Abstract
Lysophosphatidylcholine (lysoPtdCho) is a component of oxidized low density lipoprotein, and is involved in the pathogenesis of atherosclerosis and inflammation. We studied the effects of lysoPtdCho on cytotoxicity, reactive oxygen species (ROS) production, activation of the extracellular signal-regulated kinase (ERK), mitogen-activated protein kinases and pro-inflammatory gene expression in RAW 264.7 murine macrophage cells. When cells were exposed to lysoPtdCho with various acyl chains in a culture medium containing 10% fetal bovine serum, only 1-linoleoyl (C18:2) lysoPtdCho showed a remarkable cytotoxicity, reaching the highest level at 24 h, and elicited ROS production, suggesting that oxidative stress might be implicated in the cytotoxicity of 1-linoleoyl (C18:2) lysoPtdCho. Presumably in support of this, antioxidants such as magnolol or trolox prevented 1-linoleoyl (C18:2) lysoPtdCho-induced cytotoxicity as well as ROS production, although only partially. Furthermore, the phosphorylation of ERK 1/2 and the expression of pro-inflammatory cytokines such as IL-1β, CCL2 and CCL5 were augmented by 1-linoleoyl (C18:2) lysoPtdCho. Meanwhile, there was no structural importance of the acyl chain for the cytotoxic action of lysoPtdCho during 10 min incubation in serum-free media. Taken together, it is suggested that in a serum-containing medium, 1-linoleoyl (C18:2) lysoPtdCho can cause a significant cytotoxicity through ROS production, probably accompanied by activation of ERK and induction of related inflammatory cytokines, in RAW 264.7 cells.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lysophosphatidylcholine (lysoPtdCho) is known to be generated from phosphatidylcholine by at least four enzymes, phospholipase A2, lipoprotein-specific phospholipase A2, lecithin/cholesterol acyltransferase or endothelial lipase [1, 2]. The cytoplasmic and secretory forms of PLA2 are up-regulated in ischemia and inflammation, and a lipoprotein-associated PLA2 is an independent risk factor for atherosclerotic complications [2]. Presumably in support of this, lysoPtdCho accumulates in tissues during ischemia and in plasma of inflammatory arthritis [3]. In addition, a considerable increase in lysoPtdCho content during the routine storage of some blood cells has been reported [4]. However, a part of the lysoPtdCho in plasma may be bound by serum albumin or lipoproteins [5], albeit with a relatively lower affinity than alpha-1 acid glycoprotein, a major acute phase protein in plasma [6]. Alternatively, lysoPtdCho can be transferred directly to cell membranes from some specified lipids such as oxidized low density lipoprotein [7]. According to previous reports [8], lysoPtdCho elicits various pro-inflammatory and atherogenic phenomena. As a part of inflammatory actions of lysoPtdCho, previous studies reported that lysoPtdCho brought about the superoxide production in neutrophils [9]. In addition, lysoPtdCho caused superoxide generation by activating NADPH oxidase (NOX) in nonphagocytic cells, particularly in vascular endothelial cells [10]. Saturated lysoPtdCho such as 1-palmitoyl (C16:0) lysoPtdCho and 1-stearoyl (C18:0) lysoPtdCho were more potent in elevating the intracellular calcium ion level in neutrophils than 1-oleoyl (C18:1) lysoPtdCho [9]. In mechanistic analyses of lysoPtdCho effect, the increase of cytosolic Ca2+ and the reactive oxygen species (ROS) level was accompanied by stimulation of mitogen-activated protein kinase (MAPK) pathways [11]. A growing body of evidence suggests that ROS contribute to cell death, in part, through effects on various cellular signaling pathways including the MAPK pathways [12]. In addition, lysoPtdCho treatment elicits production of IL-1β and MCP-1, proinflammatory cytokine, in human monocytes and rat aortic smooth muscle cells, respectively [13]. Further support for pro-inflammatory activity of lysoPtdCho is provided by the evidence of lysoPtdCho acting as a chemotactic factor for monocytes and T cells [14], and lysoPtdCho released by apoptotic cells has been proposed to constitute a phagocyte attraction signal [15]. However, most of the studies concerning the cellular effect of lysoPtdCho were performed in primary cell cultures using saturated lysoPtdCho or oleoylated lysoPtdCho [9, 16], and moreover, these studies were carried out in serum-free media, since serum components interfered with the action of lysoPtdCho. Therefore, it needs to be clarified further as to whether lysoPtdCho may exert any significant biological effect on cells in the medium containing serum. In the present study, we attempted to examine the effect of lysoPtdCho, saturated and unsaturated, on RAW 264.7 cells in either serum-free medium or serum-containing medium. Here, we report that 1-linoleoyl (C18:2) lysoPtdCho shows a selective cytotoxic effect on RAW 264.7 cells by causing ROS formation, accompanied by activation of extracellular signal-regulated kinase (ERK) and induction of inflammatory cytokines, in the medium containing serum.
Materials and Methods
Materials
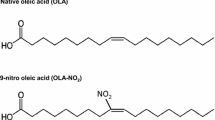
1-Palmitoyl (C16:0) lysoPtdCho, 1-stearoyl (C18:0) lysoPtdCho, 1-myristoyl (C14:0) lysoPtdCho, 1-oleoyl (C18:1) lysoPtdCho, dilinoleoyl PtdCho and diarachidonoyl PtdCho were from Avanti Polar Lipids (Alabaster, AL, USA). Magnolol (purity >95%) was kindly provided by Dr K. Bae, College of Pharmacy, Chungnam National University. 2′,7′-Dichlorofluorescein diacetate (DCFH2-DA) was from Molecular Probe (Eugene, OR, USA), Dulbecco’s modified Eagle’s medium (DMEM), fetal bovine serum (FBS), penicillin, streptomycin and trypsin-EDTA were purchased from Gibco/BRL (Gaithersburg, MD, USA). Suramin, 3-(4,5-Dimethylthiazole-2-yl)-2,5-diphenyltetrazolium bromide (MTT), phosphor-specific antibodies against ERK were obtained from BD Biosciences (San Jose, CA, USA), and all other reagents were from Sigma-Aldrich (St Louis, MO, USA) unless specifically described. 1-Linoleoyl (C18:2) lysoPtdCho and 1-arachidonoyl (C20:4) lysoPtdCho were synthesized by PLA2-catalyzed hydrolysis of corresponding phosphatidylcholine species as described previously [17].
