WD, Clack G, Miyamoto A, et al. Effects of third generation aromatase inhibitors on bone health and other safety parameters: results of an open, randomised, multi-centre study of letrozole, exemestane and anastrozole in healthy postmenopausal women. Eur J Cancer. 2007;43(17):2523–31. doi:10.1016/j.ejca.2007.08.029.
Fontanges E, Fontana A, Delmas P. Osteoporosis and breast cancer. Joint Bone Spine. 2004;71(2):102–10. doi:10.1016/j.jbspin.2003.02.001.
Love RR, Mazess RB, Barden HS, Epstein S, Newcomb PA, Jordan VC, et al. Effects of tamoxifen on bone mineral density in postmenopausal women with breast cancer. N Engl J Med. 1992;326(13):852–6.
Powles TJ, Hickish T, Kanis JA, Tidy A, Ashley S. Effect of tamoxifen on bone mineral density measured by dual-energy x-ray absorptiometry in healthy premenopausal and postmenopausal women. J Clin Oncol. 1996;14(1):78–84.
Shah SK, Gecys GT. Prednisone-induced osteoporosis: an overlooked and undertreated adverse effect. J Am Osteopath Assoc. 2006;106(11):653–7.
Cooper C, Coupland C, Mitchell M. Rheumatoid arthritis, corticosteroid therapy and hip fracture. Ann Rheum Dis. 1995;54(1):49–52. doi:10.1136/ard.54.1.49.
Adachi JD, Papaioannou A. Corticosteroid-Induced osteoporosis: detection and management. Drug Saf. 2001;24(8):607–24. doi:10.2165/00002018-200124080-00005.
Pearce G, Tabensky DA, Delmas PD, Baker HW, Seeman E. Corticosteroid-induced bone loss in men. J Clin Endocrinol Metab. 1998;83(3):801–6. doi:10.1210/jc.83.3.801.
Ragab AH, Frech RS, Vietti TJ. Osteoporotic fractures secondary to methotrexate therapy of acute leukemia in remission. Cancer. 1970;25(3):580–5. doi:10.1002/1097-0142(197003)25:3<580::AID-CNCR2820250313>3.0.CO;2-M.
Schwartz AM, Leonidas JC. Methotrexate osteopathy. Skeletal Radiol. 1984;11(1):13–6. doi:10.1007/BF00361126.
Athanassiadou F, Tragiannidis A, Rousso I, Katsos G, Sidi V, Papageorgiou T, et al. Bone mineral density in survivors of childhood acute lymphoblastic leukemia. Turk J Pediatr. 2006;48(2):101–4.
Crofton PM, Ahmed SF, Wade JC, Stephen R, Elmlinger MW, Ranke MB, et al. Effects of intensive chemotherapy on bone and collagen turnover and the growth hormone axis in children with acute lymphoblastic leukemia. J Clin Endocrinol Metab. 1998;83(9):3121–9. doi:10.1210/jc.83.9.3121.
Wermers RA, Hurley DL, Kearns AE. Osteoporosis associated with megestrol acetate. Mayo Clin Proc. 2004;79(12):1557–61. doi:10.4065/79.12.1557.
Van Leeuwen BL, Verkerke GJ, Hartel RM, Sluiter WJ, Kamps WA, Jansen HW, et al. Chemotherapy decreases epiphyseal strength and increases bone fracture risk. Clin Orthop Relat Res. 2003;413:243–54. doi:10.1097/01.blo.0000073348.50837.f2.
Von Hoff DD, Schilsky R, Reichert CM, Reddick RL, Rozencweig M, Young RC, et al. Toxic effects of cis-dichlorodiammineplatinum(II) in man. Cancer Treat Rep. 1979;63(9–10):1527–31.
Warner JT, Evans WD, Webb DK, Bell W, Gregory JW. Relative osteopenia after treatment for acute lymphoblastic leukemia. Pediatr Res. 1999;45(4 Pt 1):544–51. doi:10.1203/00006450-199904010-00014.
