Abstract
Lipid emulsions are made by mixing vegetable and/or fish oils with egg yolk and contain different types and amounts of fatty acids and sterols. This study assessed the effects of oral diet, soybean oil (SO)-, fish oil (FO)-, a mixture of olive and soybean oil (OOSO)-, and a mixture of fish, olive, coconut, and soybean oil (FOCS)-based emulsions on plasma triacylglycerols and plasma and tissue fatty acid and sterol content following acute and chronic intravenous administration in the guinea pig. Upon acute administration, peak triacylglycerols were highest with SO and lowest with OOSO. Upon chronic administration, the plasma triglyceride levels did not increase in any group over that of the controls. Fatty acid levels varied greatly between organs of animals on the control diets and organs of animals following acute or chronic lipid administration. Squalene levels increased in plasma following acute administration of OOSO, but plasma squalene levels were similar to control in all emulsion groups following chronic administration. Total plasma phytosterol levels were increased in the SO, OOSO, and FOCS groups following both acute and chronic infusions, whereas phytosterols were not increased following FO infusion. Total phytosterol levels were higher in liver, lung, kidney and adipose tissue following SO and OOSO. Levels were not increased in tissues after FO and FOCS infusion. These results indicate that fatty acid and sterol contents vary greatly among organs and that no one tissue reflects the fatty acid or sterol composition of other tissues, suggesting that different organs regulate these compounds differently.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fatty acids and sterols are important cellular substrates and structural components. They form the major content of cellular membranes. The structure of cell membranes modulates cellular functions through effects upon receptor action, ion channel function, and cell signaling [1]. In addition to membrane effects, sterols are the precursors to bile acids and modulate biliary flow which is important in the elimination of cholesterol, phytosterols, and many drugs from the body. Lipid emulsions (LE) are the source of fatty acids and sterol intake for patients receiving total parenteral nutrition and provide substrates for energy, cholesterol, and essential fatty acids [2]. However, the effects of different lipid emulsions upon fatty acid and sterol contents of the major organs remain unclear.
The LE used in this study are based upon different oils (i.e., soybean oil, olive oil, coconut oil, fish oil) and represent the most common LE used worldwide. The different oils contain different quantities of fatty acids in the form of triacylglycerols [3]. However, the LE also contains steroidal compounds and their precursors [4]. These compounds include cholesterol, phytosterols and squalene. Although all plant oils contain phytosterols, the levels differ among plants. For example, olive oil contains lower phytosterols than soybean oils. The most common phytosterols in vegetable oils are sitosterol, campesterol, and stigmasterol [5]. Phytosterols are minor components of parenteral LE. In the past they were often ignored and considered harmless during parenteral infusion.
Cholesterol is metabolized in the body to bile acids and eliminated through biliary or intestinal secretion. In contrast, phytosterols are not metabolized but are eliminated through biliary excretion. There is limited absorption (i.e., 1–5 %) of phytosterols from the gastrointestinal tract [6, 7]. However, parenteral administration of phytosterols in LE may deliver more than 40 fold greater amounts into the circulation. Phytosterols compete with cholesterol and bile acids in the body and associate with the development of cholestasis and liver failure (i.e., parenteral nutrition associated liver disease or PNALD) [8–17]. Due to the risk of development of hepatobiliary disease, the FDA recently requested Baxter Healthcare (Deerfield, IL) to perform post marketing studies comparing a phytosterol reduced lipid emulsion to their approved lipid emulsion that contains phytosterols [18]. Thus, a better understanding of phytosterol intake and metabolism (i.e., distribution, excretion, and cellular effects) may help limit the development of PNALD and other cellular toxicities.
The primary objective of this study was to assess fatty acid, squalene, and sterol contents of different tissues and to describe differences in tissue content of these lipids. We also sought to evaluate the effects of four different LE upon circulating and tissue levels of fatty acids, squalene, and sterols. We determined the degree to which LE could alter tissue fatty acid and phytosterol contents compared to oral diets. We were particularly interested in the effect of a fish oil emulsion upon tissue n-3 fatty acid levels in various organs and whether the liver was the primary organ for deposition of phytosterols (since these compounds are linked to liver dysfunction). This is the first study to measure tissue distribution of these compounds in animals following oral diets and intravenous LE. This information is important for understanding the potential consequences of LE infusion upon tissue structure and function and to help direct future studies related to LE infusions. The study also addresses the potential for using one tissue as a proxy for lipid contents of other tissues.
Materials and Methods
Animals
Hartley Guinea pigs, with their jugular vein catheterized, were purchased from Charles River Laboratories International, Inc. (Wilmington, MA 01887). All guinea pigs were housed under controlled temperature and humidity in the Methodist Research Institute Animal Care Facility, with a 12 hour light-dark cycle. Animals were provided with food and water ad libitum. The dietary composition of the oral diets are described in the supplemental data (Table 1). The fatty acid and phytosterol composition of the different diets used in this study are reported in the supplemental data (Tables 2 and 3, respectively). The protocol for these studies was approved (protocol # 2010-17) by the Methodist Research Institute’s Animal Research Committee (Animal Welfare Assurance Number-A3772-010) and strictly followed the Guide for the care and use of laboratory animals (NIH publication No. 85-23, revised 1996).
In Vivo Lipid Emulsion Infusions
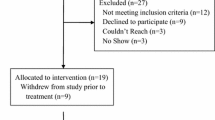
Two separate studies were performed. The acute study evaluated the effects of a single one-hour lipid infusion upon plasma and tissue fatty acid/squalene/sterol levels over a 6-hour period. The chronic study evaluated the effects of the study LE administered daily for 10 days upon the same parameters.