Cell Culture
RAW 264.7 cells were cultured in DMEM-supplemented with, penicillin (100 U/mL) and streptomycin (100 μg/mL), 10% (v/v) heat-inactivated FBS at 37 °C in a humidified atmosphere of 5% CO2 as previously described [18], and used between passages 6–13 at ~80% confluence unless otherwise stated. Cells were plated at a density of 5 × 104/well in 96-well plate, and incubated overnight to allow for adherence.
Determination of Cytotoxicity
Cell respiration, an indicator of cell viability, was determined by measuring the mitochondrial-dependent reduction of MTT to formazan [18]. Briefly, the cells (5 × 104/well), plated in the media, were incubated for indicated times at 37 °C in a 5% CO2 incubator. MTT solution was added to cells to a final concentration of 500 μg/mL, and the incubation was continued for 4 h at 37 °C. Then, the medium was aspirated, and the formazan products were solubilized with dimethyl sulfoxide. The cell viability was determined by measuring the difference of absorbance at wavelength 570 nm vs. 690 nm. To see the cytotoxicity during 10 min incubation, the cells were incubated with lysoPtdCho for 10 min in a serum-free medium. Separately, for delayed cytotoxicity of lysoPtdCho, the cells were incubated with lysoPtdCho for 24 h in DMEM containing 10% FBS.
Measurement of Intracellular ROS
Oxidative stress of the cells was determined by using the fluorescent probe DCFH2-DA [19]; DCFH2-DA, cell-permeable, is converted into the fluorescent 2,7-dichlorofluorescein by oxidative substances in cells. Briefly, cells (5 × 104/well) were pretreated with antioxidants of various concentrations for 2 h at 37 °C. Subsequently, lysoPtdCho was added to the cells, and the incubation was further extended according to the specified time. At the end of the incubation, the cells were treated with fluorescent probe DCFH2-DA (10 μM) for 30 min. The degree of fluorescence, corresponding to intracellular ROS, was determined using a spectrofluorometer (Wallac 1420, Perkin-Elmer, Turku, Finland) at 485 nm excitation and 530 nm emission wavelengths.
Prevention Against Cytotoxicity or ROS Formation
Cells (5 × 104/well) were pretreated with antioxidant or other drugs, and then lysoPtdCho was added to to the cells. The incubation was continued for 10 min in a serum-free medium or for 24 h in the medium containing 10% FBS. Determination of cytotoxicity or ROS formation was performed as described above.
Western Blot Analysis
RAW 264.7 cells were stimulated with or without 10 μM lysoPtdCho or 0.1 μg/mL lipopolysaccharide for 10 min. Cytosolic extracts were prepared in lysis buffer consisting of 0.2% NP-40, 10 mM HEPES, 15 mM KCl, 2 mM MgCl2, 1 mM dithiothreitol, 0.1 mM EDTA and 0.1 mM PMSF. Equal amounts of protein (20 μg/well) were separated by 10% SDS-polyacrylamide gel electrophoresis, and transferred to a nitrocellulose membrane (GE Healthcare UK Ltd, Buckinghamshire, UK). Each membrane was blocked overnight at 4 °C with a blocking solution (10 mM Tris–HCl, pH 7.4; 125 mM NaCl; 0.1% Tween 20; 5% skim milk) and then incubated with antibodies to ERK and phospho-ERK (Cell Signaling, Danvers, MA, USA) at room temperature for 3 h. The blots were washed three times with washing buffer (20 mM Tris, 160 mM NaCl and 0.1% Tween 20), followed by a 1-h incubation with appropriate horseradish peroxidase-conjugated secondary antibody. The peroxidase activity was detected using the Immobilon Western HRP detection reagent (Millipore, Billerica, MA, USA). This immunoblots analysis was performed three times independently.
Quantitative RT-PCR Analysis
RAW 264.7 cells were treated with or without 10 μM lysoPtdCho for 12 h. The cells were harvested and total RNA was extracted using an Easy-Blue™ kit (INtRON Biotechnology, Korea) according to the manufacturer’s instructions. A sample (1 μg) of total RNA was used for the synthesis of the first strand cDNA using the Omniscript (Qiagen, Valencia, CA, USA) according to the manufacture’s instructions. PCR amplifications were quantified using the SYBRGreen™ PCR Master Mix (Applied Biosystems, Foster City, CA, USA) against the expression of genes involved in proinflammatory mediators such as IL-1β, CCL2 and CCL5. The primers were provided in Table 1. After obtaining real-time fluorescence measurements, cycle threshold values were determined. Standard curves in the linear range (i.e., the exponential amplification phase) were used to calculate the quantity of each mRNA. The final data are expressed as the ratio of indicated mRNA to GAPDH mRNA.
Statistical Analysis
All values are expressed as means ± SD. The statistical analysis was done on an SPSS (Chicago, IL, USA) program. One-way analysis of variance and Duncan’s multiple range tests were used to examine the difference groups. A value of P < 0.05 was accepted as statistically significant, unlesss otherwise stated.
