Abstract
Unknown primary large cell neuroendocrine carcinoma (LCNEC) in the mediastinum is extremely rare. In this report, we present a case of a 53-year-old man with superior vena cava (SVC) syndrome who developed LCNEC in the middle mediastinum. His chief complaint was facial edema. Chest X-ray revealed an abnormal shadow in the right upper mediastinum. Computed tomography (CT) scan of the chest revealed a 67-mm mass in the middle mediastinum. Tumor invasion caused constriction of the SVC. The patient underwent induction chemoradiotherapy with vinorelbin and cisplatin and concurrent radiation therapy. After induction therapy, the tumor size decreased remarkably and was resected completely. The pathological diagnosis was LCNEC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Large cell neuroendocrine carcinoma is a relatively new category of pulmonary neuroendocrine (NE) tumor. Travis et al. proposed a three-grade, four-type scheme for classification of NE tumors of the lung with typical carcinoid (TC) representing a low grade tumor, atypical carcinoid (AC) representing an intermediate grade tumor, and LCNEC and small cell lung carcinoma (SCLC) representing high grade tumors [1, 2]. The prognosis of LCNEC is known to be very poor. Recent clinical studies reported that the 5-year survival rate of patients with LCNEC for all disease stages was 40.3 % [3].
Although LCNEC was first detected in the lung, it appears in various organs. Here we report a very rare case of unknown primary LCNEC in the mediastinum.
Case report
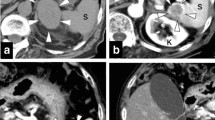
A 53-year-old man was admitted to our hospital for close examination of an abnormal shadow on chest X-ray and computed tomography (CT). His chief complaint was facial edema. He had no other notable examination findings. He had smoked 25 cigarettes per day for 37 years. Chest X-ray revealed a protruding solid mass in the right mediastinum. Enhanced CT revealed a solid mass 67 mm in diameter with severe constriction of SVC and invasion of pulmonary artery in the middle mediastinum (Fig. 1a). PET/CT revealed intense uptake (SUVmax 14.5) of the tumor without any evidence of metastasis (Fig. 1c). Preoperative examination of the brain was not performed. He did not have obvious symptoms of brain metastasis.
a Enhanced CT revealed a solid mass 67 mm in diameter with severe constriction of SVC in the middle mediastinum. b Enhanced CT following induction therapy showed 66 % reduction in tumor size. c FDG-PET revealed intense uptake of the tumor without any evidence of metastasis. d There was no remarkable change in SUVmax after induction therapy. e The resected tumor had infiltrated SVC, but not been exposed to the lumen of the SVC
The levels of tumor markers, such as CEA, CYFRA, Pro-GRP, and IL-2 were normal. The patient subsequently underwent EBUS-TBNA, but there was too little material in the specimen to diagnose. Therefore, we performed thoracoscopic biopsy and interpreted the findings as poorly differentiated squamous cell carcinoma or large cell carcinoma. Thoracoscopic examination revealed that the tumor had not originated in the lung; therefore, we speculated that the tumor had originated in the middle mediastinum. The patient received induction chemoradiotherapy with cisplatin (40 mg/m2) on days 1 and 8, and vinorelbin (25 mg/m2) on days 1 and 8, and concurrent radiotherapy (total dose of 40 Gy). The chemotherapy cycles were repeated every 21 days for two cycles. The venous occlusive symptom disappeared in the early treatment phase. Enhanced CT/FDG-PET following induction therapy showed a partial response (66 % reduction in mass size) (Fig. 1b), but without a remarkable change in FDG activity from maximal standardized-uptake-value of 14.5 pre-therapy to 14.1 post-therapy (Fig. 1d).
