Abstract
Introduction
The impact of cancer on people’s working lives is an increasingly important concern, yet, little is known regarding return to work after cancer in England. The rate of cancer patients who returned to paid employment within 18 months of diagnosis, and explored associations with demographic, clinical and work perception in one English region was investigated.
Materials and methods
A postal survey of all cancer patients registered in North West England from June 2002 through December 2002. Participants were between the ages 18–55 with a primary diagnosis of cancer, in paid employment at the time of diagnosis and being judged by their General Practitioners as suitable for return to work.
Results
Two hundrd sixty-seven eligible patients returned a completed consent form and questionnaire, a response rate of 50%. The median age was 48 years. The majority of respondents (48%) were female with breast cancer, followed by colorectal (14%), prostate (9%) and lung cancers (6%). 82% of respondents returned to work. Treatment modality (absence of surgery) and the length of sick-leave were the only significant factors related to return to work (Odds Ratio 0.28 95% CI 0.08–0.94; Odds Ratio 1.68 95% CI .1.23–2.28). The median length of sickness absence was less than 6 months, longer in the most economically deprived quintile. One fifth of those who returned to work reported deterioration in job satisfaction and career prospects.
Conclusions
While a high proportion of respondents managed to return to their place of work 20% were not able to do so. The duration of sick leave absence was associated with more difficulties in returning to work. Despite the fact that males were more likely than females to take no sick leave, they were more likely to take longer periods of absence when they did (18 months and over). In addition, the length of sick leave was greatest in the most economically deprived group, and in those survivors of cancer diagnosis and treatment who did not receive surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Every year approximately 90,000 people of working age in England are diagnosed with cancer [1]. It is estimated that more than 500,000 people under the age of 65 have been diagnosed with cancer at some point in their working lives [2]. Given improvement in cancer treatment leading to higher survival rates with the increased incidence of cancer diagnoses [3] returning to paid work after cancer is increasingly important for individuals, employers and the society. The specific change in the Disability Discrimination Act to cover employment among those specifically diagnosed with cancer [4] along with the expected extension of working life in Britain are two recent social changes that justify investigation of return to work in cancer survivors in England [5].
In North America and Western Europe cancer type and treatment and length of absence from work are factors that have been associated with return to work [6, 7]. The number of months since the end of treatment, discretion over working hours or amount of work and a supportive work environment are factors associated with return to work while those employed in a physically demanding job is also an obstacle. Age and socio-demographic factors such as gender, income and marital status do not seem to be associated with return to work rates among those with cancer [8, 9]. Furthermore, studies have found that the lack of advice regarding return to work from health care providers was related to a loss of confidence when back at work, and financial and health insurance pressures were associated with the timing and manner of the return to work [10, 11].
It is also of interest to provide population health data on work in social systems that have different policies regarding the social welfare of cancer survivors. As is well known, the UK provides free health care services at the point of use on the basis of medical need rather than ability to pay. This is delivered through the largely tax-financed National Health Service [12].
However, in terms of sickness benefits, there is a considerable variation that is dependent on the employer and the worker’s earnings and duration of employment [13]. Larger employers tend to provide occupational sick pay that would typically offer a 6 month entitlement to full pay followed by a further 6 months on half-pay. This occupational system is underpinned by Statutory Sick Pay which employers are liable to pay to employees who qualify by earning more than the modest earnings floor of the National Insurance lower earnings limit.
When entitlement to Statutory Sick Pay is exhausted after 7 months, people who are unable to work because of illness are eligible for Incapacity Benefit that provides similarly modest levels of income maintenance until they are again able to work or reach the current state pension age of 60 for women and 65 for men [14]. Pension provision is a complex mixture of ‘pay-as-you go’ state pensions and funded private provision that broadly reflects people’s lifetime earnings. The state pension system provides relatively modest levels of income maintenance with employer-provided occupational pensions providing the most generous pension levels in retirement. These social welfare arrangements suggest that there is likely to be a financial incentive for cancer survivors to return to work promptly [9]. Given the limited research from the United Kingdom on return to work in cancer survivors, the aim of this study was to explore the rate and factors associated with return to paid employment within 18 months after a diagnosis of cancer in one English region.