Wang TM, Shih C. Study of histomorphometric changes of the mandibular condyles in neonatal and juvenile rats after administration of cyclophosphamide. Acta Anat. 1986;127(2):93–9. doi:10.1159/000146262.
Mwale F, Ciobanu I, Demers CN, Antoniou J, Heon S, Servant N, et al. Amifostine and dexrazoxane enhance the rapid loss of bone mass and further deterioration of vertebrae architecture in female rats. Calcif Tissue Int. 2005;77(3):175–9. doi:10.1007/s00223-004-0231-9.
van Leeuwen BL, Hartel R, Jansen HW, Verkerke GJ, Veth RP, Kamps WA, et al. Chemotherapy affects the pattern of failure after shear loading of the proximal tibial growth plate. Arch Orthop Trauma Surg. 2004;124(8):503–6. doi:10.1007/s00402-004-0732-z.
Beresford JN, Taylor GT, Triffitt JT. Interferons and bone. A comparison of the effects of interferon-alpha and interferon-gamma in cultures of human bone-derived cells and an osteosarcoma cell line. Eur J Biochem. 1990;193(2):589–97. doi:10.1111/j.1432-1033.1990.tb19377.x.
Gur A, Dikici B, Nas K, Bosnak M, Haspolat K, Sarac AJ. Bone mineral density and cytokine levels during interferon therapy in children with chronic hepatitis B: does interferon therapy prevent from osteoporosis? BMC Gastroenterol. 2005;5:30. doi:10.1186/1471-230X-5-30.
Goodman GR, Dissanayake IR, Gorodetsky E, Zhou H, Ma YF, Jee WS, et al. Interferon-alpha, unlike interferon-gamma, does not cause bone loss in the rat. Bone. 1999;25(4):459–63. doi:10.1016/S8756-3282(99)00182-9.
Solis-Herruzo JA, Castellano G, Fernandez I, Munoz R, Hawkins F. Decreased bone mineral density after therapy with alpha interferon in combination with ribavirin for chronic hepatitis C. J Hepatol. 2000;33(5):812–7. doi:10.1016/S0168-8278(00)80314-1.
Perez Castrillon JL, Cano-del Pozo M, Sanz-Izquierdo S, Velayos-Jimenez J, Dib-Wobakin W. Bone mineral density in patients with multiple sclerosis: the effects of interferon. Rev Neurol. 2003;36(10):901–3.
Lehmann T, Beyeler C, Lammle B, Hunziker T, Vock P, Olah AJ, et al. Severe osteoporosis due to systemic mast cell disease: successful treatment with interferon alpha-2B. Br J Rheumatol. 1996;35(9):898–900. doi:10.1093/rheumatology/35.9.898.
Waheed A, Kettl PA. Low bone density with the use of valproate. Gen Hosp Psychiatry. 2005;27(5):376–8. doi:10.1016/j.genhosppsych.2005.03.008.
Sato Y, Kondo I, Ishida S, Motooka H, Takayama K, Tomita Y, et al. Decreased bone mass and increased bone turnover with valproate therapy in adults with epilepsy. Neurology. 2001;57(3):445–9.
Ecevit C, Aydogan A, Kavakli T, Altinoz S. Effect of carbamazepine and valproate on bone mineral density. Pediatr Neurol. 2004;31(4):279–82. doi:10.1016/j.pediatrneurol.2004.03.021.
Sheth RD, Wesolowski CA, Jacob JC, Penney S, Hobbs GR, Riggs JE, et al. Effect of carbamazepine and valproate on bone mineral density. J Pediatr. 1995;127(2):256–62. doi:10.1016/S0022-3476(95) 70304-7.
Cueto-Manzano AM, Konel S, Hutchison AJ, Crowley V, France MW, Freemont AJ, et al. Bone loss in long-term renal transplantation: histopathology and densitometry analysis. Kidney Int. 1999;55(5):2021–9. doi:10.1046/j.1523-1755.1999.00445.x.
Stern JM, Sullivan KM, Ott SM, Seidel K, Fink JC, Longton G, et al. Bone density loss after allogeneic hematopoietic stem cell transplantation: a prospective study. Biol Blood Marrow Transplant. 2001;7(5):257–64. doi:10.1053/bbmt.2001.v7.pm11400947.
