Abstract
The incidence of spinal cord injury in thoracic endovascular aortic repair (TEVAR) has been 3–5 % from recent major papers where sacrifice of the critical intercostal arteries is inevitable by a stent graft. Hemodynamic stability, which depends on a network of blood vessels around the cord is most important not only during but also after stent-graft deployment. High risk factors of spinal cord injury during endovascular aortic repair are (1) coverage of the left subclavian artery, (2) extensive coverage of long segments of the thoracic aorta, (3) prior downstream aortic repair, (4) compromising important intercostal (T8–L1), vertebral, pelvic and hypogastric collaterals, and (5) shaggy aorta. Preoperative, intraoperative, and postoperative managements have been required to prevent spinal cord injury with TEVAR. For imaging assessment of blood supply to spinal cord including Adamkiewicz artery, prophylactic cerebrospinal fluid drainage is mandatory, and monitoring motor-evoked potential is recommended for high risk factors of spinal cord injury. Mean arterial pressure should be maintained over 90 mmHg after stent-graft placement for a while to prevent delayed spinal cord ischemia in high-risk patients of spinal cord ischemia. Finally, because spinal cord injury during TEVAR is not rare and negligible, perioperative care during TEVAR should be strictly performed according to the protocol proposed by each cardiovascular team.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thoracic endovascular aortic repair (TEVAR) has become a standard treatment on the descending aorta, which is a less invasive approach than open surgery and its availability and relative ease of application have changed and extended management options in thoracic aortic disease. However, spinal cord injury (SCI) can occur immediately or be delayed, requiring clinical and neurological surveillance after TEVAR when the critical intercostal arteries are inevitable to sacrifice. This review paper presents how to prevent SCI, representing mechanism of SCI.
Mechanism of spinal cord injury during thoracic endovascular aortic repair
Incidence
Generally, the incidence of SCI averaged 3–5 % with TEVAR. The incidence of paraplegia/paraparesis after TEVAR, compiled from the peer reviewed literature reporting at least 20 cases is listed in Table 1 [1–20]. There was a broad range in the incidence of SCI, with an average of 4.5 % in 7309 patients (range 0–10.3 %), not making this technique superior to the open surgical procedure. Although sacrificing the critical intercostal arteries is inevitable with TEVAR, hemodynamic stability during the procedure must be translated into a lower risk of paraplegia. Therefore, many cases in SCI with TEVAR have incomplete and delayed appearance as compared with open aortic surgery.
Mechanism
Normal blood flow at the gray matter of the spinal cord has been considered to be 100 ml/min/g; the critical point of tissue blood flow that causes tissue ischemia is assumed to be 20 ml/min/g. The inherited potential of the blood supply to the spinal cord depends on a network of blood vessels around the cord. Factors that increase the blood reserve of the spinal cord during the perioperative period for TEVAR on the descending or thoracoabdominal aorta are (1) an increased cardiac output, (2) increased blood pressure (3) avoidance of hypoxemia and anemia, (4) preservation of the critical intercostal arteries, and (5) reduced CSF pressure [21]. The largest series to date, reported by the European Collaborators on Stent/Graft Techniques for Aortic Aneurysm Repair investigators, cited left subclavian artery coverage without revascularization, concomitant abdominal aortic surgery, and the use of three or more stent grafts to be associated with SCI. These three clinical variables each have a well-established relationship to the blood supply of the spinal cord. Coverage of the left subclavian artery, for instance, compromises the proximal collateral circulation to the spinal cord, including the vertebral and internal thoracic arteries. Extensive coverage of long segments of the thoracic aorta using multiple stent grafts may also significantly limit spinal cord perfusion by compromising important intercostal (T7–L1) and lumbar segmental arteries supplying the anterior spinal artery [8, 9]. Prior AAA repair can similarly lead to diminished spinal cord perfusion by compromising pelvic and hypogastric collaterals [12, 22]. Moreover, degenerative aneurysms have been associated with an increased risk for SCI, given that these patients tend to have fewer patent intercostal arteries as compared to those with postdissection thoracic aneurysms. An atheroma with an irregular and speculated appearance is commonly called a “shaggy aorta” that may be related to shower embolization in TEVAR. Spinal cord injury is caused by shower embolism after TEVAR. High risk factors for spinal cord injury during TEVAR are as follows,
-
1.