Materials and methods
Recruitment of participants and data collection
Participants were recruited from those registered by the North Western Cancer Intelligence Service (a population-based cancer registry) based in Manchester, England. Patients were selected if they met the following eligibility criteria:
-
A diagnosis of any cancer from June 2002 through to December 2002;
-
Aged 18–55 years;
-
In paid employment at the time of diagnosis;
-
Known to be alive and having a reasonable chance to return to work.
Participants were contacted some 3 years after their initial diagnosis, in order to allow for the process of return to work to take place.
In order to minimise unnecessary distress to patients and their families and to exclude patients who were physically too unwell to consider getting back to work, ethics approval was granted on the condition that patients were approached through their General Practitioner (GP). GPs were asked to assist in verifying the suitability of participants based on the above criteria. Each GP received a list of names of potential participants. Based on their judgement, they were asked to mail the questionnaire and a consent form to patients who met the criteria. GPs were also asked to return a list of patients who did not meet the criteria indicating the reason(s) for those patients being considered unsuitable for the study. A reminder was sent to GPs who did not respond at the first request, after 2 months.
Research instrument
Participants were asked to complete a confidential, self-administered brief ten item questionnaire containing questions about their employment status before, during and after their cancer diagnosis. With the participants’ consent, clinical (i.e. cancer site and treatment) and demographic (i.e. age, gender, deprivation quintiles [national quintiles of the Index of Multiple Deprivation, 2004 [16]]) information was derived from the Cancer Intelligence Service database. Since information on disease stage at diagnosis was not systematically collected by the Cancer Intelligence Service it was not possible to include this information within the analysis.
Analysis
Prevalence of differences in employment status between the various demographic and clinical groups was tested for statistical significance using contingency tables and the Pearson Chi Squared test. Spearman’s and Cramer’s V tests were used to establish the strength of association between statistically significant chi square tests. Multivariable logistic regression analysis with the variable return to work and work life measures were also conducted. We could not include the variable cancer site as the number of possible categories was too large for meaningful comparisons to be made.
Results
Level of response
Of 500 GPs that were approached, 384 doctors treating 778 patients responded, making an initial response rate of 77%. Two hundred and thirty eight patients were judged to be unsuitable for the study by their GP. Of those, two fifths (97: 41%) were judged to be too unwell with a poor prognosis and/or depressed, another 89 (37%) were near the state pension age and have actually retired; there is no information for the remaining 52 patients in this group.
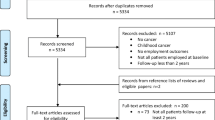
Two hundred and fifty six patients (47%) either did not respond or refused to participate. A total of 284 patients returned a completed questionnaire and consent form, of these, 267 were employed prior to diagnosis, an overall response rate of 50%. Figure 1 demonstrates response and employment status in the form of a flow chart.
Sample
The sample consisted of 267 participants. Gender was not evenly distributed with 71 (27%) males and 196 (73%) females. The sample age ranged from 19 to 55 years with a mean of 48 years. There were 33 cancer sites represented in the sample. The majority of respondents (127; 48%) were females with breast cancer, followed by colorectal (38; 14%), prostate (25; 9%) and lung (16; 6%) cancers (Table 1). Participants were relatively evenly split between deprivation quintiles. The largest group in the sample (77%) were respondents from white collar occupations (Table 2).
As depicted in Fig. 1, we were unable to contact 456 patients and an additional 256 patients did not respond. To address issues of potential sample bias, we extracted demographic and clinical data from the Cancer Intelligence Service, for those who the GP deemed unsuitable, those who refused consent, those who did not return the questionnaire and those who’s GP did not respond and compared it with the respondent group.
The respondents were similar demographically to the non-respondents; the median age was relatively similar; there were slightly fewer males among respondents than among those who the GP deemed unsuitable and those who did not return the questionnaire (28% to compare with 31 and 30%). Deprivation differed significantly between the groups, with more of the respondents in the two least deprived quintiles (40% compared with 39, 37, 30 and 29% ) and fewer in the two most deprived quintiles (38% compared with 38, 40, 44 and 53%). There were also significant differences in cancer site, with 48% of responders having breast cancers compared with 35% of those who the GP deemed unsuitable and 34% of those who did not return the questionnaire (Table 2).