Ebeling PR, Thomas DM, Erbas B, Hopper JL, Szer J, Grigg AP. Mechanisms of bone loss following allogeneic and autologous hemopoietic stem cell transplantation. J Bone Miner Res. 1999;14(3):342–50. doi:10.1359/jbmr.1999.14.3.342.
Sambrook PN. Cyclosporine and bone mass. Clin Exp Rheumatol. 2000;18(Suppl 21):S93–6.
Kerschan-Schindl K, Mitterbauer M, Fureder W, Kudlacek S, Grampp S, Bieglmayer C, et al. Bone metabolism in patients more than five years after bone marrow transplantation. Bone Marrow Transplant. 2004;34(6):491–6. doi:10.1038/sj.bmt.1704618.
Bannwarth B. Drug-induced musculoskeletal disorders. Drug Saf. 2007;30(1):27–46. doi:10.2165/00002018-200730010-00004.
Jackson HA, Sheehan AH. Effect of vitamin A on fracture risk. Ann Pharmacother. 2005;39(12):2086–90. doi:10.1345/aph.1G028.
Melhus H, Michaelsson K, Kindmark A, Bergstrom R, Holmberg L, Mallmin H, et al. Excessive dietary intake of vitamin A is associated with reduced bone mineral density and increased risk for hip fracture. Ann Intern Med. 1998;129(10):770–8.
Saino H, Matsuyama T, Takada J, Kaku T, Ishii S. Long-term treatment of indomethacin reduces vertebral bone mass and strength in ovariectomized rats. J Bone Miner Res. 1997;12(11):1844–50. doi:10.1359/jbmr.1997.12.11.1844.
Goodman SB, Jiranek W, Petrow E, Yasko AW. The effects of medications on bone. J Am Acad Orthop Surg. 2007;15(8):450–60.
van Staa TP, Leufkens HG, Cooper C. Use of nonsteroidal anti-inflammatory drugs and risk of fractures. Bone. 2000;27(4):563–8. doi:10.1016/S8756-3282(00)00361-6.
Kumaki SK. H. Effects of nonsteroidal anti-inflammatory drugs (NSAIDs) on osteoporosis. J Jpn Assoc Rural Med. 2001;50(2):96–101.
Carbone LD, Tylavsky FA, Cauley JA, Harris TB, Lang TF, Bauer DC, et al. Association between bone mineral density and the use of nonsteroidal anti-inflammatory drugs and aspirin: impact of cyclooxygenase selectivity. J Bone Miner Res. 2003;18(10):1795–802. doi:10.1359/jbmr.2003.18.10.1795.
Bauer DC, Orwoll ES, Fox KM, Vogt TM, Lane NE, Hochberg MC, et al. Aspirin and NSAID use in older women: effect on bone mineral density and fracture risk. Study of Osteoporotic Fractures Research Group. J Bone Miner Res. 1996;11(1):29–35.
Taube T, Kylmala T, Lamberg-Allardt C, Tammela TL, Elomaa I. The effect of clodronate on bone in metastatic prostate cancer. Histomorphometric report of a double-blind randomised placebo-controlled study. Eur J Cancer. 1994;30A(6):751–8. doi:10.1016/0959-8049(94)90287-9.
Citrin DL, Wallemark CB, Nadler R, Geiger C, Tuttle K, Kaplan EH, et al. Estramustine affects bone mineral metabolism in metastatic prostate cancer. Cancer. 1986;58(10):2208–13. doi:10.1002/1097-0142(19861115)58:10<2208::AID-CNCR2820581008>3.0.CO;2-A.
Yamada Y, Takahashi S, Fujimura T, Nishimatsu H, Ishikawa A, Kume H, et al. The effect of combined androgen blockade on bone turnover and bone mineral density in men with prostate cancer. Osteoporos Int. 2008;19(3):321–7. doi:10.1007/s00198-007-0472-3.