Results
Lysophosphatidylcholine has been believed to play an important role in atherosclerosis and inflammatory diseases by altering various functions in a number of cell-types [20]. Previously, it was reported that lysoPtdCho expressed cytotoxicity primarily by causing an increase of intracellular calcium ions and the formation of ROS through activation of NOX in primary suspension cells in serum-free media [21]. Separately, a remarkable formation of ROS by unsaturated lysoPtdCho was observed in human neutrophils in the serum-free media [16]; the most dramatic effect was expressed by 1-oleoyl (C18:1) lysoPtdCho, followed by 1-linoleoyl (C18:2) lysoPtdCho. However, little is known about the cytotoxic effects of polyunsaturated lysoPtdCho on adherent cells in the presence of serum. First, in this study, we examined the cytotoxic effect of lysoPtdCho on RAW 264.7 cells, representative adherent cells, since lysoPtdCho was believed to play an important role in atherosclerosis by altering various functions in monocytes and macrophages [22]. For this purpose, RAW 264.7 cells were exposed to lysoPtdCho with various acyl chains, saturated or unsaturated, in the serum-free medium, and the viability was determined using MTT assays [18].
Effects of lysoPtdCho on Macrophage Viability During 10 min Incubation in a Serum-Free Medium
First, when RAW 264.7 cells were incubated with 1-palmitoyl (C16:0) lysoPtdCho for 10 min in serum-free media, it was observed that 1-palmitoyl (C16:0) lysoPtdCho decreased the viability in a concentration-dependent fashion (Fig. 1); the remaining viability was reduced to 21% of the control level after 10 min incubation with 1-palmitoyl (C16:0) lysoPtdCho (20 μM). A similar cytotoxic effect was also exhibited by the other lysoPtdCho species such as 1-stearoyl (C18:0) lysoPtdCho (remaining viability 24.9%), 1-myristoyl (C14:0) lysoPtdCho (42.9%), 1-oleoyl (C18:1) lysoPtdCho (33.5%), 1-linoleoyl (C18:2) lysoPtdCho (37.3%) or 1-arachidonoyl (C20:4) lysoPtdCho (39.9%) after a 10-min incubation. In comparison (Table 2), the greatest cytotoxicity was expressed by 1-palmitoyl lysoPtdCho (IC50, 9.0 μM), followed by 1-stearoyl (C18:0) lysoPtdCho (IC50, 9.9 μM), 1-oleoyl (C18:1) lysoPtdCho (IC50, 13.0 μM), 1-linoleoyl (C18:2) lysoPtdCho (IC50, 11.6 μM), 1-arachidonoyl (C20:4) lysoPtdCho (IC50, 13.7 μM) and 1-myristoyl (C14:0) lysoPtdCho (IC50, 17.5 μM), indicating that the cytotoxic effect of lysoPtdCho may differ according to the type of acyl chain of the lysoPtdCho. The greater cytotoxicity of saturated lysoPtdCho such as 1-palmitoyl (C16:0) or 1-stearoyl (C18:0) lysoPtdCho may imply that lysoPtdCho acts as a detergent on the plasma membrane and thereby disturbs membrane stability. However, such a possibility is not supported by the additional finding that unsaturated lysoPtdCho, possessing relatively higher critical micelle concentration (CMC) values [23], also expresses a similar degree of cytotoxicity at the same concentration range. However, in media containing 10% FBS, no remarkable cytotoxicity (<5%) was exhibited by any of lysoPtdCho, suggesting that a component(s) of FBS prevented the cytotoxic action of lysoPtdCho.
Cytotoxicity of lysoPtdCho in RAW 264.7 cells during 10 min incubation in serum-free media. RAW 264.7 cells were incubated with various concentrations (0–40 μM) of lysoPtdCho for 10 min in serum-free media. Cell viability was determined by MTT assay, and the viability was expressed as a percentage of viable cells among total cells. Data are shown as mean ± SD of three parallel experiments. Filled squares indicate 1-myristoyl lysoPtdCho, open inverted triangles indicate 1-palmitoyl lysoPtdCho, open squares indicate 1-stearoyl lysoPtdCho, filled circles indicate 1-oleoyl lysoPtdCho, open circles indicate 1-linoleoyl lysoPtdCho, filled inverted triangles indicate 1-arachidonoyl lysoPtdCho
Effects of lysoPtdCho on ROS Production in RAW 264.7 Cells During 10-min Incubation in a Serum-Free Medium
Reactive oxygen species have been suggested to be involved in the cytotoxic effect of lysoPtdCho [24], which has been reported to induce NAD(P)H oxidase, and increase the formation of superoxide anion radicals in nonphagocytic cells [25], particularly in vascular endothelial cells [20]. To determine whether the death of RAW 264.7 cells by lysoPtdCho is related to ROS production, we measured the ROS generation in RAW 264.7 cells using a fluorescent probe (DCFH2-DA). As shown in Fig. 2, when each lysoPtdCho was incubated with RAW 264.7 cells in the serum-free medium for 10 min, 1-linoleoyl (C18:2) lysoPtdCho induced a considerable ROS production in RAW 264.7 cells in a concentration-dependent manner up to 20 μM, confirming the previous finding [16] that 1-linoleoyl (C18:2) lysoPtdCho-induced ROS formation in human neutrophils in serum-free media. In addition, a similar result was also observed with 1-arachidonoyl (C20:4) lysoPtdCho, although it caused a lower extent of ROS formation, compared to 1-linoleoyl (C18:2) lysoPtdCho. Meanwhile, other lysoPtdCho species including 1-oleoyl (C18:1) lysoPtdCho were not effective in inducing ROS formation. Thus, a considerable ROS generation was expressed only by lysoPtdCho with a 1-linoleoyl (C18:2) or a 1-arachidonoyl (C20:4) group, suggesting that ROS production might be related to the cytotoxicity of polyunsaturated lysoPtdCho in RAW 264.7 cells in the presence of serum. To confirm the above notion, the protective effect of antioxidant agents against 1-linoleoyl (C18:2) lysoPtdCho-induced ROS generation was evaluated. Figure 3 indicates that ROS generation by 1-linoleoyl (C18:2) lysoPtdCho was reduced by magnolol partially at 30 μM and fully at 100 μM. Nonetheless, the viability was not restored to the control level in the presence of magnolol even up to 100 μM. These results suggest that the formation of ROS may not be responsible for the cytotoxicity of unsaturated lysoPtdCho during a short incubation in serum-free medium. Thus, ROS appear to play a negligible role in lysoPtdCho-induced cytotoxicity during short time incubation in serum-free media. In the meantime, the inclusion of serum completely prevented the cytotoxicity of each lysoPtdCho as well as ROS formation by lysoPtdCho. These led us to examine whether the extended incubation of RAW 264.7 cells with lysoPtdCho may cause a remarkable cytotoxicity even in the presence of serum.
