Abstract
Objectives
We retrospectively analyzed the prognostic significance of preoperative serum Krebs von den Lungen-6 (KL-6) level in non-small cell lung cancer (NSCLC) patients.
Methods
We enrolled 175 NSCLC patients who underwent curative surgery between 2009 and 2011. We subdivided the patients into 2 groups: with and without interstitial lung disease (ILD). Prognostic significance of serum KL-6 level was examined.
Results
The 5-year survival of patients with high serum KL-6 level was poor. Multivariate analysis also revealed the prognostic significance of serum KL-6 level. Serum KL-6 level was also a prognostic factor for patients without ILD. Although the number of patients with ILD was small, in patients with ILD, there was a trend towards an association between serum KL-6 level and patients’ prognosis but this did not reach statistical significance.
Conclusions
Serum KL-6 level is a prognostic factor for resected NSCLC patients, especially patients without ILD. There is a possibility that serum KL-6 level is a prognostic marker regardless of the presence of ILD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Krebs von den Lungen-6 (KL-6) is a high molecular weight glycoprotein classified as ‘‘Cluster 9 (MUC1)’’ of lung tumor and differentiation antigens according to the findings of immunohistochemical and flow cytometry studies [1, 2]. KL-6 is also known to be expressed in regeneration of type II pneumocytes [3] and has been reported to serve as a sensitive serum marker for interstitial lung disease (ILD) and is now clinically used to detect the presence of ILD [4, 5].
However, recent studies have suggested that it can also be used as a tumor marker as its origin shows [6]. Some previous studies also showed that serum KL-6 level is useful for predicting survival of non-small cell lung cancer (NSCLC) patients who have undergone curative surgery [7, 8]. It has been well accepted that the prognosis of NSCLC patients with ILD was poor [9, 10]. Since serum KL-6 level has been reported to serve as a sensitive serum marker for ILD, there is a possibility that the reason for poor prognosis of patients with high serum KL-6 level might be due to the presence of ILD. To our knowledge, only one study examined the prognostic significance of serum KL-6 level in NSCLC patients with or without ILD [11]. However, the ratio of patients who underwent surgery was only 27.4 % in their study population [11].
Therefore, in the present study, we also subdivided the patients into 2 groups: with and without ILD, and investigated the significance of serum KL-6 level in NSCLC patients who underwent curative surgery.
Patients and methods
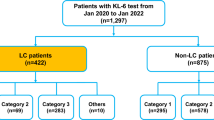
This retrospective study had institutional review board approval, and the need to obtain patient consent was waived. Consecutive NSCLC patients who underwent surgery from 2009 to 2011 in our hospital were enrolled in the present retrospective study. The following patients were excluded: (1) patients who had not received complete resection which consisted of either a lobectomy or a pneumonectomy together with the regional lymph nodes dissection, (2) patients who had not examined preoperative serum KL-6 level, (3) patients who died of other diseases after surgery, and (4) patients who lost to follow-up. One hundred and seventy-five consecutive resected NSCLC patients were enrolled in the present retrospective study. The clinicopathological factors of patients are shown in Table 1. The cutoff value of serum KL-6 was 500 U/mL. The time interval between preoperative serum KL-6 examination and surgical resection was less than 2 weeks in all the patients. The postoperative serum KL-6 level was also measured during 1–2 months after surgery for patient with preoperative high serum KL-6 level. Preoperative chest conventional or high-resolution computed tomography (HRCT) was evaluated to examine not only the extent of cancer but also the existence of ILD in all cases. ILD was defined by medical history, physical examination, and abnormalities compatible with bilateral lung fibrosis on chest computed tomography (CT) or HRCT, such as peripheral reticular opacities. When the chest CT, reviewed by radiologists, revealed such abnormalities, patients were referred to pulmonologists and the existence of ILD was evaluated preoperatively [12].