Church DN, Hassan AB, Harper SJ, Wakeley CJ, Price CG. Osteomalacia as a late metabolic complication of Ifosfamide chemotherapy in young adults: illustrative cases and review of the literature. Sarcoma. 2007. 91586.
Duck L, Devogelaer JP, Persu A, Berliere M, Caussin E, Baurain JF, et al. Osteomalacia due to chemotherapy-induced Fanconi syndrome in an adult patient. Gynecol Oncol. 2005;98(2):329–31. doi:10.1016/j.ygyno.2005.05.014.
Kintzel PE. Anticancer drug-induced kidney disorders. Drug Saf. 2001;24(1):19–38. doi:10.2165/00002018-200124010-00003.
Bluemke DA, Fishman EK, Scott WW Jr. Skeletal complications of radiation therapy. Radiographics. 1994;14(1):111–21.
Williams HJ, Davies AM. The effect of X-rays on bone: a pictorial review. Eur Radiol. 2006;16(3):619–33. doi:10.1007/s00330-005-0010-7.
Hopewell JW. Radiation-therapy effects on bone density. Med Pediatr Oncol. 2003;41(3):208–11. doi:10.1002/mpo.10338.
Vassilopoulou-Sellin R, Brosnan P, Delpassand A, Zietz H, Klein MJ, Jaffe N. Osteopenia in young adult survivors of childhood cancer. Med Pediatr Oncol. 1999;32(4):272–8. doi:10.1002/(SICI)1096-911X(199904) 32:4<272::AID-MPO6>3.0.CO;2-G.
Adler RA. Cancer treatment-induced bone loss. Curr Opin Endocrinol Diabetes Obes. 2007;14(6):442–5.
Mitchell MJ, Logan PM. Radiation-induced changes in bone. Radiographics. 1998;18(5):1125–36. quiz 1242–3.
Hirbe A, Morgan EA, Uluckan O, Weilbaecher K. Skeletal complications of breast cancer therapies. Clin Cancer Res. 2006;12(20 Pt 2):6309s–14. doi:10.1158/1078-0432.CCR-06-0652.
Iyer RB, Libshitz HI. Late sequelae after radiation therapy for breast cancer: imaging findings. AJR Am J Roentgenol. 1997;168(5):1335–8.
Pierce SM, Recht A, Lingos TI, Abner A, Vicini F, Silver B, et al. Long-term radiation complications following conservative surgery (CS) and radiation therapy (RT) in patients with early stage breast cancer. Int J Radiat Oncol Biol Phys. 1992;23(5):915–23.
Overgaard M. Spontaneous radiation-induced rib fractures in breast cancer patients treated with postmastectomy irradiation. A clinical radiobiological analysis of the influence of fraction size and dose-response relationships on late bone damage. Acta Oncol (Stockholm, Sweden). 1988;27(2):117–22. doi:10.3109/02841868809090331.
Bonfiglio M. The pathology of fracture of the femoral neck following irradiation. Am J Roentgenol Radium Ther Nucl Med. 1953;70(3):449–59.
Libshitz HI, Edeiken BS. Radiotherapy changes of the pediatric hip. AJR Am J Roentgenol. 1981;137(3):585–8.
Iyer RB, Jhingran A, Sawaf H, Libshitz HI. Imaging findings after radiotherapy to the pelvis. AJR Am J Roentgenol. 2001;177(5):1083–9.
van Leeuwen BL, Kamps WA, Jansen HW, Hoekstra HJ. The effect of chemotherapy on the growing skeleton. Cancer Treat Rev. 2000;26(5):363–76. doi:10.1053/ctrv.2000.0180.
Chen Z, Maricic M, Bassford TL, Pettinger M, Ritenbaugh C, Lopez AM, et al. Fracture risk among breast cancer survivors: results from the Women’s Health Initiative Observational Study. Arch Intern Med. 2005;165(5):552–8. doi:10.1001/archinte.165.5.552.
Holick MF. The vitamin D epidemic and its health consequences. J Nutr. 2005;135(11):2739S–48.
Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266–81. doi:10.1056/NEJMra070553.