For acute infusion studies, guinea pigs were fed regular guinea pig chow (Diet # 2040; Harlan Laboratories, Indianapolis, IN) during acclimation for 3–4 days prior to treatment with LE. The guinea pigs (5/group) were subjected to an overnight fast with ad libitum access to water. Early the following morning, the control group of animals was used to collect blood and tissues to establish baseline levels of the study biomarkers. The animals in other groups were then administered, via the jugular vein, 5 mL of one of the study lipid emulsions over a 1-hour period using a Harvard syringe pump (Instech Laboratories, Plymouth Meeting, PA). Thus, animals were infused with 1 gram of lipid (20 % emulsions; approximately 2.6 g/kg/day) or 0.5 g of lipid (10 % emulsions; approximately 1.3 g/kg/day) (see lipid emulsions below). The animals were maintained under fasting conditions throughout the acute study. Blood (1 mL) was collected at 2, 3, 4, 5, and 6 hours after initiation of the lipid infusion. Blood volume was replaced with an equal volume of 5 % albumin in Phosphate Buffered Saline (PBS; 0.01 M phosphate buffer, 0.145 M NaCl, pH 7.4). Heparinized blood samples were placed on ice. Plasma was obtained following centrifugation (800×g). The white blood cell buffy coat was discarded, and the red blood cells (RBC) were washed three times in PBS and stored at −20 °C. At the 6-hour time period, the animals were euthanized and liver tissue was isolated, weighed and snap-frozen in liquid nitrogen for biochemical analysis. Triacylglycerols (TG) at 0–6 h, and hepatic enzymes/bilirubin at 6 hours (described below) were analyzed in plasma only; furthermore, plasma, RBC and liver tissues were used to measure fatty acid and sterol levels at 6 hours. A portion of the liver was also embedded in optimal cutting temperature (OCT) compound for histological examination.
For chronic lipid infusion studies, animals were acclimated for 3–4 days on the chow diet, and then placed on a transition guinea pig diet (D10091201 containing 30 % proteins, 55 % carbohydrates and 15 % fat; Research Diets, New Brunswick, NJ) for one week prior to treatment with the study lipid emulsions. The transition diet was used to help switch guinea pigs from a regular chow diet to an experimental fat free diet (used during intravenous lipid administration) as guinea pigs take time to adapt (i.e., establish a new steady-state intake of food) when their diets are changed. After a week of the transition diet, the guinea pigs for LE treatment were switched to a fat-free diet (D10091202 containing 36 % protein, 64 % carbohydrate and 0 % fat; Research Diets, New Brunswick, NJ) and treated with LE infusions (5/group) for 10 days. The fat free diet was the same as the transition diet except that it lacked fat. These animals were administered, via the jugular vein, 5 mL of LE over a 1-hour period using syringe pumps, daily, for 10 consecutive days (i.e., 1 g/day or 2.6 g/kg/day for 20 % LE; 0.5 g/day or 1.3 g/kg/day for 10 % LE). The control group guinea pigs (n = 5) were continued on the transition diet for the 10-day study period. At the end of the 10-day period, all animals were fasted overnight, blood was then collected (5 mL), and the animals were euthanized. Organs (liver, lungs, kidneys, heart, and epididymal adipose tissues) were harvested. A portion of the liver was embedded in OCT compound for histological examination, and the remaining portions were snap-frozen in liquid nitrogen for biochemical analyses. Plasma and RBC were obtained from blood as described above. TG and hepatic enzymes/bilirubin were analyzed in the plasma. Fatty acid and sterol levels were ascertained in plasma, RBC, and tissues. All these assays were performed in the overnight fasted animals.
Study Lipid Emulsions
Four different commercially available LE were evaluated. The LE were a 100 % soybean oil (SO) emulsion (Intralipid®, Fresenius-Kabi, Bad Homburg, Germany), an 80 % olive oil and 20 % soybean oil emulsion (OOSO) (ClinOleic®, Baxter Healthcare, Deerfield, IL), a 100 % fish oil emulsion (FO) (Omegaven®, Fresenius-Kabi, Bad Homburg, Germany), and a mixture of fish oil (15 %), olive oil (25 %), coconut oil (30 %), and soybean oil (30 %) emulsion (FOCS) (SMOFlipid®, Fresenius-Kabi, Bad Homburg, Germany). The FO emulsion is only available as a 10 % (10 g/100 mL) lipid emulsion while the other three emulsions are available as 20 % (20 g/100 mL) emulsions. All LE contained 1.2 g/100 mL of egg yolk phospholipids.
Analysis of Plasma Triacylglycerols
Analysis of TG in plasma was performed by Baxter Healthcare Corporation’s Clinical Chemistry Lab (Round Lake, IL), using validated methodology in accounting for the background glycerol correction.
Analysis of Hepatic Toxicity
Hepatic integrity was evaluated using levels of plasma alkaline phosphatase (ALP), alanine aminotransferase (ALT), aspartate aminotransferase (AST) and total bilirubin. These assays were performed by Baxter Healthcare Corporation’s Clinical Chemistry Lab (Round Lake, IL), using validated methodology (ALP-document # AOSR6x04.01, ALT document # AOSR6x07.0, AST document # AOSR6x09.01, total bilirubin document # AOSR6x118.01, Olympus America Inc, Irving TX).
Fatty Acid Analysis
Diets were pulverized and samples (200 mg) were extracted using chloroform. An internal tricosanoic acid standard (C23:0 in hexane) was added prior to extraction. Samples were centrifuged at 900×g to separate phases and the clear bottom chloroform layer was removed and dried under nitrogen flow at 37–40 °C. To the residues, methanol-benzene 4:1 and acetyl chloride was added while on dry ice. The samples were placed in tubes, purged with nitrogen gas, and subjected to methanolysis at room temperature for 24 hours. The reaction was stopped and neutralized with K2CO3. Layers were separated by centrifugation and an aliquot of the benzene layer was removed for gas chromatography analysis [3]. Lipid emulsions (20 µL each) did not require fatty acid extraction prior to analysis; therefore, these samples were directly transmethylated as described above in conjunction with an internal standard.