Pathological (p) tumor–node–metastasis (TNM) staging was recorded in all patients based on the 7th edition of the American Joint Committee on Cancer (AJCC)/Union for International Cancer Control (UICC) classification. Follow-up information, including cause of death, was ascertained through a review of clinical notes and direct or family contact. Comparisons of data between the two groups were made using Fisher’s extract test. The disease-specific survival curves of the patients were plotted using the Kaplan–Meier method and analyzed using the log-rank test. The Cox regression hazard model was used for univariate and multivariate analyses to assess the prognostic value of serum KL-6 level. Statistical calculations were conducted with JMP 12.2.0 (SAS Institute Inc., Cary, NC, USA) and values of p less than 0.05 were accepted as being significant.
Results
There were only 15 patients with high serum KL-6. The number of patients with ILD was also only 14 patients. As shown in Table 1, serum KL-6 level was significantly related with ILD and serum CEA level. However, age, gender, histology, smoking status, pStage, pT status and pN status were not.
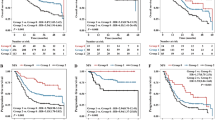
The postoperative disease-specific 5-year survival rates in patients with normal and high serum KL-6 level were 33.3 and 74.0 %, respectively (Fig. 1). This difference was significant (p < 0.0001).
The result of univariate analysis is summarized in Table 2. The gender, smoking status (never vs. former/current), histology (adenocarcinoma vs. others), pT status (pT1 vs. pT2–3), pN status (pN0 vs. pN1–2), serum CEA level (normal vs. high), serum KL-6 level (normal vs. high) and ILD (with vs. without) were related to patient prognosis. The result of multivariate analysis is also summarized in Table 3. The histology (adenocarcinoma vs. others), pN status (pN0 vs. pN1–2), serum CEA level (normal vs. high), serum KL-6 level (normal vs. high) and ILD (with vs. without) were related to patient prognosis.
In patients without ILD, serum KL-6 level was also a prognostic factor (40.0 vs. 77.2 %, p = 0.0047, Fig. 2a). On the other hand, in patients with ILD, there was a trend towards an association between serum KL-6 level and patients’ prognosis but this did not reach statistical significance (p = 0.063, Fig. 2b), although the number of patients with ILD was small.
For patients with preoperative high serum KL-6 level, postoperative serum KL-6 level was also examined. As shown in Fig. 3, the postoperative serum KL-6 levels of all but 1 patient had decreased.
Discussion
In the present study, we showed that serum KL-6 level is an independent prognostic factor in NSCLC patients. This result supports the hypothesis that KL-6 can serve as a prognostic biomarker for NSCLC although the number of patients with high serum KL-6 level was small. The prognostic roles of serum KL-6 level for various cancers, including pancreas, breast, colon, and hepatocellular carcinomas have been also reported previously [13–17].
KL-6 has been known to be expressed in regeneration of type II pneumocytes [3]. A question regarding whether the origin of serum KL-6 level of NSCLC patients is associated with tumors may be raised. Tanaka et al. [8] showed that serum KL-6 levels were found to decrease dramatically after surgical resection of primary tumors. Our result also showed that serum KL-6 levels decreased after surgical resection. Tanaka et al. [8] also reported that KL-6 was immunohistochemically detectable in all of the analyzed NSCLC tissues. These results strongly suggest that the primary tumor was the origin of serum KL-6 level in NSCLC patients.
The reason why serum KL-6 level can serve as a prognostic biomarker in NSCLC patients who undergo curative surgery has been unknown in detail. KL-6 is classified as a MUC1 mucin and Xu et al. [18] reported a result of a meta-analysis and concluded that MUC1 detection has a prognostic value in patients with epithelial-originated cancers, especially in NSCLC and gastrointestinal cancers. Furthermore, Nagai et al. [19] showed that MUC1 expression pattern was correlated with tumor differentiation and postoperative survival in NSCLC. Therefore, serum KL-6 level might reflect the degree of tumor aggressiveness at least in part.
In a review of several earlier studies, the overall frequency of ILD in lung cancer has been reported as approximately 2–3 % [20, 21], with some variation across studies. In our series, ILD was found in 8 % (14/175) of patients, and slightly higher than the frequency reported in previous studies. This might be due to the patients’ selection bias. Our study was limited to the patients who examined the serum KL-6 level preoperatively. Recently, we routinely examined the preoperative serum KL-6 level in all NSCLC patients, but we did not necessarily examine serum KL-6 level during the period of the present study.