Return to work (Univariate)
Two hundred and twenty respondents (82%) returned to work. Among those 213 received surgery (97%), with two thirds of these also receiving one or more of radiotherapy, chemotherapy or hormone therapy. A quarter of patients worked during their treatment. Table 3 presents the proportions of returning to work by gender, deprivation quintile, treatment modality and length of sick leave absence. Treatment modality was a statistically significant factor in return to work (p < 0.02) with the highest proportion of returnees among those who received surgery alone (93%) and the lowest in those who did not receive surgery (71%).
Statistically significant differences in return to work rates were also found by the length of sick leave taken, with more than 90% of those with sick leave duration of less than 12 months returning to work, compared with 62% with sick leave duration of 12 months or more. The majority (59%) of those who returned to work managed to do so within 6 months of diagnosis. However, 17% of those who were working before diagnosis were absent from work for more than 1 year. (p < 0.001)
There was no difference in return to work by gender, with small, non-significant, differences by deprivation quintile.
Return to work (Multivariable)
In order to identify the factors that were associated with return to work when accounting for the independent variables recorded, a multivariable logistic regression was conducted. All the independent variables (length of sick leave, gender, deprivation quintiles, cancer treatment or occupation) apart from cancer site were included in the analysis. The length of sick leave was found to be significant (odd ratio = 1.68 95% CI 1.23–2.28) and absence of surgery (odd ratio = 0.28 95% CI 0.08–0.94). (Table 4).
Length of sick leave absence
Table 5 presents the length of sick leave absence broken down by gender, deprivation quintile, treatment modality and occupation category among those who returned to work.
There was little difference between genders in those who took less than 6 months sick leave; however, females were nearly twice as likely to take 6–12 months sick leave compared with males (33.3% compared with 18.2%) and males were more than twice as likely to take long sick leave (1 year and over) than females (18.2%; 9.7%) (p < 0.05).
Length of sick leave differed by treatment modality (p < 0.001), with 83% of those who received surgery alone, returned to work in less than 6 months after diagnosis, compared with 47% of those who received surgery plus one or more of radiotherapy, chemotherapy or hormone therapy, and 40% in those who did not receive surgery, one quarter of whom were absent for more than 1 year.
Economic deprivation quintile was associated with length of sick leave; those in the highest quintile (1) were more likely to take less than 6 months sick leave (54.3%) compared with those in the lowest quintile (34.9%). Only one participant in the highest quintile took sick leave for 1 year and over compared with 25.6% (11) in the lowest quintile. However, those in the lowest quintiles (4&5) were slightly more likely to take no sick leave (30.4%) compared to those in the highest quintiles (18.7%) (p < 0.01).
Changes in work pattern
Eighty two percent of the sample remained in the same employment after returning to work, 8.3% changed to a different place of work while 9.5% stopped working altogether.
No significant differences were found between genders and economic deprivation quintiles. Nevertheless, there was a strong association between the length of sick leave and whether the participant returned to the same employer. Out of those with less than 6 months sick leave 94.5% returned to the same employer while of those with more than 18 months sick leave 71.4% only returned to the same employer. (X2 = 28.975, p < 0.000; Cramer’s V = 0.257, p < 0.000).
Similar patterns were found with hours worked after cancer treatment. The 83.2% of those taking less the 6 months sick leave are working the same hours compared to only 57.1% of those who took 18 months or more sick leave (x2 = 29.113, p < 0.000; Cramer’s V = 0.259, p < 0.000).
Perception of work
Over eighty percent (83.3%) of those who did not return to work reported that their overall working life had deteriorated as a result of their cancer, compared to only 19.4% of those who did return to work. (x2 = 36.848, p < 0.000).
Certain respondents who did not return to work viewed that as an improvement in their “working life.” The 14.3% of males who did not return to work considered their “working life” to have improved while no females considered that outcome as an improvement (Males x2 = 17.400, p < 0.000; Females x2 = 21.501, p < 0.000).
The number of hours worked after cancer diagnosis was cross tabulated with perceptions of working life to establish if changing work patterns or continuity were associated with positive or negative perceptions of work. Those who had to reduce the number of working hours due to their illness were more likely than those who worked the same hours to report that their working lives had deteriorated, 44.2%of those working fewer hours compared with 13.2% of those working the same hours. (x2 = 44.548, p < 0.000; Cramer’s V = 0.441, p < 0.000).