For tissue analysis of fatty acids, a small sample (approximately 200 mg) was removed from −80 °C, thawed on ice, and homogenized in cold PBS. An internal standard of tricosanoic acid was added to the homogenates (also used for plasma and RBC analyses) and methanol:benzene 4:1 added. Acetyl chloride was added while on dry ice, the samples sealed, transferred to room temperature, and maintained until the reaction mixture was melted. Transmethylation was performed as described above. Fatty acid extraction of the guinea pig plasma (100 µL) prior to analysis was not required; therefore, transmethylation of these samples were performed as described above. Guinea pig RBC were removed from −80 °C, slowly thawed on ice, vortexed, and then cold PBS was added to 400 µL of packed RBC. Samples were homogenized and homogenates (100 µL) were transmethylated as described above using an internal standard. Because of the high fat content of adipose tissue, direct transmethylation was administered to analyze the fatty acid content (approximately10 mg of tissue). Methanol-benzene 4:l (v/v) was added, and the tubes were gently vortexed. Samples were placed on a dry ice bath prior to the addition of acetyl chloride. The samples were purged with nitrogen gas, tightly sealed, and subjected to heating (70 °C for 10 min). The samples were maintained at room temperature for 24 hours prior to gas chromatography analysis.
For gas chromatography analysis of fatty acids, the benzene layer was recovered following centrifugation and fatty acids were separated on a gas chromatography system (Shimadzu GC2010) equipped with a Zebron ZB-WAX plus column (100 m, 0.25 mm ID, 0.25 μm film thickness) as described previously [3]. The oven temperature was programmed from 30 °C (2 min. hold) to 180 °C at 20 °C/min (2 min. hold), then to 207 °C at 4 °C/min (3 min. hold), then to 220 °C at 2 °C/min (2 min. hold), and finally to 240 °C at 2 °C/min (2 min. hold). Detection was performed with a FID at 250 °C to resolve fatty acids peaks, which were identified using authentic standards (Restek Corp., Bellefonte, PA). Data were analyzed with Shimadzu’s GC solutions software. Data are presented either as % of total fatty acids reported in Table 1 or mg or μg/volume or weight of tissues. Fatty acids that were below the limit of detection (i.e., 20 μg/mL in plasma, 30 μg/g tissues, and 0.05 μg/mg protein in RBC) are reported as not detected (ND).
Analysis of Sterols
Pulverized diets were accurately weighed and placed in Pyrex tubes with an internal standard, 5α-cholestane (2.6 µM), and 2 M KOH in ethanol with 20 % water and 3 % pyrogallol. These samples were saponified for 1 hour at 100 °C. After cooling, water and hexane were added to the mixture. Samples were vortexed, centrifuged at 1,500×g for 10 minutes, and the upper hexane layer was collected. The hexane extraction step was repeated. These extracts were combined, dried under nitrogen gas, and the residues were dissolved in 200 μL of hexane for GC analysis. Tissue homogenates, plasma, or lipid emulsions (200 μL), along with the addition of the internal standard, were extracted and processed as described above [4]. An internal standard, 5α-cholestane, was added to adipose tissue (50 mg) in conjunction with 2 M KOH as described above. These samples were saponified for 10 minutes at 100 °C, sonicated for 30 minutes, followed by an additional 50 minutes at 100 °C. The sterol extractions were executed as described above.
For gas chromatography analysis of sterols, the hexane layer was recovered following centrifugation, and separated on a gas chromatography system (Shimadzu GC2010) equipped with a SAC-5 capillary column (30 m, 0.25 mm ID, 0.25 μm film thickness) as described previously [4]. The oven temperature was programmed to 270 °C (1 min. hold), then to 280 °C at 2 °C/min (5 min. hold), then finally to 285 °C at 1 °C/min (20 min. hold). Peaks were identified using authentic standards. Sterol concentrations were normalized to the internal standard and calculated based on an external standard curve. Data were analyzed with Shimadzu’s GC solutions software.
Statistical Analysis of Data
The data are reported as means ± SD unless stated otherwise. All comparisons are made by one-way ANOVA with Tukey’s post hoc test using SPSS Statistics 20 software except for fatty acid analyses. Fatty acids analyses were done on the normalized data (not adjusted for interdependence) using “R (version 1.15.1)” software [19] from means and standard deviations. Means differences were compared using studentized range with Tukey’s hsd (honestly significant difference). All significant values are reported at P < 0.05.
Results
Fatty Acid Composition of Lipid Emulsions
The fatty acid composition of the four study emulsions is in line with the known fatty acid composition of the various oils used to manufacture the emulsions. As presented in Table 1, the SO emulsion contained linoleic acid as the major fatty acid in the emulsion, accounting for nearly 55 % of total fatty acid content. The OOSO lipid emulsion contained oleic acid as the major fatty acid (approximately 60 % of the total fatty acid content), whereas linoleic acid was the second most abundant fatty acid (approximately 19 %). The FO lipid emulsion contained approximately 54 % of fatty acids as long-chain n-3 polyunsaturated fatty acids (n-3 PUFA) with approximately a 1:1 eicosapentaenoic acid (EPA) to docosahexaenoic acid (DHA) ratio. The FOCS emulsion contained substantial quantities of medium-chain fatty acids (C6-10; approximately 30 %). Oleic acid and linoleic acid were present at approximately 25 and 20 % levels, whereas n-3 PUFA accounted for nearly 8 % of total fatty acids with a 1.5:1 EPA to DHA ratio.
Plasma Triacylglycerols After Acute and Chronic Infusion of Lipid Emulsions
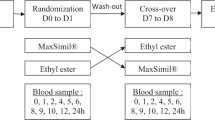
Acute administration of the LE showed different pharmacokinetic behavior for the various emulsions (as presented in Fig. 1a). Triacylglycerols from SO rose to a significantly higher level (P < 0.05) than the other emulsions. In addition, the peak FOCS lipid triacylglycerol levels were higher than the OOSO and FO lipid groups. The clearance of the LE also varied. The time to reduce triacylglycerols by 50 % from the peak level (2-hour level) was approximately 0.55 ± 0.17 hour for FOCS, 1.15 ± 0.56 hour for SO, 1.38 ± 0.27 hour for OOSO, and 1.40 ± 0.10 hour for FO. Upon chronic administration of the LE over 10 days, the plasma triacylglycerol levels were significantly (P < 0.05) lower following infusion of the SO, OOSO, and FO lipids compared to the FOCS emulsion and control diet group (Fig. 1b).