Coverage of the left subclavian artery.
-
2.
Extensive coverage of long segments of the thoracic aorta (the length of coverage by stent graft ≥30 cm) [16 ].
-
3.
Prior downstream aortic repair.
-
4.
Compromising important intercostal (T8–L1), vertebral, pelvic and hypogastric collaterals.
-
5.
Shaggy aorta.
Hybrid operation using frozen or long elephant trunk technique
The rate of incidence of SCI after frozen elephant trunk (FET) was reported to be 8.2 % [23]. Spinal cord injury after FET is associated with the thoracic vertebral level where the distal end of the FET was deployed and intraoperative hypotension, similar to TEVAR. However, the incidence of SCI with FET is generally higher than that with TEVAR because of hemodynamic instability during the procedure. Recently frozen elephant trunk has not been recommended for complex pathologic condition requiring stent graft delivery lower than T9. Efficacy of cerebrospinal fluid drainage has been reported in frozen or long elephant trunk for patients who have high risk factors as previous mentioned.
Management for spinal cord injury during thoracic endovascular aortic repair
Ullery in Hospital of the University of Pennsylvania reported onset of SCI occurred at a median of 10.6 h (range 0–229 h) postprocedure and was delayed in 83 % (n = 10) of patients [17]. Management for spinal cord injury should be carried out sequentially before and under and after TEVAR considering the mechanism of blood supply to spinal cord.
Preoperative management
Imaging assessment
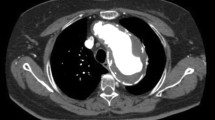
CT angiography is useful modality for diagnosis and planning treatment for TEVAR. It is necessary to plan the size of stent graft and to perform a risk evaluation of SCI in total by grasping having cited left s ubclavian artery coverage with revascularization or not and left vertebral artery probe patency and relations of a network to the blood supply of the spinal cord in CT, specially, important to identify the intercostal/lumber arteries that supply the Adamkiewicz artery (ICA–AKA). Matsuda reported that the estimated incidence of permanent and transient spinal cord injury was 3.7 % in all TEVAR patients, 6.0 % when part of or the entire distal aorta was covered and 12.5 % when the patent ICA–AKA was covered [16].
Prophylactic cerebrospinal fluid drainage
It is intended to maintain spinal cord return current by allaying cerebrospinal pressure by cerebrospinal fluid drainage. In high-risk patients with poor network to the blood supply of the spinal cord, preventive cerebrospinal fluid drainage (CSFD), which has proven efficacy in spinal cord protection during TEVAR similar to open thoracoabdominal aneurysm surgery, is strongly recommended [21]. However, we always must pay attention to the complications such as intracranial bleeding or a hematoma or meningitis in the spinal cord in 2–3 % with CSFD. In a recent review by Estera et al. [4] spanning 15 years and 1107 patients, CSF drain placement showed a technical success rate of 99.8 % and a drain-related complication rate of 1.5 %. Subdural hematoma developed in five patients (0.4 %); however, since implementing a limited CSF drainage protocol, this complication has not developed in any patients. Certain clinical situations may prevent the placement of a spinal drain, such as patients with symptomatic or ruptured thoracic aortic pathology or patients with prior lumbar spine surgery. Indications for placing a spinal drain, based on our current practice, are listed in Table 2.
Shaggy aorta
Shaggy aorta may be related to shower embolization in TEVAR. Spinal cord injury occurs caused by that shower embolism after TEVAR. Therefore, the shaggy aorta has recently been considered a contraindication for TEVAR. However, we sometimes must perform TEVAR to the atheromatous aorta with thickened wall on the descending aorta. Statins have been reported to have pleiotropic effects such as regression and stabilization of plaques in the aorta, similar to the coronary artery [24].
Operative strategies
In extended thoracic, thoracoabdominal aneurysm, two-stage operation has been considered to diminish risk of SCI. Especially in the case of TEVAR with abdominal debranching for TAAA, the interval between debranching procedure and TEVAR should be several weeks to have hemodynamic stability. Long elephant trunk or frozen elephant trunk for extended aneurysm has been not recommended. Two-stage TEVAR after upstream aortic replacement has been recommended for such pathologic condition that specially required stent graft delivery lower than T9.