One fifth of those who returned to work and stayed in the same employment reported deterioration in their job satisfaction and career prospects, highest in those who took longer period of sick leave (p < 0.05).
Discussion
Little is known about people’s experiences of returning to work after cancer in Britain. Studies from North America and Western Europe have indicated that cancer type and treatment are associated with ability to return to work and that financial and health insurance pressures rather than medical advice can influence people’s work decisions [6–11].
In the present study, overall 82% of cancer patients, who were judged by their GPs as having reasonable chances of returning to work, did so. This finding compares favourably with previous evidence [9, 15, 19]. Furthermore, the strong association between treatment modality and the length of sick-leave with the rate of return to work was reported before [6, 7] The lack of association between age and gender and return to work [8, 9] is also consistent with prior research. The current study provides information on the actual process of returning to paid employment; changes in work patterns related to cancer and their perception of the quality of their working life after being diagnosed and treated for cancer in the British social system.
Since the variation in the length of sick leave was found to be strongly associated with the return to work, it is of prime importance to explore those variables explaining this variation. We found that gender has a significant role; despite the fact that males were more likely than females to take no sick leave at all, they were more likely to take longer periods of absence (18 months and over). Also the length of sick leave was greatest in the most deprived quintiles and with patients who did not receive surgery probably due to poor prognosis. Generally, lower levels of economic deprivation were associated with the length of sick leave, however, those in the lowest quintiles were slightly more likely to take no sick leave at all, which might be explained by strong financial needs to make an immediate return to paid employment.
As the State Pension Age is gradually increased over the next few decades it is likely that more people of working-age, particularly in their late fifties and sixties will be diagnosed with many types of cancer and expect (or need) to return to work. Therefore, it will be important to apply what we know about cancer and work in the context of developments in the labour market for older people and those in non-professional occupations.
The length of absenteeism was found to be associated with the actual outcome of this process-a shorter period of absence predicted a better continuity, in terms of returning to the same employer and working the same hours, which was positively viewed by the participants. This can be viewed either as continuity or as ‘job lock.’ It is beyond the ability of the current study to address this issue which warrants some further investigation.
Exploring participants’ views on their working life post cancer yielded interesting concerns. Generally achieving a return to work was positively viewed by many participants, however, nearly one fifth of those who returned to work reported deterioration in their job satisfaction and career prospects, with no significant differences between the genders and age groups. Conversely, there were a few differences between males and females who did not return to work. Males perceived the change in their working life in a more favourable way than females. These findings raise the question whether a return to work is a goal for all survivors. With the limitation of the current study this cannot be addressed, however, it would not be unexpected and important to explore whether return to work is a shared aim by everybody.
These findings need to be placed in the context of certain limitations. Although we were able to access the Cancer Intelligence Service data we were limited in our recruitment of participants through their GP who had the flexibility to exclude patients who were too ill. We were reliant on the judgment of patients’ GPs as to whether or not potential participants were suitable for the study and the resulting loss of patients to the study was considerable.
However, while the recruitment and response rates were lower than expected respondents were broadly representative of the sample population, who themselves were representative of the target population (that is cancer patients who survived at least 18 months after diagnosis and who were aged 18–55 at the time of diagnosis). There were some differences between the respondents and non-respondents, however. The greatest proportion among the respondents group was breast cancers. Given that the prognosis of breast cancer is generally better than for many other cancers, and the higher incidence rate of breast cancer among younger patients [18], this is consistent with expectations. Also recall bias might have been present however work status is a major aspect of function that we assumed most would recall accurately. Furthermore, cancer stage at diagnosis while important to help provide further explanation for return to work outcome was not provided for all participants and therefore we were unable to add disease severity to our analysis.
The findings reported in the current study together with the fact that the incidence of cancer is age-related, indicates a potentially vulnerable group of older people with non-professional occupations. It is reasonable to assume that return to work for this group of cancer patients is more difficult and less successful, as was previously reported [9]. It is therefore of prime importance to research the current experiences of this vulnerable group so that if return to work is a goal, legal protection and employer practices and procedures can be improved so this goal can actually be achieved.
More systematic research in this area is essential so we can develop evidence-based guidelines to support an increased participation in the labour market for an ever-growing population perhaps using concepts and approaches that have evolved from the study of work with other chronic illnesses [17]. Patterns of work, such as ‘under employment,’ ‘job instability’ and ‘re-entering the labour market’ (rather than remaining in the labour market) appear to be important research areas.