Effect of lysoPtdCho on the formation of intracellular ROS. RAW 264.7 cells were incubated with various concentrations of lysoPtdCho (1, 3, 10 or 20 μM) for 10 min in serum-free media. Accumulation of intracellular ROS was monitored with DCFH2-DA as described in the section “Materials and Methods”. Data are shown as means ± SD of three parallel experiments. Filled squares indicate 1-myristoyl lysoPtdCho, open inverted triangles indicate 1-palmitoyl lysoPtdCho, open squares indicate 1-stearoyl lysoPtdCho, filled circles indicate 1-oleoyl lysoPtdCho, open circles indicate 1-linoleoyl lysoPtdCho, filled inverted triangles indicate 1-arachidonoyl lysoPtdCho
Effect of antioxidants on lysoPtdCho-induced cytotoxicity and ROS production. RAW 264.7 cells were pretreated with magnolol (1–100 μM), and then incubated with 1-linoleoyl lysoPtdCho (20 μM) for 10 min in serum-free media. Data are shown as means ± SD of three parallel experiments; *P < 0.05 vs. control, **P < 0.01 vs. control. C without lysoPtdCho and magnolol
Effects of lysoPtdCho on Macrophage Viability During 24 h Incubation in a Medium Containing 10% FBS
In the subsequent experiment to see the delayed effect of lysoPtdCho, RAW 264.7 cells were incubated with each lysoPtdCho of various concentrations in media containing 10% FBS for 24 h, after which the viability of the remaining cells was analyzed by MTT assays [18]. First, when RAW 264.7 cells were incubated with lysoPtdCho of various concentrations for 24 h, a remarkable cytotoxic effect was demonstrated by 1-linoleoyl (C18:2) lysoPtdCho (Fig. 4); the viability decreased to 68.7% of control level after 24 h incubation with 1-linoleoyl (C18:2) lysoPtdCho (20 μM), and the increase of 1-linoleoyl (C18:2) lysoPtdCho concentration beyond 20 μM failed to further increase the cytotoxicity. Actually, the delayed cytotoxicity of 1-linoleoyl (C18:2) lysoPtdCho started to appear after 9 h incubation. In addition, 1-arachidonoyl (C20:4) lysoPtdCho also seemed to show a similar cytotoxic effect, although the maximal decrease of viability was limited to 9.8%. Meanwhile, the other lysoPtdCho species such as 1-oleoyl (C18:1) lysoPtdCho, 1-myristoyl (C14:0) lysoPtdCho, 1-palmitoyl (C16:0) lysoPtdCho or 1-stearoyl (C18:0) lysoPtdCho exerted no significant cytotoxic effect (<5%). Thus, it seems that the delayed cytotoxicity seems to be expressed selectively by 1-linoleoyl (C18:2) lysoPtdCho.
Cytotoxicity of lysoPtdCho in RAW 264.7 cells during 24 h incubation in serum-containing media. Cells were incubated with each lysoPtdCho (0–40 μM) for 24 h in media containing 10% FBS. Cell viability was determined by MTT assay, and the viability was expressed as a percentage of viable cells among total cells. Data are shown as mean ± SD of three parallel experiments. Filled squares indicate 1-myristoyl lysoPtdCho, open inverted triangles indicate 1-palmitoyl lysoPtdCho, open squares indicate 1-stearoyl lysoPtdCho, filled circles indicate 1-oleoyl lysoPtdCho, open circles indicate 1-linoleoyl lysoPtdCho, dark filled inverted triangles indicate 1-arachidonoyl lysoPtdCho
Effect of lysoPtdCho on ROS Production During 24 h Incubation in a Medium Containing 10% FBS
To determine whether the delayed cell death of RAW 264.7 cells by 1-linoleoyl (C18:2) lysoPtdCho was related to ROS production, we measured ROS generation in RAW 264.7 cells exposed to 1-linoleoyl (C18:2) lysoPtdCho in a medium containing 10% FBS for 24 h. As shown in Fig. 5, 1-linoleoyl (C18:2) lysoPtdCho induced evidently a considerable ROS production in RAW 264.7 cells in a concentration-dependent manner (1–100 μM), reaching its peak at 40 μM. The effective concentrations (10–40 μM) of 1-linoleoyl (C18:2) lysoPtdCho for ROS formation was close to those for its cytotoxicity in RAW 264.7 cells. Meanwhile, the other types of lysoPtdCho including 1-arachidonoyl (C20:4) lysoPtdCho failed to express a significant formation of ROS. These data suggest that the structural requirement of the acyl group for the cytotoxicity of lysoPtdCho in a serum-free medium is apparently different from that in a medium containing FBS.