Reid IR. Glucocorticoid-induced osteoporosis. Best Pract Res Clin Endocrinol Metab. 2000;14(2):279–98. doi:10.1053/beem.2000.0074.
Ria R, Scarponi AM, Falzetti F, Ballanti S, Di Ianni M, Sportoletti P, et al. Loss of bone mineral density and secondary hyperparathyroidism are complications of autologous stem cell transplantation. Leuk Lymphoma. 2007;48(5):923–30. doi:10.1080/10428190701268775.
Heaf J, Tvedegaard E, Kanstrup IL, Fogh-Andersen N. Hyperparathyroidism and long-term bone loss after renal transplantation. Clin Transpl. 2003;17(3):268–74. doi:10.1034/j.1399-0012.2003.00047.x.
Kulak CA, Borba VZ, Kulak Junior J, Shane E. Transplantation osteoporosis. Arq Bras Endocrinol Metabol. 2006;50(4):783–92. doi:10.1590/S0004-27302006000400023.
Rosen IB, Strawbridge HG, Bain J. A case of hyperparathyroidism associated with radiation to the head and neck area. Cancer. 1975;36(3):1111–4. doi:10.1002/1097-0142(197509)36:3<1111::AID-CNCR2820360341>3.0.CO;2-9.
Christmas TJ, Chapple CR, Noble JG, Milroy EJ, Cowie AG. Hyperparathyroidism after neck irradiation. Br J Surg. 1988;75(9):873–4. doi:10.1002/bjs.1800750914.
Ippolito G, Palazzo FF, Sebag F, Henry JF. Long-term follow-up after parathyroidectomy for radiation-induced hyperparathyroidism. Surgery. 2007;142(6):819–22. discussion 822 e1.
Kalaghchi B, Brietzke SA, Drake AJ 3rd, Shakir KM. Effects of prior neck radiation therapy on clinical features of primary hyperparathyroidism and associated thyroid tumors. Endocr Pract. 2003;9(5):353–62.
Alpert PT, Shaikh U. The effects of vitamin D deficiency and insufficiency on the endocrine and paracrine systems. Biol Res Nurs. 2007;9(2):117–29. doi:10.1177/1099800407308057.
Bandeira F, Griz L, Dreyer P, Eufrazino C, Bandeira C, Freese E. Vitamin D deficiency: A global perspective. Arq Bras Endocrinol Metabol. 2006;50(4):640–6.
Baker MR, McDonnell H, Peacock M, Nordin BE. Plasma 25-hydroxy vitamin D concentrations in patients with fractures of the femoral neck. Br Med J. 1979;1(6163):589.
Holick MF, Siris ES, Binkley N, Beard MK, Khan A, Katzer JT, et al. Prevalence of Vitamin D inadequacy among postmenopausal North American women receiving osteoporosis therapy. J Clin Endocrinol Metab. 2005;90(6):3215–24. doi:10.1210/jc.2004-2364.
Kinoshita Y, Masuoka K, Miyakoshi S, Taniguchi S, Takeuchi Y. Vitamin D insufficiency underlies unexpected hypocalcemia following high dose glucocorticoid therapy. Bone. 2008;42(1):226–8. doi:10.1016/j.bone.2007.09.042.
Cohran VC, Griffiths M, Heubi JE. Bone mineral density in children exposed to chronic glucocorticoid therapy. Clin Pediatr. 2008;47(5):469–75. doi:10.1177/0009922807311732.
Berman E, Nicolaides M, Maki RG, Fleisher M, Chanel S, Scheu K, et al. Altered bone and mineral metabolism in patients receiving imatinib mesylate. N Engl J Med. 2006;354(19):2006–13. doi:10.1056/NEJMoa051140.
Grey A, O’Sullivan S, Reid IR, Browett P. Imatinib mesylate, increased bone formation, and secondary hyperparathyroidism. N Engl J Med. 2006;355(23):2494–5. doi:10.1056/NEJMc062388.
Osorio S, Noblejas AG, Duran A, Steegmann JL. Imatinib mesylate induces hypophosphatemia in patients with chronic myeloid leukemia in late chronic phase, and this effect is associated with response. Am J Hematol. 2007;82(5):394–5. doi:10.1002/ajh.20778.
