Abstract
Observational evidence suggests that in populations consuming low levels of n-3 highly unsaturated fatty acids, women have higher blood levels of docosahexaenoic acid (DHA; 22:3n-6) as compared with men. Increased conversion of alpha-linolenic acid (ALA; 18:3n-3) to DHA by females has been confirmed in fatty acid stable isotope studies. This difference in conversion appears to be associated with estrogen and some evidence indicates that the expression of enzymes involved in synthesis of DHA from ALA, including desaturases and elongases, is elevated in females. An estrogen-associated effect may be mediated by peroxisome proliferator activated receptor-α (PPARα), as activation of this nuclear receptor increases the expression of these enzymes. However, because estrogens are weak ligands for PPARα, estrogen-mediated increases in PPARα activity likely occur through an indirect mechanism involving membrane-bound estrogen receptors and estrogen-sensitive G-proteins. The protein kinases activated by these receptors phosphorylate and increase the activity of PPARα, as well as phospholipase A2 and cyclooxygenase 2 that increase the intracellular concentration of PPARα ligands. This review will outline current knowledge regarding elevated DHA production in females, as well as highlight interactions between estrogen signaling and PPARα activity that may mediate this effect.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The dietary intake and blood content of omega-3 polyunsaturated fatty acids (n-3 PUFA, ≥18 carbons, ≥2 double bonds), particularly the highly unsaturated fatty acids (HUFA, ≥20 carbons, ≥3 carbon–carbon, double bonds) eicosapentaenoic acid (EPA, 20:5n-3) and docosahexaenoic acid (DHA, 22:3n-3), are associated with a reduced risk of sudden cardiac death when incorporated into cardiac membranes as phospholipids or free fatty acids [1–4]. Also, the incorporation of DHA into brain phospholipids is associated with improved neurological development [5] and performance on spatial tasks [6]. EPA and DHA can either be obtained directly from the diet or produced within the body from dietary precursors such as alpha-linolenic acid (ALA, 18:3n-3). As reviewed recently, it appears that in humans, increasing ALA intakes can significantly increase levels of EPA and n-3 docosapentaenoic acid (DPAn-3), but not DHA in various blood measures [7]. However, even limited production of EPA, DPAn-3 and DHA from dietary ALA may be clinically relevant. The anti-arrhythmic benefit of EPA and DHA is estimated to have a very steep dose–response curve that plateaus at an EPA + DHA consumption of 750 mg/day [8], much higher than the estimated North American intakes of EPA + DHA of approximately 100 mg/day [9–12]. It has recently been suggested that 250–500 mg/day of EPA + DHA should be established as a dietary reference intake [13]. Therefore, even a small contribution to tissue EPA and DHA through ALA conversion could have a significant impact on sudden cardiac death risk reduction.
Dietary ALA intakes are inversely associated with sudden cardiac death in women [14] but not in men [15] in North American populations. North American intakes of ALA are approximately 1,500 mg/day [9–12]. Increased ALA conversion to EPA and DHA has been observed in women consuming <200 mg EPA + DHA/day as compared with men and women consuming >500 mg EPA + DHA/day [16, 17] and may partially explain the inverse association with sudden cardiac death. Increased conversion of ALA to DHA [16, 18, 19] and higher levels of DHA in various lipid fractions of liver, erythrocytes, plasma and whole blood [16, 20–24] have been observed in females consuming typical Western diets as compared with males.
An increased capacity to biosynthesize DHA in women is possibly an evolutionary adaptation to attempt to provide a supply of DHA for maternal–fetal transport during the fetal brain growth spurt [7, 12, 25]. Observational results suggest that pregnant women undergo metabolic adaptations to maintain DHA in blood for placental transport [12, 26–28]. Changes in n-3 HUFA have also been associated with both endogenous and exogenous changes in circulating estrogen [21, 29–32], however, the potential mechanisms for this enhanced biosynthesis has not been elucidated.
The biosynthesis of DHA is mediated by elongases and desaturases in the endoplasmic reticulum and acyl-CoA oxidase and multifunctional protein 2 in the peroxisome. Estrogen-response elements have not been associated with the genes of any of these enzymes to date despite our efforts (unpublished observations). This is despite the fact that estrogen response elements are well characterized [33] and can be identified using a variety of tools. Peroxisome-proliferator receptor α (PPARα), a nuclear receptor that increases the expression of desaturases [34, 35] is a potential target for an estrogen mediated effect, but it also lacks an estrogen response element [36]. However, PPARα activity may be increased by indirect estrogen mediated phosphorylation. Several of the protein kinase systems activated by membrane-bound estrogen receptors, including mitogen-activated protein kinase (MAPK) and protein kinase A, phosphorylate and increase the activity of PPARα [37–39]. We presently review evidence supporting sex differences in the conversion of ALA to DHA and suggest a potential mechanism involving interaction between PPARα and estrogen signaling.
Dietary Sources of DHA
Preformed DHA
Blood levels of DHA are strongly correlated with the dietary intake of DHA [40]. In North America, salmon is a dominant source of dietary EPA and DHA due to its high popularity (ranked 4th in consumption frequency among marine foods after shrimp, tuna and breaded fish, respectively), and a high content of EPA and DHA [8, 9, 41]. Salmon provides 1,100–2,100 mg EPA + DHA/100 g as compared with 130–860 mg from tuna, 320–550 mg from shrimp, and 0–210 mg from breaded fish (per 100 g cooked) [42]. Alternative sources that can provide significant amounts of dietary n-3 HUFA include fish oil capsules and novel EPA and DHA enriched functional foods [43, 44]. All these strategies are largely dependent on fish stocks and fish-farming practices that may not be sustainable [45]. Non-fish sources of preformed dietary DHA include fat extraction from species of microalgae such as Crypthecodinium cohnii and Schizochytrium [46, 47]. The production of DHA by microalgae varies with some species relying on alternating desaturases and elongases while others utilize polyketide synthase systems [48, 49]. There are ongoing efforts to develop genetically modified organisms capable of producing n-3 HUFA [50, 51].
Dietary Precursors of DHA
The primary dietary precursor of long chain n-3 PUFA that is consumed in North America is ALA, which is found in a variety of plant foods and oils, particularly in flaxseed oil. Canola and soybean oil also contain significant amounts of ALA, but also typically contain relatively higher amounts of linoleic acid (LNA, 18:2n-6). Supplementing with relatively low levels of dietary ALA (2.4 g ALA/day in flaxseed oil) can increase erythrocyte EPA [52] with higher doses of ALA resulting in further increases in blood levels of EPA and DPAn-3, but often not DHA as reviewed extensively [7]. There is no evidence that ALA interventions result in increased DHA in blood, however these studies have been done predominantly with males only [52–55] or with mixed sex groups without specific sex group analyses [56–59]. Recently, we demonstrated that DHA levels in free living females was significantly higher than free living males, and that increases in DHA status is much slower than changes in EPA with fish oil supplementation [24]. Therefore, acute intervention studies may not be appropriate to detect DHA biosynthesis and accumulation in human blood. There are some longer ALA intervention studies that suggest DHA blood measures may possibly increase (for example, 52 weeks) [60]. It is also important to note that blood measures of EPA, DPAn-3, and DHA may only reflect hepatic ALA conversion, while there is evidence suggesting tissue specific ALA conversion with brain capable of synthesizing DHA from ALA, while the heart appears to only convert ALA to EPA and DPAn-3 [61].
Mammalian DHA Biosynthesis
The discovery that dietary ALA was the precursor of DHA was made in 1950 by Widmer and Holman [62] by feeding fat-deficient rats isolated ALA and observing the tissue deposition of DHA. Klenk and Mohrhauer [63] later elucidated the pathway of DHA formation from ALA to be: 18:3n-3 → 18:4n-3 → 20:4n-3 → 20:5n-3 → 22:5n-3 → 22:6n-3. It was then determined that the pathway took place in the endoplasmic reticulum [64]. Testing of the assumption that a delta-4 desaturase was responsible for the conversion of 22:5n-3 into 22:6n-3 revealed no microsomal formation of 22:6n-3, but rather two novel fatty acids were microsomally produced: 24:5n-3 and 24:6n-3 [65]. It was later determined that 22:6n-3 was formed by peroxisomal β-oxidation of the microsomally produced 24:6n-3 (Fig. 1) [66].
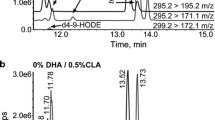
Two main metabolic fates of alpha-linolenic acid: conversion to longer-chain n-3 polyunsaturated fatty acids in the endoplasmic reticulum and peroxisomes, and mitochondrial oxidation. ALA alpha-linolenic acid, D6D delta-6 desaturase, FADS fatty acid desaturase, ELOVL elongase of very long chain fatty acids, EPA eicosapentaenoic acid, D5D delta-5 desaturase, DPA docosapentaenoic acid, DHA docosahexaenoic acid
The first enzyme in the conversion of ALA to longer chain n-3 HUFA is delta-6 desaturase (D6D) [67]. D6D catalyzes the desaturation of both n-6 and n-3 PUFA, and also appears to act on both 18- and 24-carbon PUFA, representing a significant metabolic “bottle-neck” [68]. A D6D knockout mouse has been demonstrated to lack the ability to make arachidonic acid (20:4n-6) from LNA and to lack the ability to make docosapentaenoic acid (22:5n-6) from dietary arachidonic acid [69]. In addition, the competition between ALA and 24:5n-3 for D6D results in EPA accumulation and limited synthesis and accumulation of DHA in Hep-G2 phospholipids [70]. As a result, the expression and activity of D6D, and substrate competition are considered primary determinants of DHA production rate. However, the large induction of both D6D and delta-5 desaturase (D5D), but not elongases, observed in HepG2 cells in response to essential fatty acid deficiency suggests that HUFA production is dependent on the concentration of both of these enzymes [71]. Additionally, these two genes are located only 11 kb apart on chromosome 11 in humans (chromosome 19 in mice) in a head-to-head orientation, suggesting that the transcription of these two genes may be regulated similarly [67]. A thorough review of the desaturases is available [67].