Intraoperative management
Reconstruction of left subclavian artery (LSA) bypass
LSA should be reconstructed as much as possible as mentioned above because the coverage of LSA is one of the high risk factors of SCI. In particular, reconstruction of LSA is requisite for a case to have other SCI high risk factors with a long stent-graft treatment [25]. The procedure of reconstruction of LSA is reported in various ways. Generally a bypass the right axillary artery to the right axillary artery using a prosthesis graft is performed via bilateral subclavian incision. As an alternative procedure, there is the bypass to the left subclavian artery from a common left carotid artery via single incision on the left neck. The author prefers this approach because the bypass is short and is not over the midline neck. It is important to evaluate the communication between bilateral vertebra/basilar artery and the internal carotid artery before debranching bypass of neck arteries.
Maintenance of systemic blood pressure
The blood pressure maintenance after the stent-graft placement is important from a point of view where spinal cord ischemia during TEVAR greatly participates in the anterior spinal artery network. It is necessary to maintain low blood pressure when the stent graft is deployed with regard to migration of the stent graft. However, systemic blood pressure should be immediately augmented after being deployment and touch-up of stent graft. It is required to manage it so that mean blood pressure becomes more than 90 mmHg with vasopressors such as infusion load, correction of anemia and sometimes vasopressor medication [17].
Monitoring of SCI using measurement of motor-evoked potential during TEVAR
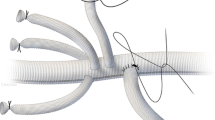
Motor-evoked potential (MEP) and somatosensory-evoked potential (SSEP) monitoring are established methods of spinal cord monitoring to evaluate spinal cord ischemia quantitatively during not only extensive thoracoabdominal aortic repair but also TEVAR [16]. In particular, MEP is effective in the case with having high risk factors. When MEP shows a drop after deployment of stent graft, we can deal with infusion load, anemia improvement, and the augmentation of blood pressure from an early stage (Figs. 1, 2) and become able to accomplish postoperative management strictly to prevent delayed SCI. Schurink reported the MEPs immediately decreased below 50 and 30 % in 2 patients of 12 after coverage of ICA–AKA by TEVAR, recovering to levels above 50 % by elevation of the mean arterial pressure. They concluded that monitoring of MEPs during TEVAR shows no decrease in most cases, but this can be reversed by elevation of the mean arterial pressure if a decrease of MEPs occurs [26].
Intraoperative monitoring of mean AP and MEP during TEVAR for high-risk patient of spinal cord ischemia—a typical case that MEP temporary decrease. Elective thoracic endovascular aortic repair using two stent grafts was performed zone 3 to T-12 (treatment length was 32 cm) with coverage of intercostal artery (T-10) that supplied the Adamkiewicz artery for 79-year woman who had extended thoracic aneurysm. Because myogenic motor-evoked potential (MEP) decreased by 60 % 15 min after deploying stent graft, cerebrospinal fluid drainage (CSFD) was open and mean arterial pressure (AP) was raised by volume overload and vasopressor medication
Management for atheromatous lesion during TEVAR
When we perform TEVAR to the atheromatous aorta with thickened wall on the descending aorta, we should avoid landing and touch-up to the atheromatous aorta as much as possible in performing TEVAR. Using a temporary AV shunt with a sieving device for an embolic protection has been reported in a TEVAR for shaggy aorta [27].
Postoperative management
Generally all patients should be taken care after TEVAR in an intensive care unit (ICU) for 24 h to manage hemodynamic state according to spinal protection protocol. The algorithm to manage the risk of spinal cord ischemia in patients undergoing TEVAR has been shown in Fig. 3. A focused neurologic assessment was performed on an hourly basis until recovery from anesthesia permitted a more thorough neurologic examination. Lower extremity motor function was classified according to the following modified Tarlov scale, ranging from 0 to 5: 0, no lower extremity movement; 1, motion without gravity; 2, motion against gravity; 3, able to stand with assistance; 4, able to walk with assistance; and 5, normal. Mean arterial pressure should be maintained over 90 mmHg after stent-graft placement for a while to prevent delayed spinal cord ischemia in high-risk patients of spinal cord ischemia. In patients receiving CFSD, cerebrospinal pressure is kept less than 10 mmHg, while the head of the bed (HOB) is ≤15°. When the HOB is >15°, we assess neurologic status prior to elevating the HOB. The drain remains in place for 24 h in an ICU, and is then removed. The utility of extending the duration of CSFD beyond 48 h diminishes over time because SCI episodes beyond 48 h are infrequent and risk of CSFD-related complications increases [12]. Reason for capping the drain 24 h before removal is to permit CSF pressure to normalize so as to ensure that SCI does not occur at normal CSF pressures and to prevent CSF hypotension after removal. In patients without CSFD placement, if neurologic findings to suspect spinal cord ischemia occur, CSFD should be immediately performed after having confirmed normal coagulation. From experiences of delayed paraparesis over 2 days after TEVAR, it is necessary to give careful hydration and sequential care of blood pressure and hydration after ICU care until discharge for high-risk patients.