Rock EP, Goodman V, Jiang JX, Mahjoob K, Verbois SL, Morse D, et al. Food and Drug Administration drug approval summary: Sunitinib malate for the treatment of gastrointestinal stromal tumor and advanced renal cell carcinoma. Oncologist. 2007;12(1):107–13. doi:10.1634/theoncologist.12-1-107.
Kane RC, Farrell AT, Saber H, Tang S, Williams G, Jee JM, et al. Sorafenib for the treatment of advanced renal cell carcinoma. Clin Cancer Res. 2006;12(24):7271–8. doi:10.1158/1078-0432.CCR-06-1249.
Heiskanen JT, Kroger H, Paakkonen M, Parviainen MT, Lamberg-Allardt C, Alhava E. Bone mineral metabolism after total gastrectomy. Bone. 2001;28(1):123–7. doi:10.1016/S8756-3282(00)00404-X.
Zittel TT, Zeeb B, Maier GW, Kaiser GW, Zwirner M, Liebich H, et al. High prevalence of bone disorders after gastrectomy. Am J Surg. 1997;174(4):431–8. doi:10.1016/S0002-9610(97) 00123-2.
von Tirpitz C, Reinshagen M. Management of osteoporosis in patients with gastrointestinal diseases. Eur J Gastroenterol Hepatol. 2003;15(8):869–76. doi:10.1097/00042737-200308000-00006.
Imawari M, Kozawa K, Akanuma Y, Koizumi S, Itakura H, Kosaka K. Serum 25-hydroxyvitamin D and vitamin D-binding protein levels and mineral metabolism after partial and total gastrectomy. Gastroenterology. 1980;79(2):255–8.
Bisballe S, Eriksen EF, Melsen F, Mosekilde L, Sorensen OH, Hessov I. Osteopenia and osteomalacia after gastrectomy: interrelations between biochemical markers of bone remodelling, vitamin D metabolites, and bone histomorphometry. Gut. 1991;32(11):1303–7. doi:10.1136/gut.32.11.1303.
Naliato EC, Farias ML, Braucks GR, Costa FS, Zylberberg D, Violante AH. Prevalence of osteopenia in men with prolactinoma. J Endocrinol Invest. 2005;28(1):12–7.
Lim JS, Kim SB, Bang HY, Cheon GJ, Lee JI. High prevalence of osteoporosis in patients with gastric adenocarcinoma following gastrectomy. World J Gastroenterol. 2007;13(48):6492–7. doi:10.3748/wjg.13.6492.
Vartej P, Poiana C, Vartej I. Effects of hyperprolactinemia on osteoporotic fracture risk in premenopausal women. Gynecol Endocrinol. 2001;15(1):43–7. doi:10.1080/713602650.
Shibli-Rahhal A, Schlechte J. The effects of hyperprolactinemia on bone and fat. Pituitary. 2008.
Constine LS, Rubin P, Woolf PD, Doane K, Lush CM. Hyperprolactinemia and hypothyroidism following cytotoxic therapy for central nervous system malignancies. J Clin Oncol. 1987;5(11):1841–51.
Zadrozna-Sliwka B, Bolanowski M, Kaluzny M, Syrycka J. Bone mineral density and bone turnover in hyperprolactinaemia of various origins. Endokrynol Pol. 2007;58(2):116–22.
Sklar CA, Constine LS. Chronic neuroendocrinological sequelae of radiation therapy. Int J Radiat Oncol Biol Phys. 1995;31(5):1113–21. doi:10.1016/0360-3016(94)00427-M.
Darzy KH, Shalet SM. Hypopituitarism as a consequence of brain tumours and radiotherapy. Pituitary. 2005;8(3–4):203–11. doi:10.1007/s11102-006-6042-4.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stava, C.J., Jimenez, C., Hu, M.I. et al. Skeletal sequelae of cancer and cancer treatment. J Cancer Surviv 3, 75–88 (2009). https://doi.org/10.1007/s11764-009-0083-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-009-0083-4