Sex Differences in DHA Status and Metabolism
Several studies have observed sex differences in blood and tissue DHA content in humans and rats (summarized in Table 1). While consuming a habitual diet, women possess significantly higher levels of DHA in total plasma lipids, as well as plasma non-esterified fatty acids, triacylglycerols, and phosphatidyl choline [23]. Sex specific responses to fish-oil supplementation have been observed including higher levels of DHA in erythrocytes and whole blood at baseline and after 8 weeks washout post-supplementation in women as compared with men [24]. Also, female sex has been significantly associated with increased DHA in studies examining various lifestyle and physiological parameters on fingertip prick whole blood in Italians [72] and serum phospholipids and cholesteryl esters in New Zealanders [22]. Higher levels of DHA in the blood of women as compared with men could be the result of differences in DHA mobilization and partitioning, dietary intake and male–female differences in body mass rather than differences in biosynthesis. However, increased ALA to DHA conversion rates in women relative to men have been determined using fatty acid stable isotope tracer studies [16, 18, 19].
The net fractional conversion of an orally ingested bolus of U13C-ALA into EPA and DHA in women capable of bearing children has been observed to be approximately 21 and 9.1%, respectively [18] as compared with conversion rates in men of 7.9% for EPA and DHA production that was undetectable by the investigators means [19]. In these studies, 13C-EPA and DHA primarily appeared in plasma phosphatidyl choline. Labelled U13C-DHA has also been detected in plasma triacylglycerol and phospholipid fractions in women (no men comparison group) after treatment with dietary U13C-ALA [73]. Compartmentalized modeling of 2H-ALA metabolism through examining 2H-HUFA appearance in plasma total lipids has isolated the sex difference to the conversion of labeled 22:5n-3 to labeled 22:6n-3, and that this sex difference was present only when participants consumed a beef-based diet low in n-3 HUFA and not a fish-based diet [16, 17]. Additionally, there may be increased partitioning of ALA towards DHA synthesis in women, as oxidation and carbon-recycling of ALA into saturated and monounsaturated fatty acids are much lower as compared with men [18, 19, 74]. In animal models, elevated DHA has also been observed in the liver phosphatidyl choline and phosphatidyl ethanolamine of mature female relative to male rats [20] and feeding male rats a high-ALA diet containing no EPA or DHA results in elevated liver and heart phospholipid EPA and DPAn-3, but not DHA [75].
In a model of dietary n-3 repletion, increased hepatic expression of D5D and D6D was observed in female rats as compared with male rats that corresponded to higher D5D protein content [76]. An increased expression of D5D only [20] and no differences in D5D and D6D [77] have also been reported. We have observed increased D5D and D6D mRNA expression in females as compared with males at 14 week of age on a standard chow diet (Kitson and Stark, unpublished observations). These results tend to suggest a greater capacity for DHA biosynthesis in females as compared with males. Sexual maturity may contribute to some of the disparity in these studies but this has not been elucidated.
Age may influence DHA accumulation [78]. There are reports of an association between age and DHA levels in adult human blood. Although dietary intake of DHA is a potential confounder, age was positively associated with DHA in plasma phospholipids [79, 80], serum phospholipids and cholesteryl esters [22], plasma total lipids [40] and erythrocytes [40, 81] after controlling for DHA intakes. However, no differences in DHA content between subjects over 75 years of age and control subjects between 20 and 48 years of age were observed in plasma phospholipids, non-esterified fatty acids, triacylglycerides, cholesteryl esters, and erythrocytes [82]. To our knowledge, a direct examination of the effect of age and sex on biosynthesis and accumulation of DHA has not been completed.
Role of Estrogen in DHA Biosynthesis
Sex differences in DHA levels appear to be mediated by circulating sex hormones, particularly estrogen (studies investigating hormone status or hormone manipulations, and DHA are summarized in Table 2). Elevated DHA content of female blood is possibly an evolutionary adaptation meant to provide fetal tissues with sufficient DHA for neural development. During pregnancy, the concentration of DHA in maternal blood is significantly elevated in the third trimester, when circulating levels of estrogen are highest [12, 26, 83]. Presumably, this increase in maternal DHA supports the fetal brain growth spurt in the third trimester, as the fetus’ capacity to produce DHA from ALA may be insufficient to meet the extreme demand [25, 84]. With postpartum, maternal estrogen and circulating maternal DHA levels decrease [12, 26].
Blood levels of DHA have been associated with exogenous sex hormone interventions. Postmenopausal women have been observed to have decreased DHA in erythrocyte phospholipids [85], and postmenopausal women undergoing hormone replacement strategies including both direct hormone replacement and selective estrogen-receptor modulators have increased circulating DHA relative to postmenopausal women not using hormone therapies [86, 87]. Women taking an estradiol-based contraceptive pill also have elevated blood and erythrocyte DHA levels as compared to women not taking oral contraceptives [21, 88]. Similarly, DHA increased in the plasma cholesteryl esters of male-to-female transsexuals receiving oral ethinyl estradiol, while plasma cholesteryl ester DHA decreased in the blood of female-to-male transsexuals receiving testosterone treatment [21].
In rats, EPA and DHA in plasma phosphatidyl choline correlate strongly with female sex hormones (estrogen and progesterone), and plasma, liver, and adipose EPA and DHA content vary inversely with testosterone [89]. DHA in liver phospholipids and plasma phosphatidyl choline have been observed to be higher in females as compared with males after n-3 deficiency/repletion [76]. Higher DHA has also been seen in female rat plasma and liver phospholipids in different diets containing varying levels of total fat and ALA [77]. Decreased erythrocyte DHA has been observed after ovariectomization as compared with sham-operated controls [90]. In addition, neuroblastoma cells incubated with ALA and estradiol exhibit higher EPA and DPAn-3 in phosphatidyl ethanolamine and increased expression of D5D as compared with cells incubated with ALA alone [91, 92]. Interestingly, treating neuroblastoma cells with dehydrotestosterone decreases EPA and DHA in phosphatidyl ethanolamine, and decreases D5D expression [91].
Based on current evidence, it appears that sex influences the concentration of circulating DHA, resulting in higher levels in females. This difference is associated with estrogen, and appears to involve increased conversion of ALA to DHA, in particular the conversion of 22:5n-3–22:6n-3, and only during low dietary intake of n-3 HUFA. It is possible that estrogen may increase the concentration or activity of DHA synthesis enzymes, including desaturases, elongases, and peroxisomal β-oxidation enzymes resulting in enhanced DHA biosynthesis.
Estrogen Signalling Mechanisms
Estrogen exerts many effects on a variety of different tissue types, and its actions are mediated by both direct interaction with the genome and nongenomic mechanisms [93]. The effects of estrogen are mediated primarily by estrogen receptors (ERα and ERβ in mammals) which exhibit a variety of subcellular localizations depending on tissue type [94, 95]. For example, in endometrial cells, ERα is primarily found at the cell membrane, whereas in breast cancer cells it is in the nucleus [95].
In direct genomic estrogen signaling, the binding of estrogen to estrogen receptors results in dimerization with another estrogen receptor (ERα or ERβ) followed by binding to an estrogen response element in the promoter of a target gene, causing altered transcription of that gene. In “nongenomic” estrogen signaling, estrogen binds to and activates estrogen receptors anchored to the plasma membrane [96], or a G-protein known as G-protein receptor 30 (GPR30) [97]. Dimerization to another estrogen receptor can also occur with this mechanism [98], however the signal transduction that results from the activation of these membrane bound receptors involves a number of second messenger protein kinases and calcium signaling mechanisms, rather then direct genomic interaction (some are presented below, and are extensively reviewed in [93]).
The observational link between circulating estrogen and DHA production suggests that estrogen increases the expression of the enzymes involved in DHA production from shorter-chain n-3 PUFA. However, to our knowledge, no estrogen response elements have been identified to date that influence the expression of any of the genes involved in DHA synthesis (D6D, D5D, acyl-CoA oxidase), suggesting that the estrogen dependent induction of these genes occurs through indirect mechanisms. Several reliable techniques exist for determining the presence of estrogen response elements on any gene on a genome-wide basis [99, 100], however genome-wide screening for these elements in DHA-producing genes has not been reported.