It has been well accepted that the prognosis of NSCLC patients with ILD was poor [9, 10, 12]. We also showed the similar result. Sato et al. [10] retrospectively analyzed data from 1763 patients with NSCLC with a clinical diagnosis of ILD who underwent pulmonary resection between 2000 and 2009 at 61 Japanese institutions. They reported that the overall 5-year survival was 40 % and the 5-year survivals were 59, 42, 43, 29, 25, 17, and 16 % for patients with stage Ia, Ib, IIa, IIb, IIIa, IIIb, and IV, respectively [10]. Since serum KL-6 level has been reported to serve as a sensitive serum marker for ILD, there is a possibility that the reason for poor prognosis of patients with high serum KL-6 level might be due to the presence of ILD. However, our result of multivariate analysis showed the independent prognostic significance of serum KL-6 level. Therefore, serum KL-6 might have a role as a tumor marker in addition to serum marker for ILD.
In our results, serum KL-6 level was a prognostic marker in NSCLC patients without ILD. In other words, serum KL-6 level might play a role as a tumor maker in NSCLC patients without ILD. On the other hand, the evaluation of serum KL-6 level in NSCLC patients with ILD is difficult. When NSCLC patients with ILD have high serum KL-6 level, it is difficult to distinguish whether high serum KL-6 level means as an ILD marker or a tumor marker. Thus, we subdivided the patients into 2 groups: with and without ILD, and investigated the significance of serum KL-6 level in NSCLC patients. Although the number of NSCLC patients with ILD in the present study was small, there was a trend towards an association between serum KL-6 level and patients’ prognosis but this did not reach statistical significance in NSCLC patients with ILD. This might be due to the small number of NSCLC patients with ILD. Therefore, there is a possibility that serum KL-6 level is a prognostic marker regardless of the presence of ILD. Further studies in this area are warranted.
There were some limitations in the present study. The study was retrospective and the number of patients with high serum KL-6 level was small. There is a possibility that our data have no statistical meanings because of small number of patients. However, we showed a clear tendency of the association between KL-6 and patients’ prognosis. We believe that this result is meaningful. Therefore, a large cohort study will be required to confirm our results.
Conclusions
In conclusion, serum KL-6 level is a prognostic factor for resected NSCLC patients. Although the number of NSCLC patients with ILD in the present study was small, there was a trend towards an association between serum KL-6 level and patients’ prognosis in NSCLC with ILD. Therefore, there is a possibility that serum KL-6 level is a prognostic marker regardless of the presence of ILD.
References
Kohno N, Inoue Y, Hamada H, Fujioka S, Fujino S, Yokoyama A, et al. Difference in sero-diagnostic values among kl-6-associated mucins classified as cluster 9. Int J Cancer Suppl. 1994;8:81–3.
Stahel RA, Gilks WR, Lehmann HP, Schenker T. Third international workshop on lung tumor and differentiation antigens: overview of the results of the central data analysis. Int J Cancer Suppl. 1994;8:6–26.
Hirasawa Y, Kohno N, Yokoyama A, Inoue Y, Abe M, Hiwada K. Kl-6, a human muc1 mucin, is chemotactic for human fibroblasts. Am J Respir Cell Mol Biol. 1997;17:501–7.
Kohno N, Kyoizumi S, Awaya Y, Fukuhara H, Yamakido M, Akiyama M. New serum indicator of interstitial pneumonitis activity. Sialylated carbohydrate antigen kl-6. Chest. 1989;96:68–73.
Kohno N, Awaya Y, Oyama T, Yamakido M, Akiyama M, Inoue Y, et al. Kl-6, a mucin-like glycoprotein, in bronchoalveolar lavage fluid from patients with interstitial lung disease. Am Rev Respir Dis. 1993;148:637–42.
Inata J, Hattori N, Yokoyama A, Doi M, Ishikawa N, et al. Circulating kl-6/muc1 mucin carrying sialyl lewisa oligosaccharide is an independent prognostic factor in patients with lung adenocarcinoma. Int J Cancer. 2007;120:2643–9.
Shoji F, Yamazaki K, Kouso H, Mori R, Takeo S. Predictive impact for postoperative recurrence of preoperative serum Krebs von den Lungen-6 concentration in pathologic stage ia non-small cell lung cancer. Ann Thorac Surg. 2016;101:1903–8.