Effect of lysoPtdCho on formation of intracellular ROS. RAW 264.7 cells were incubated with various concentrations of lysoPtdCho (1–100 μM) for 24 h in media containing 10% FBS. Accumulation of intracellular ROS was monitored with DCFH2-DA. Data are shown as means ± SD of three parallel experiments. a 1-Myristoyl lysoPtdCho, b 1-palmitoyl lysoPtdCho, c 1-stearoyl lysoPtdCho, d 1-oleoyl lysoPtdCho, e 1-linoleoyl lysoPtdCho, f 1-arachidonoyl lysoPtdCho
Protection by Antioxidants Against Cytotoxicity of 1-Linoleoyl (C18:2) lysoPtdCho and ROS Formation
To further examine the mechanism by which 1-linoleoyl (C18:2) lysoPtdCho decreased the viability of RAW 264.7 cells during a 24-h incubation in the presence of FBS, the protective effect of antioxidant agents on the delayed cytotoxicity of 1-linoleoyl (C18:2) lysoPtdCho (20 μM) was examined. As shown in Fig. 6a, magnolol (30 μM) prevented the delayed cytotoxic action of 1-linoleoyl (C18:2) lysoPtdCho in a concentration-dependent manner; the viability, which deceased to 68.7% in the presence of 1-linoleoyl (C18:2) lysoPtdCho, was restored to 93.5% in the presence of magnolol with an EC50 of 9.05 ± 1.79 μM. Additionally, trolox, another antioxidant, augmented the viability to 82.8% with an EC50 of 143 ± 21.1 μM (Fig. 6b). In a separate experiment, the effect of antioxidant agents on the ROS formation in RAW 264.7 cells, exposed to 1-linoleoyl (C18:2) lysoPtdCho (20 μM) for 24 h in a medium containing FBS, was examined. As shown in Fig. 7a, the inclusion of magnolol reduced the 1-linoleoyl (C18:2) lysoPtdCho-induced ROS formation in RAW 264.7 cells in a dose-dependent manner with an EC50 of 9.16 ± 1.99 μM. In addition (Fig. 7b), trolox also decreased the 1-linoleoyl (C18:2) lysoPtdCho-induced ROS formation in RAW 264.7 cells, although less effectively than magnolol. Thus, it is suggested that the delayed cytotoxicity of 1-linoleoyl (C18:2) lysoPtdCho in RAW 264.7 cells may be likely related to the increased ROS generation. Separately, suramin, a lysophosphatidic acid receptor antagonist, was tested for the prevention of 1-linoleoyl (C18:2) lysoPtdCho-induced cytotoxicity or ROS formation, since lysoPtdCho could be converted to lysophosphatidic acid during 24 h incubation. However, the lysophosphatidic acid receptor antagonist did not diminish the cytotoxicity of 1-linoleoyl (C18:2) lysoPtdCho or ROS formation in RAW 264.7 cells (data not shown), excluding the possibility that the cytotoxicity of 1-linoleoyl (C18:2) lysoPtdCho may be related to the action of lysophosphatidic acid, a degradation product of lysoPtdCho. Taken together, all the results suggest that oxidative stress may be implicated in the cytotoxicity of 1-linoleoyl (C18:2) lysoPtdCho in RAW 264.7 cells challenged with 1-linoleoyl (C18:2) lysoPtdCho.
Effect of antioxidants on lysoPtdCho-induced cell death. RAW 264.7 cells were pretreated with increasing magnolol concentrations (a) or increasing trolox concentrations (b), and then incubated with 1-linoleoyl lysoPtdCho (20 μM) for 24 h in media containing 10% FBS. Cell viability was determined by MTT assay, and the viability was expressed as a percentage of viable cells among total cells. Data are shown as means ± SD of three parallel experiments; *P < 0.05 vs. control, **P < 0.01 vs. control. C without lysoPtdCho and magnolol
Effect of antioxidants on lysoPtdCho-induced production of intracellular ROS. RAW 264.7cells were pretreated with increasing concentrations of magnolol (a) or increasing concentrations of trolox (b), and then incubated with 20 μM 1-linoleoyl lysoPtdCho for 24 h in media containing 10% FBS. Data are shown as means ± SD of three parallel experiments; *P < 0.05 vs. control, **P < 0.01 vs. control
Induction of Phosphorylation of ERK by 1-Linoleoyl (C18:2) lysoPtdCho
Since previous studies showed that the lysoPtdCho-induced activation of MAPKs pathways, dependent on ROS production, was observed in monocytes and endothelial cells [26], it was supposed that the production of ROS by 1-linoleoyl (C18:2) lysoPtdCho might be related to activation of MAPKs in macrophages. In this respect, RAW 264.7 cells were exposed to each lysoPtdCho, and the phosphorylation of ERK1/2 was evaluated. As demonstrated in Fig. 8, Western blot analysis clearly showed that 1-linoleoyl (C18:2) lysoPtdCho caused a significant increase in phosphorylation of ERK1/2 in a dose-dependent manner. However, the other lysoPtdCho such as 1-myristoyl (C14:0) lysoPtdCho, 1-palmitoyl (C16:0) lysoPtdCho and 1-oleoyl (C18:1) lysoPtdCho even at 10 μM were not effective. These findings indicate that ERK1/2 phosphorylation may be related to 1-linoleoyl lysoPtdCho-induced ROS formation in RAW 264.7 cells.
