Abstract
We herein report the case of a 62-year-old man who underwent extrapleural pneumonectomy (EPP) for pleural epithelial hemangioendothelioma (EHE) diagnosed by a pleural biopsy. Pre-operative computed tomography revealed diffuse pleural thickening and pleural effusion in the right thoracic cavity, although metastasis to neither the lymph nodes nor distant organs was detected. We decided to perform EPP based on surgical findings that the tumor had invaded the lung parenchyma. A pathological examination revealed tumor invasion of the lung parenchyma, blood vessel, pericardium, diaphragm and bronchial wall. Despite aggressive treatment, tumor recurrence was detected about 1 month after surgery. Although we controlled the tumor progression using pazopanib, the patient ultimately died 3.5 months after the operation. Pleural EHE is a very rare disease that has a poor prognosis due to its high malignant potential. It is important to formulate strategies matched to individual cases based on disease progression and invasiveness of treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pulmonary epithelioid hemangioendothelioma (EHE) was first reported in 1975 by Dali and Liebow [1]. The disease mostly occurs in soft tissues, lung, liver, and bone [2]. Among them, a number of pulmonary EHE cases have been reported in the past, typically occurring in women, and usually manifesting as bilateral parenchymal nodules, with a good prognosis [2]. The tumor has an intermediate malignant potential between benign hemangioma and angiosarcoma [3]. Pleural EHE is very rare, and only 30 cases have been reported so far. Pleural EHE is more aggressive than EHE derived from other organs and has a very poor prognosis. At present, no effective treatment methods have yet been established.
We herein report a case of pleural EHE that had a poor prognosis despite aggressive treatment.
Case
The patient was a 62-year-old man without asbestos exposure who complained of right chest pain and dyspnea on exertion. Right pleural effusion was noted on chest X-ray, so he was referred to our department. His medical history was unremarkable, except for the fact that he was a cigarette smoker (40 pack-year history).
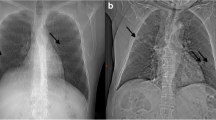
The value of pulse oximetry under room air was 96%, and laboratory findings showed mild inflammatory reaction elevation (white blood cells: 10000/μl, C-reactive protein: 2.04 mg/dl). Chest computed tomography (CT) showed diffuse pleural thickening and right pleural effusion (Fig. 1a, b), and invasion to the pulmonary parenchyma was strongly suspected. Fluorodeoxyglucose-positron-emission tomography (FDG-PET)/CT showed the diffuse accumulation of FDG (maximum standard uptake value [SUVmax] max 9.73) in the thickening right pleura (Fig. 1c). However, no lymphadenopathy or abnormalities of other organs were observed on imaging. Based on these clinical features, we suspected malignant pleural mesothelioma (MPM), so a right pleural biopsy was performed by thoracoscopy. We observed severe adhesion in the thoracic cavity.
In the pleural specimen, the pathological findings were different from MPM; polymorphonuclear to spindle-shaped cells with enlarged nucleus and deeply stained heteromorphism were observed, and individualized small massive proliferation of vascular endothelium-like lumen formation was also recognized (Fig. 2a). Based on immunohistologically findings that the tumor cells were negative for calretinin, diffusely but strongly positive for CD31 and CD34, and positive for CAMTA1 (Fig. 2b), the patient was diagnosed with pleural EHE with peripheral lung parenchymal invasion.
Pathological findings. a In the pleural specimen, polymorphonuclear to spindle-shaped cells with enlarged nucleus and deeply stained heteromorphism were observed, and individualized small massive proliferation of vascular endothelium-like lumen formation was also recognized. b Immunohistologically, the tumor cells were negative for calretinin, diffusely but strongly positive for CD31 and CD34, and positive for CAMTA1. c The surgical specimen revealed invasion of the lung parenchyma, blood vessel, and bronchial wall
An effective treatment for pleural EHE has not been established. Given that the lesion was confined to the thoracic cavity, we decided to perform surgical treatment as the first choice for pleural EHE. To preserve the pulmonary function, we initially planned to perform pleurectomy/decoritication (P/D). However, we instead performed extrapleural pneumonectomy (EPP) for the reasons shown below.
The surgical findings showed that the right lung was covered with a very thick pleura composed of many overlapping layers, and the tumor invaded the diaphragm and pericardium, which were regarded as indications of combined resection. In addition, infiltration was also noted in the lung parenchyma and the right main bronchial wall; we, therefore, chose to perform EPP instead of P/D. The operation time was 9 h and 42 min, and the amount of bleeding was 1830 cc. Heart failure occurred as a post-operative complication, but he recovered and was discharged on the 36th post-operative day.
A pathological examination revealed invasion of the lung parenchyma, blood vessels, pericardium, diaphragm and bronchial wall (Fig. 2c). However, despite aggressive treatment, tumor recurrence was confirmed a month after surgery. CT revealed chest wall thickening on the diseased side and ascites, and its cytology was malignant. Although we tried to control his disease progression using pazopanib, which is a molecular-targeted therapeutic agent, the patient ultimately died for respiratory failure due to poor control of pleural and ascites fluid 3.5 months after the operation.
Discussion
EHE is a rare malignant cancer of vascular origin, and EHE with pleural origin is extremely rare. Although pulmonary EHE usually progresses slowly with intermediate behavior, pleural EHE has an aggressive clinical course and a poor prognosis [3]. Salijevska et al. reported that pleural EHE cases showed significant heterogeneity in both presentation and management [4]. The mean age of pleural EHE cases was reported to be 45.7 years with a female/male ratio of 1:2.4 and a mean survival of 9.6 months. Because it is a rare disease, no standard treatment has yet been established, and whether or not surgical treatment is even effective is unclear.