After 4 months of initial detection of the tumor, the patient underwent tumorectomy with combined resection of SVC. Vascular reconstruction was performed between the left brachio-cephalic vein and the right auricular appendage, and between the right brachio-cephalic vein and the SVC with ringed polytetrafluoroethylene (PTFE) grafts. The resected tumor was 18 mm in diameter, had infiltrated SVC, but not been exposed to the lumen of the SVC (Fig. 1e). Microscopically, tumor cells were large and polygonally shaped, and had low nuclear to cytoplasmic ratio, coarse nuclear chromatin, and frequent necrosis. The tumor cells were scattered, forming abortive rosette-like structures. Immunohistochemically, the tumor cells were positive for synaptophysin, epithelial membrane antigen (EMA) and cytokeratin, but negative for thyroid transcription factor-1 (TTF-1) and choromogramin A.
Although CT scan revealed more than 66 % reduction in tumor size, most of the residual tumor cells were viable pathologically. Since there was no histological basis to suggest any primary organ of origin in the mediastinum, such as thymic tissue, or any evidence consistent with a lymph node metastasis, we labeled the tumor as an unknown primary LCNEC in the mediastinum.
The patient had an uneventful recovery and was discharged from the hospital on the 14th postoperative day. However, he developed multiple brain metastases with nausea and headache approximately 2.5 months postoperatively and he was treated with whole-brain irradiation. Unfortunately, he died of extensive brain metastasis 5 months after surgery. At least, there were no other significant recurrences, including in the lung or local recurrence, in the examination conducted 1 month before the patient’s death.
Discussion
Large cell neuroendocrine carcinoma is a new category of pulmonary neuroendocrine tumor, whereas LCNEC in the mediastinum is extremely rare. The majority of the reported causes of mediastinal LCNEC originated from thymus. To the best of our knowledge, unknown primary LCNEC in the mediastinum have been reported only 5 cases in the literature including our cases to date [4–7] (Table 1). Patient characteristics, treatments and prognoses are summarized in Table 1. All patients were males. The mean age of the 5 patients was 51.2 years (range 35–65). Three patients were asymptomatic. Induction CDDP-based chemotherapy was performed in 2 cases (nos. 2, 5), showing partial response (PR). Although complete resection was performed after induction chemotherapy, LCNEC recurred shortly postoperatively in both cases. The median overall survival was 11 months (range 2–13 months).
LCNEC is associated with poor prognosis due to high propensity for early distant hematogenous metastases. LCNEC and SCLC are categorized as high grade NE tumours because of their poor prognosis compared with those of other NE tumours of the lung.
Iyoda et al. reported 50 % postoperative recurrence rate of LCNEC in the lung [8]. Since the biological characteristics of LCNEC are similar to those of small cell lung cancer [3], these cases are trend to treat with chemotherapy regimens used for small cell lung cancer.
Previous reports suggest that perioperative chemotherapy is necessary to improve survival in patients with LCNEC of the lung. The 5-year survival rate of patients who underwent perioperative adjuvant chemotherapy was 87.5 %, whereas that of patients who underwent surgery alone was 58.5 % [9].
Some studies suggest that complete resection of pulmonary LCNEC followed by adjuvant chemotherapy using a regimen used to treat small cell lung cancer (platinum plus etoposide) could yield good outcomes [10, 11]. Rossi et al. reported a better survival for the 38 patients who received adjuvant chemotherapy. The multivariate analyses showed a better outcome for patients receiving a regimen of SCLC (platinum-etoposide) than a regimen of NSCLC (p = 0.0001) [10].
The role of neoadjuvant/adjuvant therapy for mediastinal LCNEC has not been adequately assessed given the limited number of reported cases. In the present case, induction therapy followed by surgery led to a complete resection of the tumor. However, the patient developed multiple brain metastases soon after surgery. The high biological malignancy grade of mediastinal LCNEC is clear from previously reported cases. We think that adjuvant chemotherapy should be administered to prevent distant metastasis. However, in our case, the patient could not be administered adjuvant chemotherapy because of his emaciation. When considering the severe biological malignancy grade and the frequency of brain metastases, prophylactic whole-brain irradiation may be beneficial. However, there is no evidence of the benefits of postoperative prophylactic irradiation in cases of LCNEC. We should consider postoperative whole-brain irradiation to prevent brain metastasis in the future.