Conclusion
Spinal cord injury during TEVAR is not negligible. Perioperative care, from preoperative to postoperative, in TEVAR should be strictly performed according to the protocol proposed by each cardiovascular team.
References
Leurs LJ, Bell R, Degrieck Y, Thomas S, Hobo R, Lundbom J. Endovascular treatment of thoracic aortic diseases: combined experience from the EUROSTAR and United Kingdom Thoracic Endograft registries. J Vasc Surg. 2004;40:670–9.
Chiesa R, Melissano G, Marrocco-Trischitta MM, Civilini E, Setacci F. Spinal cord ischemia after elective stent-graft repair of the thoracic aorta. J Vasc Surg. 2005;42:11–7.
Makaroun MS, Dillavou ED, Kee ST, Sicard G, Chaikof E, Bavaria J, et al. Endovascular treatment of thoracic aortic aneurysms: results of the phase II multicenter trial of the GORE TAG thoracic endoprosthesis. J Vasc Surg. 2005;41:1–9.
Estrera AL, Sheinbaum R, Miller CC, Azizzadeh A, Walkes JC, Lee TY, et al. Cerebrospinal fluid drainage during thoracic aortic repair: safety and current management. Ann Thorac Surg. 2009;88:9–15.
Preventza O, Wheatley GH 3rd, Williams J, Ramaiah V, Rodriguez-Lopez J, Diethrich EB. Identifying paraplegia risk associated with thoracic endografting. Asian Cardiovasc Thorac Ann. 2009;17:568–72.
Khoynezhad A, Donayre CE, Bui H, Kopchok GE, Walot I, White RA. Risk factors of neurologic deficit after thoracic aortic endografting. Ann Thorac Surg. 2007;83:S882–9.
Buth J, Harris PL, Hobo R, van Eps R, Cuypers P, Duijm L, et al. Neurologic complications associated with endovascular repair of thoracic aortic pathology: Incidence and risk factors. A study from the European Collaborators on Stent/Graft Techniques for Aortic Aneurysm Repair (EUROSTAR) registry. J Vasc Surg. 2007;46:1103–10 (discussion 1110–1).
Feezor RJ, Martin TD, Hess PJ Jr, Daniels MJ, Beaver TM, Klodell CT, et al. Extent of aortic coverage and incidence of spinal cord ischemia after thoracic endovascular aneurysm repair. Ann Thorac Surg. 2008;86:1809–14 (discussion 1814).
Amabile P, Grisoli D, Giorgi R, Bartoli JM, Piquet P. Incidence and determinants of spinal cord ischaemia in stent-graft repair of the thoracic aorta. Eur J Vasc Endovasc Surg. 2008;35:455–61.
Cheng D, Martin J, Shennib H, Dunning J, Muneretto C, Schueler S, et al. Endovascular aortic repair versus open surgical repair for descending thoracic aortic disease a systematic review and meta-analysis of comparative studies. J Am Coll Cardiol. 2010;55:986–1001.
Rizvi AZ, Murad MH, Fairman RM, Erwin PJ, Montori VM. The effect of left subclavian artery coverage on morbidity and mortality in patients undergoing endovascular thoracic aortic interventions: a systematic review and meta-analysis. J Vasc Surg. 2009;50:1159–69.
Cheung AT, Pochettino A, McGarvey ML, Appoo JJ, Fairman RM, Carpenter JP, et al. Strategies to manage paraplegia risk after endovascular stent repair of descending thoracic aortic aneurysms. Ann Thorac Surg. 2005;80:1280–8 (discussion 1288–9).