Kim et al. and Yu et al. reported that survivors showed a disease-free period of more than 14 months by combining surgical treatment with chemotherapy, especially carboplatin and etoposide [5, 6]. However, Liu et al. reported a case in which, despite surgical treatment, the patient only survived 6 months [7]. Reports are thus quite conflicting, and many have described cases in which combination chemotherapy of carboplatin and etoposide was ineffective [8, 9].
In the present case, we selected surgical treatment, which is the only radical treatment, because the lesion was confined to the thoracic cavity. However, such an invasive surgery as EPP resulted in a reduced quality of life, and early regrowth was observed post-operatively. Considering that EHE tumor cells originate and proliferate from blood vessels, the resection margin for EPP and P/D in cases of pleural EHE may be insufficient. The blood flow to the parietal pleura is not only the blood flow in the pleura, but also perforating branches from the chest wall. Therefore, even if EPP is performed, it is considered that a microscopic tumor remains in the chest wall; it is all but impossible to perform microscopic complete resection, so tumor regrowth can consequentially occur. While surgery combined with chemotherapy seems essential for controlling disease progression of pleural EHE [5, 6], pleural EHE is not sensitive to chemotherapy. Indeed, we observed little efficacy of pazopanib in our case. Given the above, it is little wonder that establishing a standard therapy for pleural EHE has proven quite difficult.
No specific chemotherapy regimens for pleural EHE have yet been established. Previous reports have often applied a regimen using carboplatin and etoposide, but its efficacy remains unclear. Although no good treatment results have been reported so far, an effective treatment is still strongly desired. Bevacizumab, a vascular endothelial growth factor (VEGF) inhibitor, has been used to treat EHE, and relatively good results have been reported [10]. Furthermore, while we did not note its efficacy in our patient, there have also been reports that pazopanib, which is a second-generation tyrosine kinase inhibitor with high selective activity against VEGF receptor, is effective against EHE [11, 12]. The development of new agents in the future might improve the prognosis of pleural EHE.
Conclusion
Pleural EHE is a very rare disease and has a worse prognosis than EHE derived from other organs due to the difficulty of microscopic complete resection and chemotherapy resistance. Establishing a standard therapy for pleural EHE has proven difficult. It is important to formulate strategies matched to individual cases based on disease progression and invasiveness of treatment.
Abbreviations
- EHE:
-
Epithelioid hemangioendothelioma
- CT:
-
Computed tomography
- MPM:
-
Malignant pleural mesothelioma
- FDG-PET:
-
Fluorodeoxyglucose-positron-emission tomography
- SUV:
-
Standard uptake value
- P/D:
-
Pleurectomy/decortication
- EPP:
-
Extrapleural pneumonectomy
- VEGF:
-
Vascular endothelial growth factor
References
Dali DH, Liebow AA. Intravascular bronchioloalveolar tumor. Am J Pathol. 1975;78:6a–7a.
Crotty EJ, McAdams HP, Erasmus JJ, Sporn TA, Roggli VL. Epithelioid hemangioendothelioma of the pleura. Am J Roentgenol. 2000;175:1545–9.
Lee YJ, Chung MJ, Jeong KC, Hahn CH, Hong KP, Kim YJ, Kim YT. Pleural epithelioid hemangioendothelioma. Yonsei Med J. 2008;49:1036–40.
Salijevska J, Watson R, Clifford A, Ritchie AI, Mauri F, Adeboyeku D. Pleural epithelioid hemangioendothelioma: literature summary and novel case report. J Clin Med Res. 2015;7:566–70.
Kim EA, Lele SM, Lackner RP. Primary pleural epithelioid hemangioendothelioma. Ann Thorac Surg. 2011;91:301–2.
Yu L, Gu T, Xiu Z, Shi E, Zhao X. Primary pleural epithelioid hemangioendothelioma compressing the myocardium. J Card Surg. 2013;28:266–8.
Liu JX, Shiau MC, Nonaka D. An 80-year-old man with shortness of breath and large right-sided pleural effusion. Chest. 2010;138:1247–52.
Lazarus A, Fuhrer G, Malekiani C, McKay S, Thurber J. Primary pleural epithelioid hemangioendothelioma (EHE)—two cases and review of the literature. Clin Respir J. 2011;5:e1–5.
Andre ST, Valente C, Paiva B, Pego A, Carvalho L, Luis AS. Epithelioid hemangioendothelioma of the pleura—a rare presentation of a clinical case. Rev Port Pneumol. 2010;16:477–82.
Agulnik M, Yarber JL, Okuno SH, von Mehren M, Jovanovic BD, Brockstein BE, Evens AM, Benjamin RS. An open-label, multicenter, phase II study of bevacizumab for the treatment of angiosarcoma and epithelioid hemangioendotheliomas. Ann Oncol. 2013;24:257–63.
Schallier D, Berendes BJ, Lefesvre P, Everaert H. Effective treatment of pleural epithelioid hemangioendothelioma with pazopanib: a case report. Anticancer Res. 2016;36:351–4.
Semenisty V, Naroditsky I, Keidar Z, Bar-Sela G. Pazopanib for metastatic pulmonary epithelioid hemangioendothelioma—a suitable treatment option: case report and review of anti-angiogenic treatment options. BMC Cancer. 2015;15:402.
Funding
None
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Takenaka, M., Ichiki, Y., Nabe, Y. et al. Difficulty of treatment for pleural epithelioid hemangioendothelioma: a report of a case. Gen Thorac Cardiovasc Surg 68, 190–193 (2020). https://doi.org/10.1007/s11748-019-01135-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-019-01135-1