Abstract
We report a rare case of a pulmonary vein stump thrombus detected by a contrast-enhanced computed tomography for transient syncope 2 days after upper division segmentectomy of the left lung for metastatic pulmonary tumor. The thrombus disappeared without embolic events after anticoagulation with intravenous heparin followed by oral warfarin. Considering this case and previous reports, thoracic surgeons should be aware of pulmonary vein stump thrombus, a latent source of systemic embolization, after pulmonary resection, especially lobectomy or segmentectomy of the left upper lobe. This possible serious complication can occur at any time from the early postoperative period.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thrombus in the pulmonary vein after pulmonary resection is rarely reported. [1–5] This complication has not been adequately described in recent textbooks of thoracic surgery. There are two main thrombus sites: the pulmonary vein of the residual lobe and the pulmonary vein stump. The former represents pulmonary circulation insufficiency, and both sites can cause systemic embolism of any organ. [1–8] We report a case of pulmonary vein stump thrombus detected 2 days after upper division segmentectomy of the left lung for metastatic pulmonary tumor.
Case
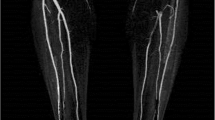
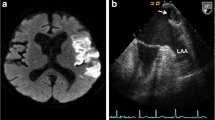
A 76-year-old woman, who had never smoked, was admitted for surgical treatment of a lung nodule (10 mm in diameter) of the left upper division that was suspicious for metastatic lung tumor. She had several previous operations including sigmoidectomy and lymphadenectomy for sigmoid colon cancer (well differentiated adenocarcinoma, pT3N0M0-IIA) 8 years earlier, and then three repeated partial hepatic resections and a partial lung resection of the right lower lobe for liver and lung metastasis followed by chemotherapy. The left lung tumor was detected by routine CT follow-up 8 years after the initial operation (Fig. 1). As the lung nodule was situated deep between S1+2 and S3, a bronchoscopic approach was thought to be difficult. At that time, there was no other suspicious recurrent disease except for the lung nodule. On admission, her physical examination was unremarkable. The concentration of tumor markers such as CEA and CA 19-9 were within the normal range. Coagulation study including prothrombin time, activated partial thromboplastin time, and D-dimer were normal. A thoracoscopic-assisted left upper division segmentectomy was performed for both diagnosis and treatment. The left upper pulmonary vein consisted of V1, V2+3, and V4+5. V1 and V2+3 were ligated and divided separately. As the lobes were completely separated, the lingular division and the lower lobe were fixed by ligation to prevent lung torsion. Intraoperative histopathological examination revealed metastatic adenocarcinoma from colon cancer. Operation time was 139 min and blood loss was 120 g. On the second postoperative day, when walking with assistance in the corridor, she had transient syncope for about 20 s. However, no remarkable change in vital signs or neurological deficit was seen. After the operation, no atrial fibrillation had been observed, and electrocardiography showed sinus rhythm also at this time. A transient cerebral ischemic attack was suspected at first. Although serum D-dimer elevation was slight up to 1.7 μg/dl, emergency chest contrast-enhanced computed tomography (CT) was performed to exclude acute pulmonary thromboembolism. It revealed a thrombus in the stump of the left upper pulmonary vein (Fig. 2), but no apparatus thrombus was seen in the pulmonary artery. Continuous intravenous heparin injection (10,000 units per day) was started. On the 3rd postoperative day, the dose of heparin was increased to 16,000 units per day. On the 8th postoperative day, contrast-enhanced CT of the chest was performed, and there was no change in size of the thrombus in the left upper pulmonary vein. Anticoagulant therapy with oral warfarin was initiated and the intravenous heparin was tapered off. She was discharged on postoperative day 19 receiving warfarin therapy (PT-INR 2.33). Eight months later, contrast-enhanced CT revealed that the thrombus in the left upper pulmonary vein had completely disappeared without any hemorrhagic or embolic events (Fig. 3).
Discussion
Pulmonary vein thrombus after anatomic pulmonary resection is a rare complication and can occur either in the pulmonary vein of a residual lobe, especially in cases associated with lung torsion, [6–8] or in the pulmonary vein stump. [1–5] Both sites of thrombus formation can be potential sources of systemic emboli. The literature on image-proven pulmonary vein stump thrombus has been limited to case reports (Table 1) [1–5]. In these reports, there are three issues that need to be mentioned. First, all the pulmonary vein stump thrombus was derived from the left upper pulmonary vein. Second, arterial embolic events occurred in four of seven cases. Last, the time of onset of the embolic event or the time of thrombus detection ranged from days to months after surgery.
The mechanism of thrombus formation in the stump of a pulmonary vein can be explained by Virchow’s triad, which consists of blood stasis, endothelial injury and hypercoagulability [9]. Blood stasis is thought to be the most specific problem after pulmonary vein closure and the long stump of the pulmonary vein may cause blood stasis. Cronin et al. measured the pulmonary vein distance to first bifurcation in atrial fibrillation patients by multidetector CT [10]. Their study demonstrated that the distance to first bifurcation of the left superior pulmonary vein was statistically larger than that of the other three pulmonary veins. Ohtaka et al. [4] measured the length of the pulmonary vein using CT in patients undergoing lobectomy and reported that the length of the stump of the left superior pulmonary vein was significantly longer than that of the other three pulmonary veins. In order to prevent thrombus formation, it is important that the pulmonary vein stump should be as short as possible, especially in the stump of the left superior pulmonary vein.