Effects of lysoPtdCho on phosphorylation of ERK 1/2 in RAW 264.7 cells. Cells were treated with various lysoPtdCho (10 μM) or LPS (100 ng/mL) for 10 min. Harvested cells were lysed, and the extracted proteins were separated on 10% SDS-polyacrylamide gels and transferred to nitrocellulose membrane. Phosphorylation of ERK 1/2 was detected by Western blotting as described in the section “Materials and Methods”. The membrane was stripped and reproved with ERK 1/2 antibody as an internal control (a). Separately, cells were treated with dose-dependent 1-linoleoyl lysoPtdCho or 100 ng/mL LPS, and were analyzed as described above (b). M 1-myristoyl lysoPtdCho, P 1-palmitoyl lysoPtdCho, O 1-oleoyl lysoPtdCho, L 1-linoleoyl lysoPtdCho
LysoPtdCho Induces Proinflammatory Cytokine and Chemokine Gene Expression in RAW 264.7 Cells
In the next study to assess the lysoPtdCho-induced signal transduction pathway of cytokines responsible for inflammatory reactions, we examined the expression of cytokines in response to 1-linoleoyl (C18:2) lysoPtdCho or 1-palmitoyl (C16:0) lysoPtdCho. For this purpose, lysoPtdCho was incubated with murine macrophages to produce cytokines, and 12 h later, RNA was extracted from RAW 264.7 cells, and analyzed by graphical representations of the fold changes in cytokines. Figure 9 indicated that the production of IL-1β and CCL2 was increased by about 20 times in the presence of 1-linoleoyl (C18:2) lysoPtdCho at 10 μM, and the gene expression of CCL5 was up-regulated by ≥10-folds (P < 0.05), compared to control. Thus, a more dramatic induction was observed for CCL2 acting mainly in inflammatory reactions. Meanwhile, there was no significant difference of cytokines gene expression after the exposure to 1-palmitoyl (C16:0) lysoPtdCho. These results indicate that the cytotoxicity as well as ROS formation by 1-linoleoyl (C18:2) lysoPtdCho may implicate the upregulation of transcription of proinflammatory mediator genes in the RAW 264.7 cells.
Effect of lysoPtdCho on the expression of cytokines by RAW 264.7 cells. Cells were treated with 1-linoleoyl lysoPtdCho for 12 h. Expression levels of Interleukin-1β (IL-1β), CCL2 or CCL5, which were determined by a quantitative real time-polymerase chain reaction (qRT-PCR), were normalized to GAPDH, and plotted relative to those without 1-linoleoyl lysoPtdCho (control). All assays were performed in triplicate, and data are expressed as mean values ± SD. *P < 0.05 vs. control, **P < 0.01 vs control. P 1-palmitoyl lysoPtdCho, L 1-linoleoyl lysoPtdCho
Discussion
Lysophosphatidylcholine is believed to play an important role in patho-physiological conditions by altering various functions in a number of cell-types [27]. Earlier, the membrane effects of lysoPtdCho had been studied extensively in erythrocytes; lysoPtdCho, at concentrations above its CMC, disturbed membrane proteins, and disrupted plasma membrane integrity, leading to hemolysis [28]. Separately, lysoPtdCho, accumulating in the atherosclerotic arterial wall [29], has been suggested as playing a role in the progress of atherosclerosis, via receptor-mediated or independent actions, by causing vascular endothelial growth factor induction in macrophages, impairment of NO release, and upregulation of cell adhesion molecules, and acting as a monocyte chemoattractant [30]. In addition, the cytotoxicity of lysoPtdCho has been studied in vascular cells; for example, lysoPtdCho has been reported to induce apoptotic death in rat aorta smooth muscle cells at low concentrations (25–50 μM), and induce necrosis at concentrations >100 μM [31]. In human endothelial cells, lysoPtdCho at concentrations (25–300 μM) has been shown to induce apoptosis, whereas primary necrosis has not been observed [22]. Our present data may provide an evidence for the cytotoxic effect of lysoPtdCho on RAW 264.7 cells. Thus, the effect of lysoPtdCho on cells may depend on the lysoPtdCho concentration or the cell type as well as incubation conditions. Concerning the cytotoxicity of lysoPtdCho, lysoPtdCho as a detergent can be directly incorporated into the lipid matrix of cellular membranes and increase fluidity [28]. Further, lysoPtdCho at concentrations above its CMC values might induce micellar disruption, thus damaging membrane integrity. The present finding about the structure activity relationship for the cytotoxicity of saturated lysoPtdCho in RAW 264.7 cells in serum-free medium seemed to reflect the micellar property of lysoPtdCho [32] as had been observed with the cytotoxicity of lysoPtdCho in neutrophils [16]; the CMC value of saturated lysoPtdCho was inversely proportional to the size of acyl chain. However, this idea was not supported by another finding that 1-linoleoyl (C18:2) lysoPtdCho expressed a cytotoxicity below their CMC values (>20 μM). Moreover, there was no significant difference of cytotoxicity between 1-oleoyl (C18:1) lysoPtdCho and 1-arachidonoyl (C20:4) lysoPtdCho, despite a great difference of their CMC values. Rather, it is supposed that the cytotoxic actions of lysoPtdCho may be explained by mechanisms different from detergent function [16]. One of them may involve the induction of oxidative stress, as had been previously observed in other types of cells [16, 31]. The formation of ROS through the activation of NOX had been observed with Jurkat T cells [33], fibroblast cell [32], human neutrophils [10] and endothelial cells [31] in the absence of serum, which prevented the cytotoxicity of lysoPtdCho [33]. However, in the present study, the cytotoxicity of lysoPtdCho during 10 min incubation in a serum-free medium was not addressed properly by ROS formation. Further, the cytotoxicity of lysoPtdCho was not prevented significantly by antioxidants. Meanwhile, the delayed cytotoxicity of 1-linoleoyl (C18:2) lysoPtdCho in medium containing 10% FBS was supposed to be related to ROS formation, since the delayed cytotoxicity was accompanied by ROS formation. A further support is from the finding that antioxidants such as magnolol and trolox diminished cytotoxicity as well as ROS formation in RAW 264.7 cells. It is worth noting that the delayed cytotoxicity in the presence of serum was expressed remarkably by 1-linoleoyl (C18:2) lysoPtdCho and slightly by 1-arachidonoyl (C20:4) lysoPtdCho, but not by saturated lysoPtdCho. Moreover, 1-oleoyl (C18:1) lysoPtdCho also failed to show a significant formation of ROS in RAW 264.7 cells in the presence of serum, despite a remarkable ROS formation by 1-oleoyl (C18:1) lysoPtdCho in human neutrophils in a serum-free medium [16]. Thus, it seems that the delayed cytotoxicity of lysoPtdCho may be peculiar to 1-linoleoyl (C18:2) lysoPtdCho in RAW 264.7 cells. Additionally, the delayed cytotoxicity of 1-linoleoyl (C18:2) lysoPtdCho might be cell-specific, since 1-linoleoyl (C18:2) lysoPtdCho did not show a delayed cytotoxic effect on RBL-2H3 cells. Taken together, the delayed cytotoxicity of 1-linoleoyl (C18:2) lysoPtdCho seems to depend on the types of cells or lysoPtdCho as well as the incubation conditions.