Pharmacokinetics of plasma triacylglycerols (TG) during acute administration of lipid emulsion (a) and after chronic lipid emulsion infusion (b). Triacylglycerols were assayed using a validated enzymatic method that corrected for background glycerol content. Values are means ± SD of five guinea pigs in each group. Data are analyzed by one-way ANOVA with Tukey’s post hoc test. Values labeled with dissimilar symbols exhibit significant differences at P < 0.05. Note normal plasma triacylglycerol concentration in guinea pig plasma ranges from 28–76 mg/dL [36]. To convert mg/dL to mmol/L (mM), multiply mg/dL by 0.0113
Effect of Lipid Emulsions on Liver Integrity and Body Weights
Plasma levels of alkaline phosphatase (ALP), alanine aminotransferase (ALT), aspartate aminotransferase (AST), and bilirubin were not significantly changed during acute (6-h) LE infusion (data not shown). Similarly, chronic infusion of LE for 10 days also did not increase plasma ALP, ALT, AST, or total bilirubin levels over levels in the control animals (supplementary data Table 4). Interestingly, infusion of SO, OOSO, and FO produced approximately a 40–50 % reduction in ALP activities (supplementary Table 4). Histology of liver samples showed no sign of Oil red O’ staining after chronic infusion of any of these LE (data not shown) indicating no accumulation of TG in liver. Furthermore, chronic infusion of LE (i.e., 10 days) resulted in similar gain in body and organ weights (supplementary data Table 5).
Tissue Distribution of Fatty Acids
The distribution of fatty acids in total lipids of different tissues after acute (plasma, RBC and liver) or chronic (plasma, RBC, heart, liver, lungs, kidney and adipose tissue) administration of the study LE was determined. We analyzed all 39 fatty acids as listed in Table 1, but only report data for the most metabolically relevant fatty acids (16:0,18:0, 18:1n-9, 18:2n-6, 18:3n-3, 20:4n-6, 20:5n-3, 22:5n-3, 22:6n-3) as percent of total fatty acids for simplicity in Table 2. These fatty acids account for 85–95 % of total fatty acids in plasma, RBC, and liver.
Fatty acid content of plasma, liver, and RBC for the acute study are reported in Tables 2 and 3. Levels of many of the fatty acids differed significantly between tissue specimens. In general, fatty acid changes in plasma and liver reflecting the composition of the LE as early as 6 hours post-infusion. Linoleic acid increased in the SO group and decreased in the OOSO and FO groups. Oleic acid increased in the OOSO group while EPA + DPA + DHA increased in the FO and FOCS groups. In contrast, RBC maintained fatty acid levels similar to the control group.
Total fatty acid concentrations (by weight) in plasma and RBC were not significantly different in any lipid infusion group compared to that of control (Table 3); however, fatty acid concentrations in the LE groups were increased significantly in liver compared to the control group. There were no significant differences between emulsion groups. The changes in fatty acid levels in the liver reflected the composition of the individual lipid emulsions and indicate that hepatic fatty acid levels can change within 6 hours of intravenous lipid administration. Although FOCS contained significant amounts of MCT, no detectable levels of medium chain fatty acids were found in any of the tissues.
In the chronic study, levels of the major metabolically relevant fatty acids (16:0,18:0, 18:1n-9, 18:2n-6, 18:3n-3, 20:4n-6, 20:5n-3, 22:5n-3, 22:6n-3) were compared across the various organs in animals on the control diets and following LE infusion (Tables 4 and 5). The results demonstrated highly variable quantities of the various fatty acids in different tissues and no one tissue was reflective of the others. For example, linoleic acid predominated over arachidonic acid in all tissues in animals on the control diet. However, levels were close to 1:1 in RBC, kidneys, lungs, and heart, while linoleic acid greatly exceeded arachidonic acid in plasma, liver, and adipose tissues. The linoleic:arachidonic acid ratio (%) was 24:21 in heart and 28:0.17 in adipose tissue. In control animals, the ratio of DHA/EPA was greater than one in heart (3.07), RBC (2.29), liver (2.11) and adipose tissue (2.5). The ratio of DHA/EPA was less than one in plasma (0.73), lungs (0.43), and kidneys (0.53). Fatty acid changes in the tissues following infusion of the LE were reflective of the composition of the oils used in the LE. Oleic acid levels decreased in the SO, FO and FOCS groups but remained at baseline in the OOSO group. Linoleic acid levels significantly decreased in the OOSO, FOCS, and FO groups while it remained at baseline levels in the SO group. Despite changes in linoleic acid, arachidonic acid was maintained at control levels or increased in all organs except for the heart. Levels of EPA and DHA remained at baseline in the SO and OOSO groups while they significantly increased in the FO and FOCS groups. However, the increase in n-3 fatty acids varied greatly between tissues. Levels of EPA + DPA + DHA reached 2.63 % in adipose tissue, 6.46 % in RBC, 8.53 % in lungs, 11.39 % in kidneys, 13.4 % in plasma, 14.46 % in heart, and 26.09 % in liver.
Although infusion of different lipid emulsions caused changes in relative distribution of fatty acids in different tissues, the total fatty acid concentrations (by weight) were not significantly different in any tissue after chronic infusion of LE (Table 5). Interestingly, most organs maintained their total saturated, monounsaturated and polyunsaturated fatty acid contents similar to that of the control levels; however, tissues exhibited changes in the relative concentration of n-3 and n-6 PUFA contents (Table 5). Furthermore, similar to acute studies, none of the tissues accumulated detectable levels of medium chain fatty acids during chronic treatment.