Weigang E, Hartert M, Siegenthaler MP, Beckmann NA, Sircar R, Szabo G, et al. Perioperative management to improve neurologic outcome in thoracic or thoracoabdominal aortic stent-grafting. Ann Thorac Surg. 2006;82:1679–87.
Hnath JC, Mehta M, Taggert JB, Sternbach Y, Roddy SP, Kreienberg PB, et al. Strategies to improve spinal cord ischemia in endovascular thoracic aortic repair: outcomes of a prospective cerebrospinal fluid drainage protocol. J Vasc Surg. 2008;48:836–40.
Rizvi AZ, Sullivan TM. Incidence, prevention, and management in spinal cord protection during TEVAR. J Vasc Surg. 2010;52:86S–90S.
Matsuda H, Fukuda T, Iritani O, Nakazawa T, Tanaka H, Sasaki H, Minatoya K, Ogino H. Spinal cord injury is not negligible after TEVAR for lower descending aorta. Eur J Vasc Endovasc Surg. 2010;39(2):179–86.
Ullery BW, Cheung AT, Fairman RM, Jackson BM, Woo EY, Bavaria J, Pochettino A, Wang GJ. Risk factors, outcomes, and clinical manifestations of spinal cord ischemia following thoracic endovascular aortic repair. J Vasc Surg. 2011;54(3):677–84.
Bicknell CD, Riga CV, Wolfe JHN. Prevention of paraplegia during thoracoabdominal aortic aneurysm repair. Management and prevention of paraplegia during and after Thoracic Aortic stenting and hybrid repair. Eur J Vasc Endovasc Surg. 2009;37:654–60.
DeSart K, Scali ST, Feezor RJ, Hong M, Hess PJ, Beaver TM, et al. Fate of patients with spinal cord ischemia complicating thoracic endovascular aortic repair. J Vasc Surg. 2013;58:635–42.
Wong CS, Healy DH, Canning C, Coffey JC, Boyle JR, Walsh SR. A systemic review of spinal cord injury and cerebrospinal fluid drainage after thoracic endografting. J Vasc Surg. 2012;56:1438–47.
Okita Y. Fighting spinal cord complication during surgery for thoracoabdominal aortic disease. Gen Thorac Cardiovasc Surg. 2011;59(2):79–90.
Martin DJ, Martin TD, Hess PJ, Daniels MJ, Feezor RJ, Lee WA. Spinal cord ischemia after TEVAR in patients with abdominal aortic aneurysms. J Vasc Surg. 2009;49:302–6.
Uchida N. Open stent grafting for complex diseases of the thoracic aorta: clinical utility. Gen Thorac Cardiovasc Surg. 2013;61:118–26.
McNally MM, Aqle SC, Parker FM, Boqey WM, Powell CS, Stoner MC. Preoperative statin therapy is associated with improved outcomes and resource utilization in patients undergoing aortic aneurysm repair. J Vasc Surg. 2010;51:1390–6.
Rizvi AZ, Murad MH, Fairman RM, Erwin PJ, Montori VM. The effect of left subclavian artery coverage on morbidity and mortality in patients undergoing endovascular thoracic aortic interventions: a systematic review and meta-analysis. J Vasc Surg. 2009;50:1159–69.
Schurink GWH, Nijenhuis RJ, Backes WH, Mess W, de Haan MW, Mochtar B, Jacobs MJ. Assessment of spinal cord circulation and function in endovascular treatment of thoracic aortic aneurysms. Ann Thorac Surg. 2007;83:S877–81.
Skuzawa S, Mitsuoka H, Ishigami N, Suzuki K. An experience of distal embolic protection with a filtered temporary AV shunt during TEVAR for shaggy aorta. Jpn J Vasc Surg. 2013;22:1009–12.
Conflict of interest
The author has declared that no conflict of interest exists.
Author information
Authors and Affiliations
Corresponding author
Additional information
This review was submitted at the invitation of the editorial committee.
Rights and permissions
About this article
Cite this article
Uchida, N. How to prevent spinal cord injury during endovascular repair of thoracic aortic disease. Gen Thorac Cardiovasc Surg 62, 391–397 (2014). https://doi.org/10.1007/s11748-014-0395-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-014-0395-9