Although a previous study indicated that albumin and lipoprotein fractions of plasma contained higher amounts of saturated lysoPtdCho than unsaturated ones [31], this could not provide a relevant explanation of the selective cytotoxicity of 1-linoleoyl (C18:2) lysoPtdCho. Separately, alpha-1-acid glycoprotein was observed to show a strong binding affinity toward unsaturated lysoPtdCho [6]. However, such an action of alpha-1-acid glycoprotein may lead to the reduction in the cytotoxicity of 1-linoleoyl (C18:2) lysoPtdCho, although the possible delivery of lipids by alpha-1-acid glycoprotein to cell membrane may not be neglected. Rather, the delayed cytotoxicity of 1-linoleoyl (C18:2) lysoPtdCho is supposed to depend on free lysoPtdCho equilibrating with blood proteins- or lipoproteins-bound ones. Since the effective concentrations (10–20 μM) of 1-linoleoyl (C18:2) lysoPtdCho for delayed cytotoxicity was much below the reported CMC (~50 μM) of lysoPtdCho in aqueous medium [34], it is more likely that the delayed cytotoxicity of 1-linoleoyl (C18:2) lysoPtdCho may be due to the specific interaction, rather than non-specific lipid interaction, between 1-linoleoyl (C18:2) lysoPtdCho and RAW 264.7 cells. The plasma concentration of lysoPtdCho ranges from 100 to 190 μM [35]; the most abundant lysoPtdCho species in fresh plasma samples was 1-palmitoyl (C16:0) lysoPtdCho, comprising ~40% of total lysoPtdCho, followed by 1-linoleoyl (C18:2) lysoPtdCho, corresponding to ~20% of total lysoPtdCho. Based on this, the plasma concentration of lysoPtdCho was estimated to be ~40 μM for 1-palmitoyl (C16:0) lysoPtdCho and 20 μM for 1-linoleoyl (C18:2) lysoPtdCho. Since the concentrations (10–20 μM) of lysoPtdCho for delayed cytotoxicity of 1-linoleoyl (C18:2) lysoPtdCho were close to the physiological level, it is supposed that 1-linoleoyl (C18:2) lysoPtdCho may be one of plasma lysoPtdCho species implicated in the patho-physiological states. It is possible that lysophosphatidic acid, generated from the incubation of lysoPtdCho with RAW 264.7 cells, may be possibly responsible for the cytotoxicity. However, this is not supported by the observation that 1-linoleoyl (C18:2) lysophosphatidic acid was less cytotoxic than 1-palmitoyl (C16:0) lysophosphatidic acid in RAW 264.7 cells during 24 h incubation in medium containing FBS (data not shown). Separately, it is conceivable that the 1-(13-hydroperoxy) octadecadienoyl (C18:2) lysoPtdCho, generated from 24 h exposure of 1-linoleoyl (C18:2) lysoPtdCho to RAW 264.7 cells, may express the cytotoxicity. However, 1-(13-hydroperoxy) octadecadienoyl (C18:2) lysoPtdCho up to 10 μM failed to show any cytotoxic effect on RAW 264.7 cells (data not shown). All these observations suggest that the cytotoxic effect of lysoPtdCho on RAW 264.7 cells differed according to the incubation conditions as well as types of cells or lysoPtdCho. Overall, saturated lysoPtdCho species were more cytotoxic than unsaturated lysoPtdCho species in the serum-free medium, but the reverse seemed to be true for the 24-h incubation in the medium containing FBS. Especially, 1-linoleoyl (C18:2) lysoPtdCho at physiological concentrations demonstrated a remarkable delayed cytotoxicity. Another important finding addressed by the present study is the involvement of the MAPK pathways in the selective cytotoxicity of 1-linoleoyl (C18:2) lysoPtdCho in RAW 264.7 cells. This may be consistent with previous findings that lysoPtdCho causes the activation of MAPK during apoptotic cell death in certain types of cells [36], and induces the activation of MAPK such as ERK 1/2 and JNK in endothelial cells [37]. However, most of these studies were done with 1-palmitoyl (C16:0) lysoPtdCho or 1-oleoyl (C18:1) lysoPtdCho, which failed to activate MAPK significantly in our present study. Although this discrepancy was not further examined in the present study, one possibility is that the selective interaction between 1-linoleoyl (C18:2) lysoPtdCho and RAW 264.7 cells may be responsible for the cytotoxicity of 1-linoleoyl (C18:2) lysoPtdCho as well as activation of MAPK. In support of this, there is a good correlation between the level of 1-linoleoyl (C18:2) lysoPtdCho-induced ERK activation and the cytotoxicity of 1-linoleoyl (C18:2) lysoPtdCho, accompanied by ROS formation. This idea may be somewhat relevant to a recent report that ERK can contribute to exerting apoptotic cell death during the cellular response to oxidative stress [38], although the role of the MAPK pathway in apoptosis is still controversial. Alternatively, it is conceivable that 1-linoleoyl (C18:2) lysoPtdCho-induced MAPK activation may be responsible for NOX-mediated ROS production according to a NOX–ROS–ERK-dependent pathway [27], since NOX-generated ROS may aid the phosphorylation of ERK and thereby contribute to upregulation in a downstream gene that is mediated by the ERK-dependent pathway. Additionally, we demonstrated that 1-linoleoyl (C18:2) lysoPtdCho markedly induces the expression of cytokine IL-1β, and chemokines CCL2 (MCP-1) and CCL5 (RANTES) in RAW 264.7 cells while 1-palmitoyl (C16:0) lysoPtdCho failed to induce the expression. The mechanism for the increase in the production of cytokine by lysoPtdCho may be related to the activation of MAPK, as previously observed with inflammatory cells [36, 39]. In this regard, it is conceivable that the induction of CCL2 by 1-linoleoyl (C18:2) lysoPtdCho may contribute to the pro-inflammatory response in atherosclerosis. Taken together, present observations suggest that 1-linoleoyl (C18:2) lysoPtdCho may exert proinflammatory actions by selectively inducing ROS formation, activation of MAPK and gene expression of cytokines in some specific cells. Further study employing in vivo methods may divulge the role of 1-linoleoyl (C18:2) lysoPtdCho in pro-inflammatory conditions.