Sterol and Squalene Contents of Diets and Lipid Emulsions
The diets contained variable amounts of squalene, cholesterol, and phytosterols (supplementary data Table 3). The primary phytosterols in the diet were β-sitosterol, campesterol, and stigmasterol. The normal chow diet also contained significant amounts of β-sitostanol. All diets contained reasonable amounts of cholesterol. Squalene was found in the 15 % fat diet, which contained olive oil as a source of lipid. The LE were also found to contain variable amounts of sterols (both cholesterol and phytosterols), and the cholesterol precursor squalene, depending on the oil source (Table 6).
Plasma Levels of Sterols and Squalene
Plasma levels of sterols and squalene differed between LE groups, and between acute and chronic lipid administration (Table 7). Following chronic LE infusion, plasma cholesterol levels were decreased in the FO group but maintained at control levels in the other lipid groups. Total plasma phytosterol levels were higher in the acute study control animals compared to the chronic study control animals (10.33 vs 3.83 µg/mL) (Table 7). This difference reflects the different oils used and the lower fat content of the diet used in the chronic study. Following chronic infusion of the study lipids, total plasma phytosterol levels and β-sitosterol were increased in the SO, OOSO, and FOCS groups; however, levels were decreased in the FO group. Although the concentration of stigmasterol was similar to campesterol in the different lipid emulsions (Table 6), the plasma did not show detectable levels of stigmasterol. Phytosterol levels were higher in animals after the acute infusion compared to the chronic infusion. The difference probably reflects clearance of the phytosterols since levels were measured 6 hours after infusion in the acute study and after an overnight fast in the chronic study.
Tissue Levels of Sterols and Squalene
Tissue sterol and squalene content after acute (Table 8) and chronic (Figs. 2, 3) LE administration were measured to determine the distribution of different phytosterols. Despite the presence of stigmasterol in the diets and LE, we did not detect stigmasterol in the tissues. Similar to acute lipid infusion, none of the LE produced significant changes in sterol or squalene levels in RBC following chronic infusion (Fig. 2). Following chronic LE infusion, squalene was highest in adipose tissue and levels were significantly increased in the liver following OOSO (Fig. 3a). Phytosterol content was highest in the lung and adipose tissue (Fig. 3b, c). β-Sitosterol levels were increased in liver, lung, kidney, and adipose tissue with SO and OOSO compared to FO and FOCS. Campesterol levels were increased with SO in liver, heart, lung, and adipose tissue (Fig. 3c).
Distribution of squalene, β-sitosterol, campesterol and cholesterol in RBC after chronic lipid emulsion infusion. Stigmasterol was not detected. Sterols were analyzed using a GC system. Values are means ± SD of five guinea pigs in each group. Data are analyzed by one-way ANOVA with Tukey’s post hoc test. No significant differences in squalene, phytosterol, and cholesterol contents were observed between lipid emulsion groups
Tissue distribution of squalene (a), β-sitosterol, (b) campesterol (c), and cholesterol (d) after chronic lipid emulsion infusion. Stigmasterol was not detected. Sterols were analyzed using a GC system. Values are means ± SD of five guinea pigs in each group. Data are analyzed by one-way ANOVA with Tukey’s post hoc test. Values labeled with dissimilar symbols exhibit significant differences at P < 0.05
Discussion
This is the first study to compare fatty acid and sterol contents across multiple tissues in animals on oral diets and following administration of different LE. We were particularly interested in determining whether one tissue specimen could be used as a proxy for other tissue specimens and the distribution of phytosterols across different organs. Our results indicate that fatty acids and sterol levels vary greatly between tissues and that no one tissue was a good proxy for the others. We also report that sterol levels (cholesterol and phytosterols) vary greatly between tissues with the highest contents in lung and adipose tissue.
The study demonstrates widely varying fatty acid content of plasma and other tissues (i.e., RBC, heart, liver, lungs, kidney, and adipose tissue) in control and lipid-infused animals. For example, in control (oral diet) animals, oleic acid varied from 7.8 % in heart to 38.5 % in adipose tissue; linoleic acid varied from 11.7 % in RBC to 34.4 % in liver; arachidonic acid levels varied from 0.17 % in adipose tissue to 13.9 % in kidney; total n-3 PUFA varied from 0.82 % in liver to 3.37 % in adipose tissue. Total fatty acid content of the tissues was similar. Thus, the changes in relative composition of the fatty acids also reflect absolute concentrations.
The accumulation of long-chain n-3 PUFA (i.e., ALA, EPA, DPA, DHA) varied greatly in tissues following FO administration. Plasma, heart, and liver achieved the highest relative concentrations (14–15 % for heart and plasma; 26 % for liver). Adipose tissue and RBC achieved the lowest relative levels (5.7–6.7 %). It was also interesting that DHA exceeded EPA accumulation in liver (DHA/EPA ratio = 3.29), heart (DHA/EPA ratio = 2.62), plasma (DHA/EPA ratio = 1.37), RBC (DHA/EPA ratio = 1.34), and adipose tissue (DHA/EPA ratio = 1.2). In contrast, EPA exceeded DHA accumulation in lungs (DHA/EPA ratio = 0.78) and kidney (DHA/EPA ratio = 0.32). These differences in ratios of DHA to EPA are very interesting in view of the DHA/EPA ratio of the FO emulsion of 0.91. The results indicate that tissues regulate the levels of DHA and EPA differently and independent of the relative supply. The large variations between tissue levels of n-3 PUFA and other fatty acids is interesting since these fatty acids have many bioactive properties. Future studies are needed to investigate the mechanisms for regulation of DHA, EPA and other fatty acid levels within tissues.
No one tissue provided a good representation of the fatty acid or sterol content of the other tissues before or after LE infusion. This finding is important and has clinical implications. Many clinicians and investigators use plasma, RBC, or adipose tissue samples to approximate tissue levels of fatty acids. Our results suggest that these samples may not adequately reflect fatty acid content of different tissues. Thus, the effects of fatty acid cellular content and alterations upon organ functions likely require measurement of levels in the organ or organelle of interest. The clinical significance of the changes in fatty acids and the regulation (i.e., uptake, storage, and metabolism) of fatty acids remains unclear and requires further study.