Peroxisome Proliferator-Activated Receptor α (PPARα)
The structure, ligand-binding, DNA-binding and metabolic actions of PPARs have been reviewed [101, 102]. PPARs are ligand-activated transcription factors belonging to the nuclear steroid receptor superfamily. Inactive PPARs are bound to corepressor proteins which are released upon ligand binding to the PPAR through a conformational change to the PPAR. This conformational change allows the PPAR to bind to the retinoid-x-receptor and co-activator proteins that facilitate binding of the complex to DNA through a number of different mechanisms including histone acetylase activity [103]. This activated complex then interacts with peroxisome proliferator response elements (PPRE; nucleotide regions with an imperfect direct repeat-1 motif) in the promoter region of target genes, and gene transcription is modulated.
Three distinct PPARs have been discovered with varying tissue expression, genomic targets, and ligands: PPARα, PPARγ (PPARγ1 and PPARγ2 are produced from the same gene by different promoters), and PPARβ/δ. All three subtypes bind to the direct repeat-1 motif, however, each PPAR subtype distinguishes its targets by differences in the region directly upstream of this motif [101].
PPARα is expressed in metabolically active tissues such as liver, heart, kidney, skeletal muscle and brown adipose tissue [104, 105] and is known to regulate the expression of genes involved in PUFA desaturation (D6D, D5D) [35, 106], peroxisomal β-oxidation (acyl-CoA oxidase, D-bifunctional protein) [107, 108], and fatty acid transport (cytosolic fatty acid binding protein, fatty acid transport protein, acyl-CoA binding protein) [109, 110], all of which are involved in DHA formation (a review of PPARα responsive genes is available [111]). PPARα plays a large role in lipid homeostasis by increasing peroxisomal and mitochondrial β-oxidation rates, and producing energy and acetyl units for ketone body formation in periods of fasting and/or low carbohydrate intake [112].
Natural ligands for PPARα include PUFA (n-3 and n-6), monounsaturated fatty acids, and eicosanoids such as leukotriene B4 and hydroxyeicosatetraenoic acids [36]. Fibrates such as clofibrate, fenofibrate, and bezafibrate are synthetic ligands for PPARα and are effective lipid-lowering agents in humans, while in rodents fibrates cause increased hepatic peroxisome number, hepatomegaly, and carcinogenesis at higher doses [111].
PPARα can be phosphorylated at multiple sites, resulting in increased activity (reviewed in [113]). The mechanism by which phosphorylation increases PPARα activity has not been elucidated, however, some evidence suggests that phosphorylation of PPARα results in a decreased affinity for corepressor proteins [114]. This finding is significant, as it suggests that phosphorylated PPARα is more likely to be activated at a biological concentration of PPARα ligands, such as PUFA.
Estrogen and PPARα
There is strong evidence that estrogen signaling interacts with PPARα-dependent gene transcription particularly with regards to lipid metabolism. For example, mice deficient in aromatase, and therefore unable to synthesize estrogen, succumb to hepatic steatosis resulting from elevated hepatic lipid accumulation and deficient β-oxidation [115]. However, estrogen supplementation prevents this effect by increasing mitochondrial and peroxisomal β-oxidation rates via increased expression of mitochondrial and peroxisomal β-oxidation enzymes (acyl-CoA oxidase, medium chain acyl-CoA dehydrogenase) [115, 116], similar to the effect of PPARα activation. Additionally, the expression of stearoyl-CoA desaturase 1, a PPARα-induced gene, is significantly increased in female mouse livers and results in elevated hepatic oleate production [117]. Also, mitochondrial β-oxidation is increased in women but not in men fed a high oleate diet (31.4% of energy), indicating a sex difference in the metabolic response to oleate, a weak PPARα ligand [118]. Treating ovariectomized rats with 17β-estradiol increases PPARα content and expression of PPARα-dependent lipid oxidation genes in red gastrocnemius muscle [119]. Significant increases in the expression and transcriptional activity of PPARβ/δ, and an increase in the expression of lipid oxidation genes under transcriptional control of PPARα, independent of an increase in PPARα expression in liver, muscle, and adipose tissue has been demonstrated using a similar approach [120]. Reduced fat accumulation in female but not male mice has also been observed after treatment with phytol, a peroxisome proliferator [121].
The expression of fatty acid binding proteins (FABP), which is increased following PPARα activation [122], is also much higher in females than in males [123, 124]. FABP transports fatty acids to the nucleus and has been observed to co-localize with and possibly increasing the activity of PPARα in fibroblasts and primary mouse hepatocytes [125–127]. However, transient transfection of fibroblasts with FABPs decreased tetradecylthioacetic acid stimulated PPAR activity [128].
Similarly, estrogen administration causes peroxisome proliferation in the uropygial glands of male and female mallard ducks, accompanied by an increase in the peroxisome-dependent production of 3-hydroxy fatty acid diesters [129]. In humans, the rate of DHA retroconversion to EPA, a process dependent on peroxisomal activity, is increased in postmenopausal women receiving hormone replacement therapy as compared with postmenopausal women not receiving this treatment [30]. Additionally, phospholipids and long chain PUFA in the brain are increased in female but not male PPARβ knockout mice suggesting sexual dimorphisms and a role of PPARβ in paroxysmal acyl-CoA use in the brain [130]. Considerable differences exist in the response of PPARα and PPARβ/δ to some natural ligands (particularly 8(S)-HETE) [131], and that generalizing in vivo results between different PPARs should be done with caution. Nonetheless, it seems that sex differences exist in other PPARs, as well as PPARα.
In a transgenic luciferase-5×PPRE mouse, it was shown that liver exhibited significantly lower PPARα transcriptional activity in females as compared with males in response to oral fibrate administration, food withdrawal, and reversal of feeding schedule [132]. These sexual dimorphisms remained despite ovariectomization and castration that suggests gonadal hormones are not involved. These observations may also be a dependent on the presence of the 5 PPREs in this model as similar observations have not been confirmed in mice with intact genomes. However, this transgenic model does support the notion that sex differences exist in PPARα-dependent gene transcription. Similarly, male as compared with female mice express more PPARα-dependent genes in response to 2 weeks of daily oral trichloroethylene treatment, suggesting a sex specific response to exogenous activators of PPARα [133].
Observations in PPARα-null mice strongly illustrate the interaction between estrogen and PPARα. Normally, ovariectomization results in significant gains in adipose tissue mass, while subsequent treatment with exogenous estradiol relieves this effect. However, in PPARα-null mice, no significant changes in adipose tissue are observed upon ovariectomization and subsequent estradiol administration, suggesting that the effect estrogen has on fat oxidation is dependent on the presence of PPARα [134]. Circulating leptin concentrations decrease in PPARα-null mice as compared with control mice, with a sex-specific effect in the leptin response to feeding as leptin was increased in female PPARα-null mice as compared with male PPARα-null mice [135].
The evidence presented above infers that a significant biological interaction exists between estrogen signaling and PPARα activity, and is present in several animal models. Accordingly, understanding the mechanism by which estrogen regulates PPARα may provide a better understanding of observations of sexual dimorphisms in n-3 PUFA metabolism. Interestingly, in vitro ligand binding analysis has shown that 17-β estradiol is a weak direct activator of PPARα, suggesting that it is not a PPARα ligand [36]. However, many interactions exist between estrogen signaling and PPARα, including protein kinases and other mechanisms, which suggest that estrogen acts on PPARα indirectly.
Estrogen Increases PPARα Activity by Phosphorylation
It is known that the phosphorylation (and corresponding activity) of PPARα is enhanced by several of the protein kinase systems activated by membrane bound estrogen receptors. By phosphorylating PPARα, estrogen will enhance DHA formation by increasing the transcription of enzymes involved in this pathway (Fig. 2).
Proposed mechanism of increased peroxisome-proliferator activated receptor α phosphorylation by estrogen. ER estrogen receptor, ERK-MAPK extracellular receptor kinase-mitogen activated protein kinase, Pi inorganic phosphate, PPARα peroxisome-proliferator activated receptor α, ALA alpha-linolenic acid, DHA docosahexaenoic acid
Estrogen binding to membrane bound estrogen receptors activates extracellular receptor kinase-mitogen activated protein kinase (ERK-MAPK) in a variety of tissue types/cell lines. Injection of 17-β-estradiol increases ERK-MAPK activity in several rat brain structures [38] and the addition of estrogen to male derived hypothalamic nuclei in vitro results in significant elevations in the activity of MAPK [39]. Furthermore, the addition of estrogen to cultured muscle cells [136] and breast cancer cells [137] also results in elevated ERK-MAPK activity, illustrating that this effect is shared by a variety of tissues.
Phosphorylation and increased activity of PPARα resulting from MAPK-mediated signal transduction has been well documented in a variety of cellular processes. Hepatic PPARα is known to be phosphorylated at two serine residues in response to insulin signaling via the ERK-MAPK system, resulting in increased PPARα-dependent gene transcription [114, 138]. The incubation of cultured myotubes with adiponectin results in elevated activity of ERK-MAPK and corresponding phosphorylation of PPARα, resulting in increased target gene expression and lipid catabolism [139]. Similarly, phosphatidyl inositol supplementation also increases PPARα activity via ERK-MAPK-dependent phosphorylation in human hepatocyte cell lines [140], resulting in PPARα-dependent production and secretion of apolipoprotein A-1.