References
Office for National Statistics (2005). Cancer statistics registrations: Registrations of cancer diagnosed in 2003, England. Her Majesty’s Stationery Office: London. Accessed on 21/6/2006 from: http://www.statistics.gov.uk/downloads/theme_health/MB1_34/MB1_34.pdf.
Cancer Backup (2005). Work and cancer: How cancer affects working lives. London: Cancer Backup.
House of Commons, Committee of Public Accounts (2006). The NHS Cancer Plan: A progress report. The Stationery Office: London. Accessed on 28/6/2006 from: http://www.publications.parliament.uk/pa/cm200506/cmselect/cmpubacc/791/791.pdf.
Directory (2006). Definition of ‘disability’ under the Disability Discrimination Act. Accessed on 21/6/2006 from: http://www.direct.gov.uk/DisabledPeople/RightsAndObligations/YourRights/YourRightsArticles/fs/en?CONTENT_ID=4001069&chk=Bjab3%2B.
DWP (2006). Security in retirement: Towards a new pension system. Cm 6841. The Stationery Office: London accessed on 21/6/2006 from: http://www.dwp.gov.uk/pensionsreform/pdfs/white_paper_complete.pdf.
Farley Short, P., Vasey, J., & Tunceli, K. (2005). Employment pathways in a large cohort of adult cancer survivors. Cancer, 103, 1292–1301.
Bradley, C., Oberst, K., & Schenk, M. (2006). Absenteeism from work: The experience of employed breast and prostate cancer patients in the months following diagnosis. Psycho-Oncology, 15, 739–747.
Bradley, C. J., & Bednarek, H. L. (2002). Employment patterns of long-term cancer survivors. Psycho-Oncology, 11, 188–198.
Spelten, E., Sprangers, M., & Verbeek, J. (2002). Factors reported to influence the return to work of cancer survivors: A literature review. Psycho-Oncology, 11, 124–131.
Maunsell, E., Brisson, C., Dubois, L., Lauzier, S., & Fraser, A. (1999). Work problems after breast cancer: An exploratory qualitative study. Psycho-Oncology, 8, 467–473.
Main, D. S., Nowels, C. T., Cavender, T. A., Etschmaier, M., & Steiner, J. F. (2005). A qualitative study of work and work return in cancer survivors. Psycho-Oncology, 14, 992–1004.
McDonald, R. (2006). Creating a patient-led NHS: Empowering ‘consumers’ or shrinking the state? In L. Bauld, K. Clarke, & T. Maltby (Eds.), Social Policy Review 18: Analysis and debate in social policy (33–49). Bristol: Policy.
Alcock, P. (1999). Development of social security. In Introduction to social security: Policies, benefits and poverty (48–78). London: Routledge.
Directgov (2005). Benefits and financial support. Accessed on 14.3.2007 from: http://www.direct.gov.uk/en/Bfsl1/BenefitsAndFinancialSupport/DG_10018913.
Bouknight, R., Bradley, C., & Luo, Z. (2006). Correlates of return to work for breast cancer survivors. Journal of Clinical Oncology, 24(3), 345–352.
OPDM (2004). The English Indices of Deprivation. London: Office of the Deputy Prime Minister (OPDM).
Feuerstein, M. (2005). Cancer survivorship and work. Journal of Occupational Rehabilitation, 15(1), 1–2.
CRUK (2003). Numbers of new cases and age specific incidence rates by sex, breast cancer, UK. Accessed on 6.2.2007 from: http://info.cancerresearchuk.org/cancerstats/types/breast/incidence/.
Sanchez, K. M., Richardson, J. L., & Mason, H. R. (2004). The return to work experiences of colorectal cancer survivors. AAOHN Journal, 52(12), 500–510.
Acknowledgements
We are grateful to all participants who took part in this survey; Macmillan Cancer Support who funded the study; The North Western Cancer Intelligence Service; Janine Arnold for her support with the analysis and Sue Tizini for providing administrative support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Amir, Z., Moran, T., Walsh, L. et al. Return to paid work after cancer: A British experience. J Cancer Surviv 1, 129–136 (2007). https://doi.org/10.1007/s11764-007-0021-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-007-0021-2