Results of this study demonstrate changes in liver tissue within 6 hours of lipid infusion. For example, oleic acid increased in liver following OOSO and FOCS infusion; linoleic acid increased in liver following SO infusion and decreased following FO infusion; EPA and DHA increased in liver following FO and FOCS infusion. These liver changes preceded changes in RBC. The results indicate that fatty acid content of some tissues change within a few hours of intravenous infusion of lipids.
Plasma phytosterol levels (β-sitosterol and campesterol) were increased in the SO, OOSO, and FOCS groups compared to controls following both acute and chronic LE infusions. Plasma levels were not increased following FO infusion. The increase in plasma phytosterol levels reflected the content of the LE. The most common phytosterols in plasma were β-sitosterol and campesterol. Stigmasterol was not detected. Although phytosterol levels increased in plasma following chronic administration of SO, OOSO, and FOCS emulsions, tissue levels were more variable. These results indicate that phytosterols deposit in most tissues; however, it remains unclear whether the levels cause dysfunction of the various tissues. We found no differences between study groups for alkaline phosphatase, AST, ALT, or total bilirubin following infusion of the LE. We also failed to detect any evidence of increased lipid deposition in the liver (using oil red staining) or liver damage following either acute or chronic lipid administration.
One of the very interesting findings of the present investigation was the undetectable levels of stigmasterol in plasma and tissues of the animals receiving oral diets or LE in both the acute and chronic studies, despite the LE/diets having similar concentrations of campesterol and stigmasterol. It appears that stigmasterol did not get stored in tissues and was rapidly cleared (probably via biliary excretion) from the blood and tissues. This finding has importance since stigmasterol has been implicated in the etiology of cholestasis [10]. In support of our findings, Clayton et al [15] failed to detect stigmasterol in the plasma of hospitalized patients receiving oral diets (without liver disease). In contrast, human studies in both adults and neonates/children receiving long-term parenteral nutrition reveal elevated plasma levels of stigmasterol; however, levels of stigmasterol were significantly lower than levels of campesterol [15, 17, 20, 21]. Most long-term parenteral nutrition patients in these studies had evidence of cholestatic liver disease which may have contributed to the elevated stigmasterol levels. Further studies are needed to determine if phytosterols in LE cause cholestasis and to determine the mechanisms involved in liver and other organ dysfunction and/or toxicity.
The total mean phytosterol levels found in the plasma of the animals following 10 days of lipid infusion ranged from 2.09 to 7.18 µg/mL. These levels are similar to levels in healthy humans receiving western diets (i.e., 3–17 µg/mL) [5, 15, 17]. In addition, the total plasma phytosterol levels of the animals on the chow diet were also similar to normal human controls. In contrast, total plasma phytosterol levels were significantly higher in patients with intestinal failure receiving long-term parenteral nutrition [15, 17], where mean levels varied from 55.4 to 379 µg/mL. Many of these patients had evidence of cholestatic liver disease and it remains unclear whether the elevated levels are a cause or consequence of hepatobiliary dysfunction. Additional studies will need to be performed to determine if the levels of phytosterols found in tissues cause organ dysfunction. It is also unclear whether a longer duration of treatment would result in higher phytosterol levels or tissue dysfunction. It is important to note that animals in this study were consuming oral lipid-free diets which may limit phytosterol toxicity (perhaps by stimulating the enterohepatic circulation of bile acids).
A number of reports in the clinical literature have established the occurrence of liver disease in patients receiving long-term parenteral nutrition. The majority of the reports are in infants with underlying medical problems that include intestinal failure, recurrent sepsis, and inability to tolerate adequate enteral feeding. A smaller number of reports came from the adult population. The occurrence of liver disease in patients receiving parenteral nutrition is termed parenteral nutrition-associated liver disease (PNALD) [14, 22–24]. Current evidence supports a potential role for phytosterols as contributors to the development of PNALD [8–10, 12, 15]. The mechanisms by which phytosterols may cause liver disease are unclear. However, phytosterols inhibit enzymes involved in cholesterol and bile acid synthesis and metabolism, and also inhibit bile acid transporters involved in uptake and secretion of bile acids [10–12]. Infants may be particularly susceptible to liver injury induced by phytosterols due to reduced bile acid synthesis and immature biliary secretory systems [13]. The use of lower doses of SO [25–27] and substitution of FO-based emulsion [28] for SO emulsion (both result in decreased phytosterol intake) has been reported to improve liver disease and cholestasis in patients with PNALD.
The various study LE were chosen to allow for assessment of the range of variation of fatty acids and sterols that are produced in tissues when lipid varying in monounsaturated fatty acids, n-6 PUFA, and n-3 PUFA are administered. The LE represent four of the most common commercial LE used today for parenteral nutrition. The large variations of fatty acids in the different LE reflect the different oils used to manufacture the emulsions. For example, levels of oleic acid varied from 10.15 % in FO to 59.7 % in OOSO; levels of linoleic acid varied from 3 % in FO to 54.7 % in SO; levels of DHA varied from 0.06 % in OOSO to 17.7 % in FO. The different lipid emulsions also contain different quantities of phytosterols.
In preliminary experiments, we monitored oral diet intake in a group of guinea pigs receiving the 15 % fat diet (i.e., D10091201), which is a diet typical for these animals. We found that the guinea pigs consumed approximately 18 g of food/day which resulted in about 1 g fat intake per day and 209 Kcal/kg/day. Thus, we supplied similar quantities of fat and energy to the guinea pigs (5 mL of 20 % LE) during SO, OOSO and FOCS lipid infusion when the animals were kept on a fat free diet. The FO lipid was a 10 % emulsion (10 g/dL) and animals received less lipid energy (0.5 g/day as 5 mL/day). Despite the lower lipid content in the FO group, animals grew at similar rates and achieved similar body weights. Since we did not monitor oral intake of the fat free diet during chronic lipid infusion, it is possible that these animals compensated for the lower lipid calories and increased their food intake.