Estrogen also activates protein kinase A phosphorylation systems. In vitro research with hippocampal neurons indicates that estrogen causes significant protein kinase A activation that is dependent on the presence of membrane-bound estrogen receptors [37]. Estrogen has been observed to cause protein kinase A dependent phosphorylation of N-methyl-d-aspartic acid receptors in rat spinal neurons, lessening the perception of pain by the animal [141]. In rat liver tissue, estrogen interaction with GPR30 results in activated protein kinase A signal transduction and prevention of apoptosis following organ injury [142]. Activation of protein kinase A signaling by cholera toxin has also been shown to increase the phosphorylation and transcriptional activity of PPARα [143]. Protein kinase A phosphorylates several enzymes in lipid-utilization systems and metabolism, including diacylglycerol lipase in the brain [144].
Phosphorylation of 5′AMP-activated protein kinase has also been observed in response to 17β-estradiol supplementation in the skeletal muscle of ovariectomized rats. Lipid oxidation in white adipose tissue [145] and skeletal muscle [146] is increased during AMP-activated protein kinase (AMPK) activation, and it has been found that siRNA inhibition of PPARα prevents this response [146].
Phosphorylation of PPARα via activation of membrane bound estrogen receptors is likely similar to the estrogen mediated phosphorylation and increased activity of cAMP response element binding (CREB) protein. Activation of CREB protein results in the increased expression of anti-apoptotic proteins, including the Bcl-2 family [147]. It has been well established that estrogen binding to membrane bound estrogen receptors results in the phosphorylation and increased activity of CREB protein. The precise protein kinase that mediates this phosphorylation varies by tissue, as protein kinase A is responsible in ZR-75 breast cancer cells [148], and protein kinase B/Akt and ERK-MAPK mediate this response in neuronal cells [149]. The increased CREB protein activity that results from phosphorylation has anti-apoptotic effects in all cell types, indicating increased CREB protein-dependent transcription.
Increased Concentration of Intracellular PPARα Ligands
Despite not being a PPARα ligand, estrogen may increase the intracellular concentrations of effective PPARα ligands, particularly PUFA and eicosanoids (Fig. 3). PUFA are most often found in the inner membrane leaflet of cells, in the sn-2 position of phosphatidyl ethanolamine [150]. Hydrolytic release of PUFA from this position for cell signaling or eicosanoid synthesis is catalyzed by phospholipase A2 (PLA2). Upon phosphorylation, the activity and a calcium-dependent isoform of PLA2 (Ca2+-PLA2) is increased, and the enzyme becomes localized in the cell membrane and nuclear envelope regions. By localizing in these regions, Ca2+-PLA2 functions to release PUFA from biological membranes for cell signaling and eicosanoid synthesis.
Proposed mechanism by which estrogen increases intracellular concentration of ligands for peroxisome-proliferator activated receptor α. ER estrogen receptor, ERK-MAPK extracellular receptor kinase-mitogen activated protein kinase, Ca 2+ -PLA 2 calcium-dependent phospholipase A2, COX-2 cyclooxygenase-2, Pi inorganic phosphate, PUFA polyunsaturated fatty acids, PPARα peroxisome-proliferator activated receptor α, ALA alpha-linolenic acid, DHA docosahexaenoic acid
Similarly to PPARα, activation of the ERK-MAPK signaling cascade has been observed to phosphorylate Ca2+-PLA2 in HeLa cells [151, 152]. Because estrogen has been observed to activate the ERK-MAPK system [38], as well as IP3-dependent calcium signaling cascades [153–155], estrogen would be expected to increase the activity of Ca2+-PLA2. Indeed, in pregnant rats uterine Ca2+-PLA2 activity is elevated near gestation in response to increased estradiol concentrations [156]. Estradiol-administration also enhanced the activity of Ca2+-PLA2 of mussel (Mytilus galloprovincialis) blood cells [157].
Eicosanoids are known to be involved in atherosclerosis, bronchial asthma, and many other inflammatory conditions [158]. Prostaglandins are produced in most tissue types, and are known to activate PPARα [36]. These cytokines are produced by enzymes known as cyclooxygenases (COX) of which there are two types: COX-1, which is constitutively expressed in most tissue types, and COX-2, the expression of which is induced during periods of inflammation. With regards to estrogen, increased COX-2 expression has been observed in response to elevated estrogen in human amnion, resulting in elevated prostaglandin E2 production [159].
Conclusions
The current knowledge of sex differences in n-3 PUFA metabolism is presently outlined and various likely mechanisms mediating the elevated n-3 HUFA synthesis observed in females have been indicated. Women have higher circulating concentrations of DHA as compared with men that is associated with estrogen, and is a result of increased conversion of ALA into DHA. This increased conversion likely involves the increased expression/activity of DHA synthesis enzymes, highlighting possible interaction between estrogen signaling mechanisms and the expression of enzymes responsible for the synthesis of DHA. Two likely mechanisms by which estrogen increases PPARα activity and subsequent DHA formation are presented: (1) estrogen increases the activity of ERK-MAPK and protein kinase A, which phosphorylate and increase the activity of PPARα, and/or (2) estrogen increases the intracellular concentration of both PUFA and eicosanoids, PPARα ligands, via elevated Ca2+-PLA2 and COX-2 activities, resulting in activation of PPARα. By increasing the activity of PPARα, estrogen likely causes elevated transcription of the enzymes involved in DHA synthesis, including desaturases, elongases, and peroxisomal β-oxidation enzymes. The increased activity of these enzymes results in the increased production of DHA, contributing to the elevated tissue DHA content observed in females.
A more complete understanding of these interactions is required to understand the health benefits of individual n-3 PUFA and to assist in the determination of dietary recommendations for ALA, EPA, DPAn-3 and DHA. The impact of hormonal status on n-3 PUFA metabolism may be important for DHA availability for maternal–fetal transport during pregnancy. In addition, subtle differences in DHA production may be contributing to observed sexual dimorphisms in sudden cardiac death. The interaction between estrogen and fatty acid metabolism requires further research including an examination of the effects of various gonadal hormones, the impact of fluctuations in hormones throughout the life cycle including physiological challenges such as pregnancy, and the impact of the dietary intake of specific fatty acids. In addition, an enhanced understanding of the regulation and control of DHA biosynthesis may assist in efforts to produce alternative food sources of DHA and aid in the challenge of meeting the potential global demand for EPA and DHA.
Abbreviations
- ALA:
-
Alpha-linoleic acid
- AMPK:
-
AMP-activated protein kinase
- Ca2+-PLA2 :
-
Calcium-dependent phospholipase A2
- CE:
-
Cholesteryl esters
- COX:
-
Cyclooxygenase
- CREB:
-
cAMP response element binding
- D5D:
-
Delta-5 desaturase
- D6D:
-
Delta-6 desaturase
- DHA:
-
Docosahexaenoic acid
- DPAn-3:
-
Docosapentaenoic acid, n-3
- ELOVL:
-
Elongase of very long chain fatty acids
- EPA:
-
Eicosapentaenoic acid
- ER:
-
Estrogen receptor
- ERK-MAPK:
-
Extracellular receptor kinase-mitogen activated protein kinase
- FABP:
-
Fatty acid binding proteins
- GPR30:
-
G-protein receptor 30
- HUFA:
-
Highly unsaturated fatty acids
- LNA:
-
Linoleic acid
- MAPK:
-
Mitogen-activated protein kinase
- PC:
-
Phosphatidyl choline
- PE:
-
Phosphatidyl ethanolamine
- PL:
-
Phospholipids
- PLA2 :
-
Phospholipase A2
- PPAR:
-
Peroxisome proliferator activated receptor
- PPRE:
-
Peroxisome proliferator response element
- PS:
-
Phosphatidyl serine
- PUFA:
-
Polyunsaturated fatty acids
References
Xiao YF, Sigg DC, Leaf A (2005) The antiarrhythmic effect of n-3 polyunsaturated fatty acids: modulation of cardiac ion channels as a potential mechanism. J Membr Biol 206:141–154