Tanaka S, Hattori N, Ishikawa N, Shoda H, Takano A, Nishino R, et al. Krebs von den Lungen-6 (kl-6) is a prognostic biomarker in patients with surgically resected nonsmall cell lung cancer. Int J Cancer. 2012;130:377–87.
Kawasaki H, Nagai K, Yoshida J, Nishimura M, Nishiwaki Y. Postoperative morbidity, mortality, and survival in lung cancer associated with idiopathic pulmonary fibrosis. J Surg Oncol. 2002;81:33–7.
Sato T, Watanabe A, Kondo H, Kanzaki M, Okubo K, Yokoi K, et al. Long-term results and predictors of survival after surgical resection of patients with lung cancer and interstitial lung diseases. J Thorac Cardiovasc Surg. 2015;149:64–9 (70.e1–2).
Miyazaki K, Kurishima K, Kagohashi K, Kawaguchi M, Ishikawa H, Satoh H, et al. Serum kl-6 levels in lung cancer patients with or without interstitial lung disease. J Clin Lab Anal. 2010;24:295–9.
Chiyo M, Sekine Y, Iwata T, Tatsumi K, Yasufuku K, Iyoda A, et al. Impact of interstitial lung disease on surgical morbidity and mortality for lung cancer: analyses of short-term and long-term outcomes. J Thorac Cardiovasc Surg. 2003;126:1141–6.
Ogawa Y, Ishikawa T, Ikeda K, Nakata B, Sawada T, Ogisawa K, et al. Evaluation of serum kl-6, a mucin-like glycoprotein, as a tumor marker for breast cancer. Clin Cancer Res. 2000;6:4069–72.
Xu H, Inagaki Y, Tang W, Guo Q, Wang F, Seyama Y, et al. Elevation of serum kl-6 mucin levels in patients with cholangiocarcinoma. Hepatogastroenterology. 2008;55:2000–4.
Kimura T, Tanaka S, Haruma K, Sumii K, Kajiyama G, Shimamoto F, et al. Clinical significance of muc1 and e-cadherin expression, cellular proliferation, and angiogenesis at the deepest invasive portion of colorectal cancer. Int J Oncol. 2000;16:55–64.
Yamasaki H, Ikeda S, Okajima M, Miura Y, Asahara T, Kohno N, et al. Expression and localization of muc1, muc2, muc5ac and small intestinal mucin antigen in pancreatic tumors. Int J Oncol. 2004;24:107–13.
Kurosaki M, Izumi N, Onuki Y, Nishimura Y, Ueda K, Tsuchiya K, et al. Serum kl-6 as a novel tumor marker for hepatocellular carcinoma in hepatitis c virus infected patients. Hepatol Res. 2005;33:250–7.
Xu F, Liu F, Zhao H, An G, Feng G. Prognostic significance of mucin antigen muc1 in various human epithelial cancers: a meta-analysis. Med (Balt). 2015;94:e2286.
Nagai S, Takenaka K, Sonobe M, Ogawa E, Wada H, Tanaka F. A novel classification of muc1 expression is correlated with tumor differentiation and postoperative prognosis in non-small cell lung cancer. J Thorac Oncol. 2006;1:46–51.
Kinoshita A, Hirose K, Taniguchi T, Soda H, Rikitake T, Tsurukawa Y, et al. [lung cancer associated with idiopathic interstitial pneumonia]. Nihon Kyobu Shikkan Gakkai Zasshi. 1990;28:852–8 (in Japanese).
Park J, Kim DS, Shim TS, Lim CM, Koh Y, Lee SD, et al. Lung cancer in patients with idiopathic pulmonary fibrosis. Eur Respir J. 2001;17:1216–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no conflict of interest exists.
Rights and permissions
About this article
Cite this article
Tomita, M., Ayabe, T., Chosa, E. et al. Prognostic significance of preoperative serum Krebs von den Lungen-6 level in non-small cell lung cancer. Gen Thorac Cardiovasc Surg 64, 657–661 (2016). https://doi.org/10.1007/s11748-016-0706-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-016-0706-4