Further study is warranted to determine the efficacy of adjuvant therapy for mediastinal LCNEC.
Conclusions
We encountered a rare case of unknown primary LCNEC in the mediastinal. It was radically resected following induction therapy. The effect of induction therapy on mediastinal LCNEC has not been adequately assessed. In the present case, concurrent induction chemoradiotherapy with cisplatin and vinorelbin plus radiotherapy was shown to be effective. Induction therapy should be considered as one of the treatment options for radical resection.
References
Travis WD, Linnoila RI, Tsokos MG, Hitchcock CL, Cutler GB Jr, Nieman L, et al. Neuroendocrine tumors of the lung with proposed criteria for large-cell neuroendocrine carcinoma. An ultrastructural, immunohistochemical, and flow cytometric study of 35 cases. Am J Surg Pathol. 1991;15:529–53.
Travis WD, Rush W, Flieder DB, Falk R, Fleming MV, Gal AA, et al. Survival analysis of 200 pulmonary neuroendocrine tumours with clarification of criteria for atypical carcinoid and its separation from typical carcinoid. Am J Surg Pathol. 1998;22:934–44.
Asamura H, Kameya T, Matsuno Y, Noguchi M, Tada H, Ishikawa Y, et al. Neuroendocrine neoplasms of the lung: a prognostic spectrum. J Clin Oncol. 2006;24:70–6.
Natsuhara A, Iwasaki Y, Minagawa T, Takemura Y, Nakanishi M, Nagata K, et al. Aggressively metastatic neuroendocrine carcinoma in the middle mediastinum. Jpn J Respir. 2001;39:705–9.
Takezawa K, Okamoto I, Fukuoka J, Tanaka K, Kaneda H, Uejima H, et al. Large cell neuroendocrine carcinoma of the mediastinum with alpha-fetoprotein production. J Thorac Oncol. 2008;3:187–9.
Nojima D, Kiura K, Hotta K, Takigawa N, Tabata M, Tanimoto M. Large cell neuroendocrine carcinoma of the mediastinum. Nihon Kokyuki Gakkai Zasshi. 2010;48:506–10.
Lukina O, Gorbunkov S, Dvorakovskaja I, Varlamov V, Akopov A. Fast-growing large cell neuroendocrine carcinoma of mediastinum. Ann Thorac Surg. 2011;91:1618–20.
Iyoda A, Hiroshima K, Moriya Y, Iwadate Y, Takiguchi Y, Uno T, et al. Postoperative recurrence and the role of adjuvant chemotherapy in patients with pulmonary large-cell neuroendocrine carcinoma. J Thorac Cardiovasc Surg. 2009;138:446–53.
Saji H, Tsuboi M, Matsubayashi J, Miyajima K, Shimada Y, Imai K, et al. Clinical response of large cell neuroendocrine carcinoma of the lung to perioperative adjuvant chemotherapy. Anticancer Drugs. 2010;21:89–93.
Rossi G, Cavazza A, Marchioni A, Longo L, Migaldi M, Sartori G, et al. Role of chemotherapy and the receptor tyrosine kinases KIT, PDGFRalpha, PDGFRbeta, and Met in large-cell neuroendocrine carcinoma of the lung. J Clin Oncol. 2005;23:8774–85.
Iyoda A, Hiroshima K, Moriya Y, Takiguchi Y, Sekine Y, Shibuya K, et al. Prospective study of adjuvant chemotherapy for pulmonary large cell neuroendocrine carcinoma. Ann Thorac Surg. 2006;82:1802–7.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maeda, A., Nakata, M., Yasuda, K. et al. Unknown primary large cell neuroendocrine carcinoma (LCNEC) in the mediastinum. Gen Thorac Cardiovasc Surg 61, 542–545 (2013). https://doi.org/10.1007/s11748-012-0157-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-012-0157-5