GISSI-Prevenzione Investigators (1999) Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: results of the GISSI-Prevenzione trial Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto miocardico. Lancet 354:447–455
Leaf A, Albert CM, Josephson M, Steinhaus D, Kluger J, Kang JX, Cox B, Zhang H, Schoenfeld D (2005) Prevention of fatal arrhythmias in high-risk subjects by fish oil n-3 fatty acid intake. Circulation 112:2762–2768
Leaf A, Xiao YF, Kang JX, Billman GE (2005) Membrane effects of the n-3 fish oil fatty acids, which prevent fatal ventricular arrhythmias. J Membr Biol 206:129–139
McCann JC, Ames BN (2005) Is docosahexaenoic acid, an n-3 long-chain polyunsaturated fatty acid, required for development of normal brain function? An overview of evidence from cognitive and behavioral tests in humans and animals. Am J Clin Nutr 82:281–295
Lim SY, Hoshiba J, Salem N Jr (2005) An extraordinary degree of structural specificity is required in neural phospholipids for optimal brain function: n-6 docosapentaenoic acid substitution for docosahexaenoic acid leads to a loss in spatial task performance. J Neurochem 95:848–857
Burdge GC, Calder PC (2005) Conversion of alpha-linolenic acid to longer-chain polyunsaturated fatty acids in human adults. Reprod Nutr Dev 45:581–597
Mozaffarian D, Rimm EB (2006) Fish intake, contaminants, and human health: evaluating the risks and the benefits. JAMA 296:1885–1899
Gebauer SK, Psota TL, Harris WS, Kris-Etherton PM (2006) n-3 Fatty acid dietary recommendations and food sources to achieve essentiality and cardiovascular benefits. Am J Clin Nutr 83:1526S–1535S
Denomme J, Stark KD, Holub BJ (2005) Directly quantitated dietary (n-3) fatty acid intakes of pregnant Canadian women are lower than current dietary recommendations. J Nutr 135:206–211
Fratesi JA, Hogg RC, Young-Newton GS, Patterson AC, Charkhzarin P, Block TK, Sharratt MT, Stark KD (2009) Direct quantitation of omega-3 fatty acid intake of Canadian residents of a long-term care facility. Appl Physiol Nutr Metab 34:1–9
Stark KD, Beblo S, Murthy M, Buda-Abela M, Janisse J, Rockett H, Whitty JE, Martier SS, Sokol RJ, Hannigan JH, Salem N Jr (2005) Comparison of bloodstream fatty acid composition from African-American women at gestation, delivery, and postpartum. J Lipid Res 46:516–525
Harris WS, Mozaffarian D, Lefevre M, Toner CD, Colombo J, Cunnane SC, Holden JM, Klurfeld DM, Morris MC, Whelan J (2009) Towards establishing dietary reference intakes for eicosapentaenoic and docosahexaenoic acids. J Nutr 139:804S–819S
Albert CM, Oh K, Whang W, Manson JE, Chae CU, Stampfer MJ, Willett WC, Hu FB (2005) Dietary alpha-linolenic acid intake and risk of sudden cardiac death and coronary heart disease. Circulation 112:3232–3238
Mozaffarian D, Ascherio A, Hu FB, Stampfer MJ, Willett WC, Siscovick DS, Rimm EB (2005) Interplay between different polyunsaturated fatty acids and risk of coronary heart disease in men. Circulation 111:157–164
Pawlosky R, Hibbeln J, Lin Y, Salem N Jr (2003) n-3 Fatty acid metabolism in women. Br J Nutr 90:993–994
Pawlosky RJ, Hibbeln JR, Lin Y, Goodson S, Riggs P, Sebring N, Brown GL, Salem N Jr (2003) Effects of beef- and fish-based diets on the kinetics of n-3 fatty acid metabolism in human subjects. Am J Clin Nutr 77:565–572
Burdge GC, Wootton SA (2002) Conversion of alpha-linolenic acid to eicosapentaenoic, docosapentaenoic and docosahexaenoic acids in young women. Br J Nutr 88:411–420
Burdge GC, Jones AE, Wootton SA (2002) Eicosapentaenoic and docosapentaenoic acids are the principal products of alpha-linolenic acid metabolism in young men. Br J Nutr 88:355–363
Burdge GC, Slater-Jefferies JL, Grant RA, Chung WS, West AL, Lillycrop KA, Hanson MA, Calder PC (2008) Sex, but not maternal protein or folic acid intake, determines the fatty acid composition of hepatic phospholipids, but not of triacylglycerol, in adult rats. Prostaglandins Leukot Essent Fatty Acids 78:73–79
Giltay EJ, Gooren LJ, Toorians AW, Katan MB, Zock PL (2004) Docosahexaenoic acid concentrations are higher in women than in men because of estrogenic effects. Am J Clin Nutr 80:1167–1174
Crowe FL, Skeaff CM, Green TJ, Gray AR (2008) Serum n-3 long-chain PUFA differ by sex and age in a population-based survey of New Zealand adolescents and adults. Br J Nutr 99:168–174
Bakewell L, Burdge GC, Calder PC (2006) Polyunsaturated fatty acid concentrations in young men and women consuming their habitual diets. Br J Nutr 96:93–99
Metherel AH, Armstrong JM, Patterson AC, Stark KD (2009) Assessment of blood measures of n-3 polyunsaturated fatty acids with acute fish oil supplementation and washout in men and women. Prostaglandins Leukot Essent Fatty Acids 81:23–29
Innis SM (2005) Essential fatty acid transfer and fetal development. Placenta 26 Suppl A:S70–S75
Stewart F, Rodie VA, Ramsay JE, Greer IA, Freeman DJ, Meyer BJ (2007) Longitudinal assessment of erythrocyte fatty acid composition throughout pregnancy and post partum. Lipids 42:335–344
Otto SJ, van Houwelingen AC, Badart-Smook A, Hornstra G (2001) Comparison of the peripartum and postpartum phospholipid polyunsaturated fatty acid profiles of lactating and nonlactating women. Am J Clin Nutr 73:1074–1079
Postle AD, Al MD, Burdge GC, Hornstra G (1995) The composition of individual molecular species of plasma phosphatidylcholine in human pregnancy. Early Hum Dev 43:47–58
Stark KD, Park EJ, Holub BJ (2003) Fatty acid composition of serum phospholipid of premenopausal women and postmenopausal women receiving and not receiving hormone replacement therapy. Menopause 10:448–455
Stark KD, Holub BJ (2004) Differential eicosapentaenoic acid elevations and altered cardiovascular disease risk factor responses after supplementation with docosahexaenoic acid in postmenopausal women receiving and not receiving hormone replacement therapy. Am J Clin Nutr 79:765–773
Oscarsson J, Eden S (1988) Sex differences in fatty acid composition of rat liver phosphatidylcholine are regulated by the plasma pattern of growth hormone. Biochim Biophys Acta 959:280–287
Burdge GC, Hunt AN, Postle AD (1994) Mechanisms of hepatic phosphatidylcholine synthesis in adult rat: effects of pregnancy. Biochem J 303(Pt 3):941–947
O’Lone R, Frith MC, Karlsson EK, Hansen U (2004) Genomic targets of nuclear estrogen receptors. Mol Endocrinol 18:1859–1875
Tang C, Cho HP, Nakamura MT, Clarke SD (2003) Regulation of human delta-6 desaturase gene transcription: identification of a functional direct repeat-1 element. J Lipid Res 44:686–695
Guillou H, Martin P, Jan S, D’Andrea S, Roulet A, Catheline D, Rioux V, Pineau T, Legrand P (2002) Comparative effect of fenofibrate on hepatic desaturases in wild-type and peroxisome proliferator-activated receptor alpha-deficient mice. Lipids 37:981–989
Krey G, Braissant O, L’Horset F, Kalkhoven E, Perroud M, Parker MG, Wahli W (1997) Fatty acids, eicosanoids, and hypolipidemic agents identified as ligands of peroxisome proliferator-activated receptors by coactivator-dependent receptor ligand assay. Mol Endocrinol 11:779–791
Shingo AS, Kito S (2005) Estradiol induces PKA activation through the putative membrane receptor in the living hippocampal neuron. J Neural Transm 112:1469–1473
Bryant DN, Bosch MA, Ronnekleiv OK, Dorsa DM (2005) 17-Beta estradiol rapidly enhances extracellular signal-regulated kinase 2 phosphorylation in the rat brain. Neuroscience 133:343–352
Gorosito SV, Cambiasso MJ (2008) Axogenic effect of estrogen in male rat hypothalamic neurons involves Ca(2+), protein kinase C, and extracellular signal-regulated kinase signaling. J Neurosci Res 86:145–157
Stark KD, Beblo S, Murthy M, Whitty JE, Buda-Abela M, Janisse J, Rockett H, Martier SS, Sokol RJ, Hannigan JH, Salem N Jr (2005) Alcohol consumption in pregnant, black women is associated with decreased plasma and erythrocyte docosahexaenoic acid. Alcohol Clin Exp Res 29:130–140
Mahaffey KR, Clickner RP, Jeffries RA (2008) Methylmercury and omega-3 fatty acids: co-occurrence of dietary sources with emphasis on fish and shellfish. Environ Res 107:20–29
Health Canada (2010) Canadian Nutrient File. http://webprod.hc-sc.gc.ca/cnf-fce/index-eng.jsp. Accessed Jan 2010
Patterson AC, Stark KD (2008) Direct determinations of the fatty acid composition of daily dietary intakes incorporating nutraceuticals and functional food strategies to increase n-3 highly unsaturated fatty acids. J Am Coll Nutr 27:538–546