Ischemic stroke is a common disease worldwide. Cardioembolic stroke is generally the most severe ischemic stroke subtype. If it occurs in patients undergoing anatomic pulmonary resection late after hospital discharge, it might not be recognized as a complication of pulmonary resection. After an ischemic stroke developed as a result of the thrombus being dislodged from the pulmonary vein stump, the existence of thrombus might not be proved in imaging modalities. Thus, the incidence of ischemic stroke due to pulmonary vein stump thrombus might be much higher than has been reported. Atrial fibrillation is associated with a five-fold increased risk for stroke, mostly due to thromboembolic events [11]. Approximately, 90 % of the thrombi responsible for embolic events originate in the left atrial appendage in patients with nonvalvular atrial fibrillation [12]. Given that long stump of the pulmonary vein behaves similar to the left atrial appendage, thrombus formation in the pulmonary vein stump might be promoted in patients with atrial fibrillation.
In addition to stroke, abdominal organ infarction (two kidneys and a spleen) of unknown cause has been reported after pulmonary resection for lung cancer in three cases [13, 14]. Left upper lobectomy was performed in all three cases. In these cases, pulmonary vein stump thrombus was thought to be responsible for the abdominal embolic events.
In our case, the reason for syncope was unclear, however, a possibility of a transient ischemic attack due to embolism by pulmonary vein stump thrombus could not be excluded. The thrombus was detected in our patient 2 days after surgery, and this is earlier than in other reported cases. Thrombus formation can occur at any time after anatomic pulmonary resection. In asymptomatic patients, the presence of thrombus cannot be excluded without contrast-enhanced CT or transesophageal echocardiography (TEE). [2, 5] Although contrast-enhanced CT is more readily available in routine clinical practice, it seems impossible to set optimal time and the interval of CT examination.
Pulmonary vein stump thrombus is generally treated in the same manner as left atrial appendage thrombus, with anticoagulant therapy using intravenous heparin followed by oral warfarin [3]. Surgical removal of a thrombus has also been reported, in which it extended from the pulmonary vein stump to the left atrium [1]. Because there are so few reported cases, the optimal treatment of this condition remains uncertain. The role of anticoagulant therapy in the prevention of postoperative thrombus formation is not clear either. Certainly, further investigation of the causes, treatment, and prevention of this condition are necessary. However, even more importantly, thoracic surgeons need greater awareness of this potential complication after anatomic lung resection.
Conclusion
We report a case of pulmonary vein stump thrombus detected 2 days after upper division segmentectomy of the left lung for metastatic pulmonary tumor. This potentially lethal complication can occur anytime after anatomic lung resection, especially resection of the left upper lobe of the lung.
References
Seki M, Endo M, Kidani M, Kobayashi H, Sato H, Noto T. A rare case of left atrial thrombus after left upper pulmonary lobectomy. Nihon Kyobu Geka Gakkai Zasshi. 1989;37:1371–5. Japanese.
Schwalm S, Ward RP, Spencer KT. Transient ischemic attack in a patient with pulmonary vein thrombosis after left upper lobectomy for squamous cell lung cancer. J Am Soc Echocardiogr. 2004;17:487–8.
Nagaoka E, Yano M, Sugano T, Miyamoto T. Thrombus in the left superior pulmonary vein after left upper pulmonary lobectomy. J Thorac Cardiovasc Surg. 2008;135:709–10.
Ohtaka K, Hida Y, Kaga K, Iimura Y, Shiina N, Muto J, et al. Pulmonary vein thrombosis after video-assisted thoracoscopic left upper lobectomy. J Thorac Cardiovasc Surg. 2012;143:e3–5.
Gual-Capllonch F, Teis A, Palomeras E. Pulmonary vein spontaneous echocontrast and stroke after pulmonary lobectomy. J Clin Ultrasound. 2012. doi:10.1002/jcu.21913.
Genta PR, Ho N, Beyruti R, Takagaki TY, Terra-Filho M. Pulmonary vein thrombosis after bilobectomy and development of collateral circulation. Thorax. 2003;58:550–1.
Burri E, Duwe J, Kull C, Glaser C, Maurer CA. Pulmonary vein thrombosis after lower lobectomy of the left lung. J Cardiovasc Surg (Torino). 2006;47:609–12.
Apostolakis E, Koletsis EN, Panagopoulos N, Prokakis C, Dougenis D. Fatal stroke after completion pneumonectomy for torsion of left upper lobe following left lower lobectomy. J Cardiothorac Surg. 2006;1:25.
Lowe GD. Virchow’s triad revisited: abnormal flow. Pathophysiol Haemost Thromb. 2003;33:455–7.
Cronin P, Kelly AM, Desjardins B, Patel S, Gross BH, Kazerooni EA, et al. Normative analysis of pulmonary vein drainage patterns on multidetector CT with measurements of pulmonary vein ostial diameter and distance to first bifurcation. Acad Radiol. 2007;14:178–88.
Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22:983–8.
Blackshear JL, Odell JA. Appendage obliteration to reduce stroke in cardiac surgical patients with atrial fibrillation. Ann Thorac Surg. 1996;61:755–9.
Asteriou C, Barbetakis N, Efstathiou A, Kleontas A, Tsilikas C. Renal artery thrombosis following lobectomy for lung cancer. Case Rep Oncol. 2010;3:208–11.
Oura H, Hirose M, Aikawa H, Ishiki M. Abdominal organ infarction encountered immediately after surgery of primary lung cancer. Kyobu Geka. 2005;58:137–42. Japanese.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Asai, K., Mochizuki, T., Iizuka, S. et al. Pulmonary vein stump thrombus: an early complication following upper division segmentectomy of the left lung. Gen Thorac Cardiovasc Surg 62, 244–247 (2014). https://doi.org/10.1007/s11748-013-0229-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-013-0229-1