Since it is impossible to study the effects of the four study LE upon the tissue content of fatty acids and sterols in humans (requires tissue specimens), we chose the guinea pig as an animal model because the lipoprotein profile of guinea pigs, as opposed to other rodents, more closely resembles that of the human in terms of the low density lipoprotein cholesterol (LDL-C) and high density lipoprotein cholesterol (HDL-C) constituents [29]. Since clearance of lipids from the circulation and uptake by the tissues is dependent upon lipoprotein levels, the guinea pig represents a preferred rodent model for studying lipid metabolism, as their tissues express lipoprotein lipase and possess activities for intravascular processing of plasma lipoproteins [30]. Furthermore, the guinea pig shares with humans several other characteristics of lipid metabolism including high LDL-to-HDL ratio [31], higher concentrations of free than esterified cholesterol in the liver [32], response to exercise by decreasing TG and increasing HDL levels [33], and response to drug treatment by lowering plasma LDL-cholesterol concentrations [34, 35].
This study had a number of limitations. The study was designed to assess levels of fatty acids, squalene, and different sterols in LE and tissues of animals on oral diets and after 4 diverse lipid infusions. The study was not designed to compare oral with intravenous effects from the lipid emulsions. In addition, it was not designed to evaluate outcomes or tissue functions affected by the LE infusions. Functional effects require additional study. The study was also performed in healthy animals and results may be different with disease (especially hepatobiliary disease). The commercial lipid emulsions varied in concentration with SO, OOSO, and FOCS available as 20 % (20 g/dL) emulsions while the FO emulsion was a 10 % (10 g/dL) emulsion. We chose to administer equal volumes of the emulsions. As a result, the FO group received half the dose of lipid compared to the other lipid emulsion groups. As mentioned above, the lower lipid content was not associated with lower body and organ weights. FO is usually administered at lower doses than the other emulsions since it is approved as a lipid supplement rather than a complete lipid (i.e., low content of n-6 essential fatty acids). Oral intake was not recorded in the animals. It is possible that the FO group consumed greater amounts of the oral fat free diet to compensate for the reduced lipid intake. Finally, the chronic study was performed over a 10-day period, and results may vary with longer durations of study. However, it is difficult to maintain central venous access in rodents for longer durations.
In conclusion, the key findings of the present investigation are:
-
1.
Fatty acid/squalene/sterol contents of various tissues were highly variable and no one tissue adequately reflected the contents of the other tissues. The changes in liver occurred before changes in RBC.
-
2.
n-3 PUFA were found in low concentrations in all tissues; however, levels increased significantly following infusion of fish oil emulsion.
-
3.
Plasma and RBC were a poor reflection of tissue levels of squalene, cholesterol, and phytosterols. Squalene was highest in adipose tissue while total phytosterols were highest in lungs and adipose tissue after chronic administration of LE.
-
4.
β-Sitosterol and campesterol were the primary phytosterols detected in the tissues of the animals.
-
5.
Although stigmasterol was present in the diets and LE, stigmasterol was not detected in the tissues of the animals.
-
6.
Future studies should evaluate the functional consequences of the widely varying fatty acid and phytosterol contents of tissues in both health and disease.
Abbreviations
- ALP:
-
Alkaline phosphatase
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- CO:
-
Coconut oil
- DHA:
-
Docosahexaenoic acid
- DPA:
-
Docosapentaenoic acid
- EPA:
-
Eicosapentaenoic acid
- FO:
-
Fish oil emulsion
- FOCS:
-
Fish, olive, coconut and soybean oils emulsion
- OOSO:
-
Olive and soybean oils emulsion
- GC:
-
Gas chromatography
- HDL-C:
-
High density lipoprotein-cholesterol
- LCT:
-
Long-chain triacylglycerols
- LDL-C:
-
Low density lipoproteins-Cholesterol
- LDL-R:
-
Low density lipoprotein receptor
- LE:
-
Lipid emulsion
- LPL:
-
Lipoprotein lipase
- MCT:
-
Medium chain triacylglycerols
- PUFA:
-
Polyunsaturated fatty acids
- PNALD:
-
Parenteral-nutrition associated liver disease
- RBC:
-
Red blood cells
- SO:
-
Soybean oil emulsion
- TG:
-
Triacylglycerols
References
Rustan AC, Drevon CA (2005) Fatty acids: Structures and properties. In: Encyclopedia of life sciences. John Wiley, pp 1-7
Gurr M, Harwood J, Frayn K (1989) Lipid biochemistry: an introduction. 5th edn. Blackwell Science, Oxford, UK
Xu Z, Harvey K, Pavlina T, Dutot G, Zaloga G, Siddiqui R (2011) An improved method for determining medium- and long-chain FAMEs using gas chromatography. Lipids 45:199–208
Xu Z, Harvey KA, Pavlina T, Dutot G, Hise M, Zaloga GP, Siddiqui RA (2012) Steroidal compounds in commercial parenteral lipid emulsions. Nutrients 4:904–921
Ostlund RE Jr (2002) Phytosterols in human nutrition. Annu Rev Nutr 22:533–549
Subbiah MT (1973) Dietary plant sterols: current status in human and animal sterol metabolism. Am J Clin Nutr 26:219–225
Salen G, Ahrens EH Jr, Grundy SM (1970) Metabolism of beta-sitosterol in man. J Clin Invest 49:952–967