Kitson AP, Patterson AC, Izadi H, Stark KD (2009) Pan-frying Salmon in an eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) enriched margarine prevents EPA and DHA loss. Food Chem 114:927–932
Jenkins DJ, Sievenpiper JL, Pauly D, Sumaila UR, Kendall CW, Mowat FM (2009) Are dietary recommendations for the use of fish oils sustainable? CMAJ 180:633–637
Hauvermale A, Kuner J, Rosenzweig B, Guerra D, Diltz S, Metz JG (2006) Fatty acid production in Schizochytrium sp.: involvement of a polyunsaturated fatty acid synthase and a type I fatty acid synthase. Lipids 41:739–747
Spolaore P, Joannis-Cassan C, Duran E, Isambert A (2006) Commercial applications of microalgae. J Biosci Bioeng 101:87–96
Chi X, Zhang X, Guan X, Ding L, Li Y, Wang M, Lin H, Qin S (2008) Fatty acid biosynthesis in eukaryotic photosynthetic microalgae: identification of a microsomal delta 12 desaturase in Chlamydomonas reinhardtii. J Microbiol 46:189–201
Meyer A, Cirpus P, Ott C, Schlecker R, Zahringer U, Heinz E (2003) Biosynthesis of docosahexaenoic acid in Euglena gracilis: biochemical and molecular evidence for the involvement of a delta4-fatty acyl group desaturase. Biochemistry 42:9779–9788
Damude HG, Kinney AJ (2007) Engineering oilseed plants for a sustainable, land-based source of long chain polyunsaturated fatty acids. Lipids 42:179–185
Damude HG, Zhang H, Farrall L, Ripp KG, Tomb JF, Hollerbach D, Yadav NS (2006) Identification of bifunctional delta12/omega3 fatty acid desaturases for improving the ratio of omega3 to omega6 fatty acids in microbes and plants. Proc Natl Acad Sci USA 103:9446–9451
Barcelo-Coblijn G, Murphy EJ, Othman R, Moghadasian MH, Kashour T, Friel JK (2008) Flaxseed oil and fish-oil capsule consumption alters human red blood cell n-3 fatty acid composition: a multiple-dosing trial comparing 2 sources of n-3 fatty acid. Am J Clin Nutr 88:801–809
Mantzioris E, James MJ, Gibson RA, Cleland LG (1994) Dietary substitution with an alpha-linolenic acid-rich vegetable oil increases eicosapentaenoic acid concentrations in tissues. Am J Clin Nutr 59:1304–1309
Li D, Sinclair A, Wilson A, Nakkote S, Kelly F, Abedin L, Mann N, Turner A (1999) Effect of dietary alpha-linolenic acid on thrombotic risk factors in vegetarian men. Am J Clin Nutr 69:872–882
Wallace FA, Miles EA, Calder PC (2003) Comparison of the effects of linseed oil and different doses of fish oil on mononuclear cell function in healthy human subjects. Br J Nutr 89:679–689
Sanders TA, Younger KM (1981) The effect of dietary supplements of omega 3 polyunsaturated fatty acids on the fatty acid composition of platelets and plasma choline phosphoglycerides. Br J Nutr 45:613–616
Cunnane SC, Hamadeh MJ, Liede AC, Thompson LU, Wolever TM, Jenkins DJ (1995) Nutritional attributes of traditional flaxseed in healthy young adults. Am J Clin Nutr 61:62–68
Finnegan YE, Minihane AM, Leigh-Firbank EC, Kew S, Meijer GW, Muggli R, Calder PC, Williams CM (2003) Plant- and marine-derived n-3 polyunsaturated fatty acids have differential effects on fasting and postprandial blood lipid concentrations and on the susceptibility of LDL to oxidative modification in moderately hyperlipidemic subjects. Am J Clin Nutr 77:783–795
Harper CR, Edwards MJ, DeFilippis AP, Jacobson TA (2006) Flaxseed oil increases the plasma concentrations of cardioprotective (n-3) fatty acids in humans. J Nutr 136:83–87
Bemelmans WJ, Broer J, Feskens EJ, Smit AJ, Muskiet FA, Lefrandt JD, Bom VJ, May JF, Meyboom-de JB (2002) Effect of an increased intake of alpha-linolenic acid and group nutritional education on cardiovascular risk factors: the Mediterranean Alpha-linolenic Enriched Groningen Dietary Intervention (MARGARIN) study. Am J Clin Nutr 75:221–227
Barcelo-Coblijn G, Murphy EJ (2009) Alpha-linolenic acid and its conversion to longer chain n-3 fatty acids: benefits for human health and a role in maintaining tissue n-3 fatty acid levels. Prog Lipid Res 48:355–374
Widmer C Jr, Holman RT (1950) Polyethenoid fatty acid metabolism; deposition of polyunsaturated fatty acids in fat-deficient rats upon single fatty acid supplementation. Arch Biochem 25:1–12
Klenk E, Mohrhauer H (1960) Studies on the metabolism of polyenoic fatty acids in the rat. Hoppe Seylers Z Physiol Chem 320:218–232
Nugteren DH (1965) The enzymic chain elongation of fatty acids by rat-liver microsomes. Biochim Biophys Acta 106:280–290
Voss A, Reinhart M, Sankarappa S, Sprecher H (1991) The metabolism of 7, 10, 13, 16, 19-docosapentaenoic acid to 4, 7, 10, 13, 16, 19-docosahexaenoic acid in rat liver is independent of a 4-desaturase. J Biol Chem 266:19995–20000
Luthria DL, Mohammed BS, Sprecher H (1996) Regulation of the biosynthesis of 4, 7, 10, 13, 16, 19-docosahexaenoic acid. J Biol Chem 271:16020–16025
Nakamura MT, Nara TY (2004) Structure, function, and dietary regulation of delta6, delta5, and delta9 desaturases. Annu Rev Nutr 24:345–376
Goyens PL, Spilker ME, Zock PL, Katan MB, Mensink RP (2006) Conversion of alpha-linolenic acid in humans is influenced by the absolute amounts of alpha-linolenic acid and linoleic acid in the diet and not by their ratio. Am J Clin Nutr 84:44–53
Stroud CK, Nara TY, Roqueta-Rivera M, Radlowski EC, Lawrence P, Zhang Y, Cho BH, Segre M, Hess RA, Brenna JT, Haschek WM, Nakamura MT (2009) Disruption of FADS2 gene in mice impairs male reproduction and causes dermal and intestinal ulceration. J Lipid Res 50:1870–1880
Portolesi R, Powell BC, Gibson RA (2007) Competition between 24:5n-3 and ALA for Delta 6 desaturase may limit the accumulation of DHA in HepG2 cell membranes. J Lipid Res 48:1592–1598
Melin T, Nilsson A (1997) Delta-6-desaturase and delta-5-desaturase in human Hep G2 cells are both fatty acid interconversion rate limiting and are upregulated under essential fatty acid deficient conditions. Prostaglandins Leukot Essent Fatty Acids 56:437–442
Marangoni F, Colombo C, Martiello A, Negri E, Galli C (2007) The fatty acid profiles in a drop of blood from a fingertip correlate with physiological, dietary and lifestyle parameters in volunteers. Prostaglandins Leukot Essent Fatty Acids 76:87–92
McCloy U, Ryan MA, Pencharz PB, Ross RJ, Cunnane SC (2004) A comparison of the metabolism of eighteen-carbon 13C-unsaturated fatty acids in healthy women. J Lipid Res 45:474–485
Burdge GC, Wootton SA (2003) Conversion of alpha-linolenic acid to palmitic, palmitoleic, stearic and oleic acids in men and women. Prostaglandins Leukot Essent Fatty Acids 69:283–290
Barcelo-Coblijn G, Collison LW, Jolly CA, Murphy EJ (2005) Dietary alpha-linolenic acid increases brain but not heart and liver docosahexaenoic acid levels. Lipids 40:787–798
Extier A, Langelier B, Perruchot MH, Guesnet P, Van Veldhoven PP, Lavialle M, Alessandri JM (2009) Gender affects liver desaturase expression in a rat model of n-3 fatty acid repletion. J Nutr Biochem. doi:10.1016/j.jnutbio.2008.10.008
Childs CE, Romeu-Nadal M, Burdge GC, Calder PC (2010) The polyunsaturated fatty acid composition of hepatic and plasma lipids differ by both sex and dietary fat intake in rats. J Nutr 140:245–250
Vandal M, Freemantle E, Tremblay-Mercier J, Plourde M, Fortier M, Bruneau J, Gagnon J, Begin M, Cunnane SC (2008) Plasma omega-3 fatty acid response to a fish oil supplement in the healthy elderly. Lipids 43:1085–1089
Dewailly EE, Blanchet C, Gingras S, Lemieux S, Sauve L, Bergeron J, Holub BJ (2001) Relations between n-3 fatty acid status and cardiovascular disease risk factors among Quebecers. Am J Clin Nutr 74:603–611
de Groot RH, van Boxtel MP, Schiepers OJ, Hornstra G, Jolles J (2009) Age dependence of plasma phospholipid fatty acid levels: potential role of linoleic acid in the age-associated increase in docosahexaenoic acid and eicosapentaenoic acid concentrations. Br J Nutr 102:1058–1064
Sands SA, Reid KJ, Windsor SL, Harris WS (2005) The impact of age, body mass index, and fish intake on the EPA and DHA content of human erythrocytes. Lipids 40:343–347
Babin F, Abderrazik M, Favier F, Cristol JP, Leger CL, Papoz L, Descomps B (1999) Differences between polyunsaturated fatty acid status of non-institutionalised elderly women and younger controls: a bioconversion defect can be suspected. Eur J Clin Nutr 53:591–596
Rump P, Otto SJ, Hornstra G (2001) Leptin and phospholipid-esterified docosahexaenoic acid concentrations in plasma of women: observations during pregnancy and lactation. Eur J Clin Nutr 55:244–251
Su HM, Huang MC, Saad NM, Nathanielsz PW, Brenna JT (2001) Fetal baboons convert 18:3n-3 to 22:6n-3 in vivo. A stable isotope tracer study. J Lipid Res 42:581–586
Tworek C, Muti P, Micheli A, Krogh V, Riboli E, Berrino F (2000) Fatty acid composition of the red blood cell membrane in relation to menopausal status. Ann Epidemiol 10:477
Giltay EJ, Duschek EJ, Katan MB, Zock PL, Neele SJ, Netelenbos JC (2004) Raloxifene and hormone replacement therapy increase arachidonic acid and docosahexaenoic acid levels in postmenopausal women. J Endocrinol 182:399–408
Sumino H, Ichikawa S, Murakami M, Nakamura T, Kanda T, Sakamaki T, Mizunuma H, Kurabayashi M (2003) Effects of hormone replacement therapy on circulating docosahexaenoic acid and eicosapentaenoic acid levels in postmenopausal women. Endocr J 50:51–59
Magnusardottir AR, Steingrimsdottir L, Thorgeirsdottir H, Gunnlaugsson G, Skuladottir GV (2009) Docosahexaenoic acid in red blood cells of women of reproductive age is positively associated with oral contraceptive use and physical activity. Prostaglandins Leukot Essent Fatty Acids 80:27–32
Childs CE, Romeu-Nadal M, Burdge GC, Calder PC (2008) Gender differences in the n-3 fatty acid content of tissues. Proc Nutr Soc 67:19–27
McNamara RK, Able J, Jandacek R, Rider T, Tso P (2009) Gender differences in rat erythrocyte and brain docosahexaenoic acid composition: role of ovarian hormones and dietary omega-3 fatty acid composition. Psychoneuroendocrinology 34:532–539
Extier A, Perruchot MH, Baudry C, Guesnet P, Lavialle M, Alessandri JM (2009) Differential effects of steroids on the synthesis of polyunsaturated fatty acids by human neuroblastoma cells. Neurochem Int 55:295–301
Alessandri JM, Extier A, Langelier B, Perruchot MH, Heberden C, Guesnet P, Lavialle M (2008) Estradiol favors the formation of eicosapentaenoic acid (20:5n-3) and n-3 docosapentaenoic acid (22:5n-3) from alpha-linolenic acid (18:3n-3) in SH-SY5Y neuroblastoma cells. Lipids 43:19–28
Bjornstrom L, Sjoberg M (2005) Mechanisms of estrogen receptor signaling: convergence of genomic and nongenomic actions on target genes. Mol Endocrinol 19:833–842
Ropero AB, Eghbali M, Minosyan TY, Tang G, Toro L, Stefani E (2006) Heart estrogen receptor alpha: distinct membrane and nuclear distribution patterns and regulation by estrogen. J Mol Cell Cardiol 41:496–510
Monje P, Zanello S, Holick M, Boland R (2001) Differential cellular localization of estrogen receptor alpha in uterine and mammary cells. Mol Cell Endocrinol 181:117–129
Acconcia F, Ascenzi P, Fabozzi G, Visca P, Marino M (2004) S-palmitoylation modulates human estrogen receptor-alpha functions. Biochem Biophys Res Commun 316:878–883
Filardo EJ, Quinn JA, Bland KI, Frackelton AR Jr (2000) Estrogen-induced activation of Erk-1 and Erk-2 requires the G protein-coupled receptor homolog, GPR30, and occurs via trans-activation of the epidermal growth factor receptor through release of HB-EGF. Mol Endocrinol 14:1649–1660
Razandi M, Pedram A, Merchenthaler I, Greene GL, Levin ER (2004) Plasma membrane estrogen receptors exist and functions as dimers. Mol Endocrinol 18:2854–2865
Kamalakaran S, Radhakrishnan SK, Beck WT (2005) Identification of estrogen-responsive genes using a genome-wide analysis of promoter elements for transcription factor binding sites. J Biol Chem 280:21491–21497
Sharov AA, Dudekula DB, Ko MS (2006) CisView: a browser and database of cis-regulatory modules predicted in the mouse genome. DNA Res 13:123–134
Berger J, Moller DE (2002) The mechanisms of action of PPARs. Annu Rev Med 53:409–435
Fruchart JC, Duriez P, Staels B (1999) Peroxisome proliferator-activated receptor-alpha activators regulate genes governing lipoprotein metabolism, vascular inflammation and atherosclerosis. Curr Opin Lipidol 10:245–257
Zhu Y, Qi C, Calandra C, Rao MS, Reddy JK (1996) Cloning and identification of mouse steroid receptor coactivator-1 (mSRC-1), as a coactivator of peroxisome proliferator-activated receptor gamma. Gene Expr 6:185–195
Braissant O, Foufelle F, Scotto C, Dauca M, Wahli W (1996) Differential expression of peroxisome proliferator-activated receptors (PPARs): tissue distribution of PPAR-alpha, -beta, and -gamma in the adult rat. Endocrinology 137:354–366
Palmer CN, Hsu MH, Griffin KJ, Raucy JL, Johnson EF (1998) Peroxisome proliferator activated receptor-alpha expression in human liver. Mol Pharmacol 53:14–22
Jump DB, Thelen A, Mater M (1999) Dietary polyunsaturated fatty acids and hepatic gene expression. Lipids 34 Suppl:S209–S212
Corton JC, Bocos C, Moreno ES, Merritt A, Cattley RC, Gustafsson JA (1997) Peroxisome proliferators alter the expression of estrogen-metabolizing enzymes. Biochimie 79:151–162
Chu R, Madison LD, Lin Y, Kopp P, Rao MS, Jameson JL, Reddy JK (1995) Thyroid hormone (T3) inhibits ciprofibrate-induced transcription of genes encoding beta-oxidation enzymes: cross talk between peroxisome proliferator and T3 signaling pathways. Proc Natl Acad Sci USA 92:11593–11597
Sandberg MB, Bloksgaard M, Duran-Sandoval D, Duval C, Staels B, Mandrup S (2005) The gene encoding acyl-CoA-binding protein is subject to metabolic regulation by both sterol regulatory element-binding protein and peroxisome proliferator-activated receptor alpha in hepatocytes. J Biol Chem 280:5258–5266
Martin G, Schoonjans K, Lefebvre AM, Staels B, Auwerx J (1997) Coordinate regulation of the expression of the fatty acid transport protein and acyl-CoA synthetase genes by PPARalpha and PPARgamma activators. J Biol Chem 272:28210–28217
Mandard S, Muller M, Kersten S (2004) Peroxisome proliferator-activated receptor alpha target genes. Cell Mol Life Sci 61:393–416
Nakamura MT, Cheon Y, Li Y, Nara TY (2004) Mechanisms of regulation of gene expression by fatty acids. Lipids 39:1077–1083
Burns KA, Vanden Heuvel JP (2007) Modulation of PPAR activity via phosphorylation. Biochim Biophys Acta 1771:952–960
Juge-Aubry CE, Hammar E, Siegrist-Kaiser C, Pernin A, Takeshita A, Chin WW, Burger AG, Meier CA (1999) Regulation of the transcriptional activity of the peroxisome proliferator-activated receptor alpha by phosphorylation of a ligand-independent trans-activating domain. J Biol Chem 274:10505–10510
Nemoto Y, Toda K, Ono M, Fujikawa-Adachi K, Saibara T, Onishi S, Enzan H, Okada T, Shizuta Y (2000) Altered expression of fatty acid-metabolizing enzymes in aromatase-deficient mice. J Clin Invest 105:1819–1825
Yoshikawa T, Toda K, Nemoto Y, Ono M, Iwasaki S, Maeda T, Saibara T, Hayashi Y, Miyazaki E, Hiroi M, Enzan H, Shizuta Y, Onishi S (2002) Aromatase-deficient (ArKO) mice are retrieved from severe hepatic steatosis by peroxisome proliferator administration. Hepatol Res 22:278–287
Lee KN, Pariza MW, Ntambi JM (1996) Differential expression of hepatic stearoyl-CoA desaturase gene 1 in male and female mice. Biochim Biophys Acta 1304:85–88
Kien CL, Bunn JY (2008) Gender alters the effects of palmitate and oleate on fat oxidation and energy expenditure. Obesity (Silver Spring) 16:29–33
Campbell SE, Mehan KA, Tunstall RJ, Febbraio MA, Cameron-Smith D (2003) 17beta-estradiol upregulates the expression of peroxisome proliferator-activated receptor alpha and lipid oxidative genes in skeletal muscle. J Mol Endocrinol 31:37–45
D’Eon TM, Souza SC, Aronovitz M, Obin MS, Fried SK, Greenberg AS (2005) Estrogen regulation of adiposity and fuel partitioning. Evidence of genomic and non-genomic regulation of lipogenic and oxidative pathways. J Biol Chem 280:35983–35991
Atshaves BP, Payne HR, McIntosh AL, Tichy SE, Russell D, Kier AB, Schroeder F (2004) Sexually dimorphic metabolism of branched-chain lipids in C57BL/6 J mice. J Lipid Res 45:812–830
Brandes R, Kaikaus RM, Lysenko N, Ockner RK, Bass NM (1990) Induction of fatty acid binding protein by peroxisome proliferators in primary hepatocyte cultures and its relationship to the induction of peroxisomal beta-oxidation. Biochim Biophys Acta 1034:53–61
Bass NM, Barker ME, Manning JA, Jones AL, Ockner RK (1989) Acinar heterogeneity of fatty acid binding protein expression in the livers of male, female and clofibrate-treated rats. Hepatology 9:12–21