El Kasmi KC, Anderson A, Devereaux MW, Noe MS, Sokol RJ (2011) Soy lipid-derived phytosterols are responsible for parenteral nutrition associated liver injury (PNALI) in a mouse model. Hepatology 54(suppl):412A
Iyer KR, Spitz L, Clayton P (1998) New insight into mechanisms of parental nutrition-associated cholestasis: role of plant sterols. Journal of Pediatric Surgery 33:1–6
Carter BA, Taylor OA, Prendergast DR, Zimmerman TL, Von Furstenberg R, Moore DD, Karpen SJ (2007) Stigmasterol, a soy lipid-derived phytosterol, is an antagonist of the bile acid nuclear receptor FXR. Pediatr Res 62:301–306
Shefer S, Salen G, Nguyen L, Batta AK, Packin V, Tint GS, Hauser S (1988) Competitive inhibition of bile acid synthesis by endogenous cholestanol and sitosterol in sitosterolemia with xanthomatosis. Effect on cholesterol 7 alpha-hydroxylase. J Clin Invest 82:1833–1839
Boberg KM, Akerlund JE, Bjorkhem I (1989) Effect of sitosterol on the rate-limiting enzymes in cholesterol synthesis and degradation. Lipids 24:9–12
Clayton PT, Whitfield P, Iyer K (1998) The role of phytosterols in the pathogenesis of liver complications of pediatric parenteral nutrition. Nutrition 14:158–164
Kelly DA (2010) Preventing parenteral nutrition liver disease. Early Hum Dev 86:683–687
Clayton PT, Bowron A, Mills KA, Massoud A, Casteels M, Milla PJ (1993) Phytosterolemia in children with parenteral nutrition-associated cholestatic liver disease. Gastroenterology 105:1806–1813
Ellegard L, Sunesson A, Bosaeus I (2005) High serum phytosterol levels in short bowel patients on parenteral nutrition support. Clin Nutr 24:415–420
Llop JM, Virgili N, Moreno-Villares JM, Garcia-Peris P, Serrano T, Forga M, Solanich J, Pita AM (2008) Phytosterolemia in parenteral nutrition patients: implications for liver disease development. Nutrition 24:1145–1152
Clinolipid (lipid injectable emulsion, USP), 20 % - Accessdata FDA. WWW.accessdata.fda.gov
Team RDC (2008) R: A language and environment for statistical computing. Austria, Vienna
Hallikainen M, Huikko L, Kontra K, Nissinen M, Piironen V, Miettinen T, Gylling H (2008) Effect of parenteral serum plant sterols on liver enzymes and cholesterol metabolism in a patient with short bowel syndrome. Nutr Clin Pract 23:429–435
Dimakou K, Guillotte C, Hill S Phytosterols of HPN patients. In: The 34th ESPEN Congress, Barcelona, Spain, 2012. Clinical Nutrition Supplements, p 135
Beale EF, Nelson RM, Bucciarelli RL, Donnelly WH, Eitzman DV (1979) Intrahepatic cholestasis associated with parenteral nutrition in premature infants. Pediatrics 64:342–347
Van Aerde JE, Duerksen DR, Gramlich L, Meddings JB, Chan G, Thomson AB, Clandinin MT (1999) Intravenous fish oil emulsion attenuates total parenteral nutrition-induced cholestasis in newborn piglets. Pediatr Res 45:202–208
Nehra D, Fallon EM, Puder M (2011) The prevention and treatment of intestinal failure-associated liver disease in neonates and children. Surg Clin North Am 91:543–563
Cober MP, Killu G, Brattain A, Welch KB, Kunisaki SM, Teitelbaum DH (2012) Intravenous fat emulsions reduction for patients with parenteral nutrition-associated liver disease. J Pediatr 160:421–427
Allardyce DB (1982) Cholestasis caused by lipid emulsions. Surg Gynecol Obstet 154:641–647
Cavicchi M, Beau P, Crenn P, Degott C, Messing B (2000) Prevalence of liver disease and contributing factors in patients receiving home parenteral nutrition for permanent intestinal failure. Ann Intern Med 132:525–532
Puder M, Valim C, Meisel JA, Le HD, de Meijer VE, Robinson EM, Zhou J, Duggan C, Gura KM (2009) Parenteral fish oil improves outcomes in patients with parenteral nutrition-associated liver injury. Ann Surg 250:395–402
Fernandez ML (2001) Guinea pigs as models for cholesterol and lipoprotein metabolism. J Nutr 131:10–20
Olivecrona T, Bengsston-Olivecrona G (1993) Lipoprotein lipase and hepatic lipase. Curr Opin Lipidiol 4:187–196
Fernandez ML, Yount NY, McNamara DJ (1990) Whole body and hepatic cholesterol synthesis rates in the guinea-pig: effect of dietary fat quality. Biochim Biophys Acta 1044:340–348
Angelin B, Olivecrona H, Reihner E, Rudling M, Stahlberg D, Eriksson M, Ewerth S, Henriksson P, Einarsson K (1992) Hepatic cholesterol metabolism in estrogen-treated men. Gastroenterology 103:1657–1663
McNamara DJ, Ensign W, Montano C, D.M. S, Soscia A (1993) Exercise and plasma lipoproteins in the guinea pig. Faseb J:A869
Hidaka K, Takada Y, Matsunaga A, Sasaki J, Arakawa K (1992) Effects of probucol on low-density lipoprotein catabolism in guinea pigs. Artery 19:162–176
Berglund L, Sharkey MF, Elam RL, Witztum JL (1989) Effects of lovastatin therapy on guinea pig low density lipoprotein composition and metabolism. J Lipid Res 30:1591–1600
Suckow MA, Stevens KA, Wilson RP (2012) The laboratory rabbit, guinea pig, hamster, and other rodents. Academic Press, Salt Lake City, UT
Acknowledgments
The authors wish to thank Elaine Bammerlin for providing editorial assistance and Dr. Cary Mariash for the statistical analysis of data. This study was supported by a grant from Baxter Healthcare Corporation, Deerfield, IL 60015, USA.
Conflict of interest
All authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Harvey, K., Xu, Z., Walker, C. et al. Parenteral Lipid Emulsions in Guinea Pigs Differentially Influence Plasma and Tissue Levels of Fatty Acids, Squalene, Cholesterol, and Phytosterols. Lipids 49, 777–793 (2014). https://doi.org/10.1007/s11745-014-3927-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11745-014-3927-2