Gorski J, Zendzian-Piotrowska M, Wolfrum C, Nawrocki A, Spener F (2000) Effect of sex and bezafibrate on incorporation of blood borne palmitate into lipids of rat liver nuclei. Mol Cell Biochem 214:57–62
Huang H, Starodub O, McIntosh A, Atshaves BP, Woldegiorgis G, Kier AB, Schroeder F (2004) Liver fatty acid-binding protein colocalizes with peroxisome proliferator activated receptor alpha and enhances ligand distribution to nuclei of living cells. Biochemistry 43:2484–2500
Hostetler HA, McIntosh AL, Atshaves BP, Storey SM, Payne HR, Kier AB, Schroeder F (2009) L-FABP directly interacts with PPARalpha in cultured primary hepatocytes. J Lipid Res 50:1663–1675
McIntosh AL, Atshaves BP, Hostetler HA, Huang H, Davis J, Lyuksyutova OI, Landrock D, Kier AB, Schroeder F (2009) Liver type fatty acid binding protein (L-FABP) gene ablation reduces nuclear ligand distribution and peroxisome proliferator-activated receptor-alpha activity in cultured primary hepatocytes. Arch Biochem Biophys 485:160–173
Helledie T, Antonius M, Sorensen RV, Hertzel AV, Bernlohr DA, Kolvraa S, Kristiansen K, Mandrup S (2000) Lipid-binding proteins modulate ligand-dependent trans-activation by peroxisome proliferator-activated receptors and localize to the nucleus as well as the cytoplasm. J Lipid Res 41:1740–1751
Bohnet S, Rogers L, Sasaki G, Kolattukudy PE (1991) Estradiol induces proliferation of peroxisome-like microbodies and the production of 3-hydroxy fatty acid diesters, the female pheromones, in the uropygial glands of male and female mallards. J Biol Chem 266:9795–9804
Rosenberger TA, Hovda JT, Peters JM (2002) Targeted disruption of peroxisomal proliferator-activated receptor beta (delta) results in distinct gender differences in mouse brain phospholipid and esterified FA levels. Lipids 37:495–500
Yu K, Bayona W, Kallen CB, Harding HP, Ravera CP, McMahon G, Brown M, Lazar MA (1995) Differential activation of peroxisome proliferator-activated receptors by eicosanoids. J Biol Chem 270:23975–23983
Ciana P, Biserni A, Tatangelo L, Tiveron C, Sciarroni AF, Ottobrini L, Maggi A (2007) A novel peroxisome proliferator-activated receptor responsive element-luciferase reporter mouse reveals gender specificity of peroxisome proliferator-activated receptor activity in liver. Mol Endocrinol 21:388–400
Nakajima T, Kamijo Y, Usuda N, Liang Y, Fukushima Y, Kametani K, Gonzalez FJ, Aoyama T (2000) Sex-dependent regulation of hepatic peroxisome proliferation in mice by trichloroethylene via peroxisome proliferator-activated receptor alpha (PPARalpha). Carcinogenesis 21:677–682
Kim BH, Won YS, Kim DY, Kim B, Kim EY, Yoon M, Oh GT (2009) Signal crosstalk between estrogen and peroxisome proliferator-activated receptor alpha on adiposity. BMB Rep 42:91–95
Lewitt MS, Brismar K (2002) Gender difference in the leptin response to feeding in peroxisome-proliferator-activated receptor-alpha knockout mice. Int J Obes Relat Metab Disord 26:1296–1300
Ronda AC, Buitrago C, Colicheo A, de Boland AR, Roldan E, Boland R (2007) Activation of MAPKs by 1alpha, 25(OH)2-vitamin D3 and 17beta-estradiol in skeletal muscle cells leads to phosphorylation of Elk-1 and CREB transcription factors. J Steroid Biochem Mol Biol 103:462–466
Migliaccio A, Di DM, Castoria G, de FA, Bontempo P, Nola E, Auricchio F (1996) Tyrosine kinase/p21ras/MAP-kinase pathway activation by estradiol-receptor complex in MCF-7 cells. EMBO J 15:1292–1300
Shalev A, Siegrist-Kaiser CA, Yen PM, Wahli W, Burger AG, Chin WW, Meier CA (1996) The peroxisome proliferator-activated receptor alpha is a phosphoprotein: regulation by insulin. Endocrinology 137:4499–4502
Yoon MJ, Lee GY, Chung JJ, Ahn YH, Hong SH, Kim JB (2006) Adiponectin increases fatty acid oxidation in skeletal muscle cells by sequential activation of AMP-activated protein kinase, p38 mitogen-activated protein kinase, and peroxisome proliferator-activated receptor alpha. Diabetes 55:2562–2570
Pandey NR, Renwick J, Misquith A, Sokoll K, Sparks DL (2008) Linoleic acid-enriched phospholipids act through peroxisome proliferator-activated receptors alpha to stimulate hepatic apolipoprotein A-I secretion. Biochemistry 47:1579–1587
Tang B, Ji Y, Traub RJ (2008) Estrogen alters spinal NMDA receptor activity via a PKA signaling pathway in a visceral pain model in the rat. Pain 137:540–549
Hsieh YC, Yu HP, Frink M, Suzuki T, Choudhry MA, Schwacha MG, Chaudry IH (2007) G protein-coupled receptor 30-dependent protein kinase A pathway is critical in nongenomic effects of estrogen in attenuating liver injury after trauma-hemorrhage. Am J Pathol 170:1210–1218
Lazennec G, Canaple L, Saugy D, Wahli W (2000) Activation of peroxisome proliferator-activated receptors (PPARs) by their ligands and protein kinase A activators. Mol Endocrinol 14:1962–1975
Rosenberger TA, Farooqui AA, Horrocks LA (2007) Bovine brain diacylglycerol lipase: substrate specificity and activation by cyclic AMP-dependent protein kinase. Lipids 42:187–195
Gaidhu MP, Fediuc S, Anthony NM, So M, Mirpourian M, Perry RL, Ceddia RB (2009) Prolonged AICAR-induced AMP-kinase activation promotes energy dissipation in white adipocytes: novel mechanisms integrating HSL and ATGL. J Lipid Res 50:704–715
Lee WJ, Kim M, Park HS, Kim HS, Jeon MJ, Oh KS, Koh EH, Won JC, Kim MS, Oh GT, Yoon M, Lee KU, Park JY (2006) AMPK activation increases fatty acid oxidation in skeletal muscle by activating PPARalpha and PGC-1. Biochem Biophys Res Commun 340:291–295
Wilson BE, Mochon E, Boxer LM (1996) Induction of bcl-2 expression by phosphorylated CREB proteins during B-cell activation and rescue from apoptosis. Mol Cell Biol 16:5546–5556
Castro-Rivera E, Samudio I, Safe S (2001) Estrogen regulation of cyclin D1 gene expression in ZR-75 breast cancer cells involves multiple enhancer elements. J Biol Chem 276:30853–30861
Alexaki VI, Charalampopoulos I, Kampa M, Nifli AP, Hatzoglou A, Gravanis A, Castanas E (2006) Activation of membrane estrogen receptors induce pro-survival kinases. J Steroid Biochem Mol Biol 98:97–110
Boon JM, Smith BD (2002) Chemical control of phospholipid distribution across bilayer membranes. Med Res Rev 22:251–281
Jupp OJ, Vandenabeele P, MacEwan DJ (2003) Distinct regulation of cytosolic phospholipase A2 phosphorylation, translocation, proteolysis and activation by tumour necrosis factor-receptor subtypes. Biochem J 374:453–461
Grewal S, Morrison EE, Ponnambalam S, Walker JH (2002) Nuclear localisation of cytosolic phospholipase A2-alpha in the EA.hy.926 human endothelial cell line is proliferation dependent and modulated by phosphorylation. J Cell Sci 115:4533–4543
Improta-Brears T, Whorton AR, Codazzi F, York JD, Meyer T, McDonnell DP (1999) Estrogen-induced activation of mitogen-activated protein kinase requires mobilization of intracellular calcium. Proc Natl Acad Sci USA 96:4686–4691
Chen Z, Yuhanna IS, Galcheva-Gargova Z, Karas RH, Mendelsohn ME, Shaul PW (1999) Estrogen receptor alpha mediates the nongenomic activation of endothelial nitric oxide synthase by estrogen. J Clin Invest 103:401–406
Marino M, Acconcia F, Bresciani F, Weisz A, Trentalance A (2002) Distinct nongenomic signal transduction pathways controlled by 17beta-estradiol regulate DNA synthesis and cyclin D(1) gene transcription in HepG2 cells. Mol Biol Cell 13:3720–3729
Farina MG, Billi S, Leguizamon G, Weissmann C, Guadagnoli T, Ribeiro ML, Franchi AM (2007) Secretory and cytosolic phospholipase A2 activities and expression are regulated by oxytocin and estradiol during labor. Reproduction 134:355–364
Burlando B, Marchi B, Panfoli I, Viarengo A (2002) Essential role of Ca2+-dependent phospholipase A2 in estradiol-induced lysosome activation. Am J Physiol Cell Physiol 283:C1461–C1468
Das UN (2007) A defect in the activity of Delta6 and Delta5 desaturases may be a factor in the initiation and progression of atherosclerosis. Prostaglandins Leukot Essent Fatty Acids 76:251–268
Spaziani EP, Lantz ME, Benoit RR, O’Brien WF (1996) The induction of cyclooxygenase-2 (COX-2) in intact human amnion tissue by interleukin-4. Prostaglandins 51:215–223
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kitson, A.P., Stroud, C.K. & Stark, K.D. Elevated Production of Docosahexaenoic Acid in Females: Potential Molecular Mechanisms. Lipids 45, 209–224 (2010). https://doi.org/10.1007/s11745-010-3391-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11745-010-3391-6