Abbreviations
- lysoPtdCho:
-
Lysophosphatidylcholine
- ROS:
-
Reactive oxygen species
- FBS:
-
Fetal bovine serum
- MTT:
-
3-(4,5-Dimethylthiazole-2-yl)-2,5-diphenyltetrazolium bromide
- ERK:
-
Extracellular signal-regulated kinase
- CCL:
-
Chemotactic cytokines ligand
References
Adibhatla Rao M, Hatcher JF (2006) Phospholipase A2, reactive oxygen species, and lipid peroxidation in cerebral ischemia. Free Radic Biol Med 40:376–387
Zalewski A, Macphee CH (2005) Role of lipoprotein-associated phospholipase A2 in atherosclerosis: biology, epidemiology, and possible therapeutic target. Arterioscler Thromb Vasc Biol 25:923–931
Daleau P (1999) Lysophosphatidylcholine, a metabolite which accumulates early in myocardium during ischemia, reduces gap junctional coupling in cardiac cells. J Mol Cell Cardiol 31:1391–1401
Silliman CC, Clay KL, Thurman GW, Johnson CA, Ambruso DR (1994) Partial characterization of lipids that develop during the routine storage of blood and prime the neutrophil NADPH oxidase. J Lab Clin Med 124:684–694
Thumser AE, Voysey JE, Wilton DC (1994) The binding of lysophospholipids to rat liver fatty acid-binding protein and albumin. Biochem J 301:801–806
Ojala PJ, Hermansson M, Tolvanen M, Polvenen K, Hirvonen T, Impola U, Jauhiainen M, Somerharju P, Parkkinen J (2006) Identification of alpha-1 acid glycoprotein as a lysophospholipid binding protein: a complementary role to albumin in the scavenging of lysophosphatidylcholine. Biochemistry 45:14021–14031
Kugiyama K, Sakamoto T, Misumi I, Sugiyama S, Ohgushi M, Ogawa H, Horiguchi M, Yasue H (1993) Transferable lipids in oxidized low-density lipoprotein stimulate plasminogen activator inhibitor-1 and inhibit tissue-type plasminogen activator release from endothelial cells. Circ Res 73:335–343
Huang F, Subbaiah PV, Holian O, Zhang J, Johnson A, Gertzberg N, Lum H (2005) Lysophosphatidylcholine increases endothelial permeability: role of PKC and RhoA cross talk. Am J Physiol Lung Cell Mol Physiol 289:L176–L185
Silliman CC, Elzi DJ, Ambruso DR, Musters RJ, Hamiel C, Harbeck RJ, Bjornsen AJ, Wyman TH, Kelher M, England KM, McLaughlin-Malaxecheberria N, Barnett CC, Aiboshi J, Bannerjee A (2003) Lysophosphatidylcholines prime the NADPH oxidase and stimulate multiple neutrophil functions through changes in cytosolic calcium. J Leukoc Biol 73:511–524
Nishioka H, Horiuchi H, Arai H, Kita T (1998) Lysophosphatidylcholine generates superoxide anions through activation of phosphatidylinositol 3-kinase in human neutrophils. FEBS Lett 441:63–66
Guyton KZ, Liu Y, Gorospe M, Xu Q, Holbrook NJ (1996) Activation of mitogen-activated protein kinase by H2O2. Role in cell survival following oxidant injury. J Biol Chem 271:4138–4142
Yamakawa T, Eguchi S, Yamakawa Y, Motley ED, Numaguchi K, Utsunomiya H, Inagami T (1998) Lysophosphatidylcholine stimulates MAP kinase activity in rat vascular smooth muscle cells. Hypertension 31:258–263
Liu-Wu Y, Hurt-Camejo E, Wiklund O (1998) Lysophosphatidylcholine induces the production of IL-1beta by human monocytes. Atherosclerosis 137:351–357
Quinn MT, Parthasarathy S, Steinberg D (1988) Lysophosphatidylcholine: a chemotactic factor for human monocytes and its potential role in atherogenesis. Proc Natl Acad Sci USA 85:2805–2809
Lauber K, Bohn E, Krober SM, Xiao YJ, Blumenthal SG, Lindemann RK, Marini P, Wiedig C, Zobywalski A, Baksh S, Xu Y, Autenrieth IB, Schulze-Osthoff K, Belka C, Stuhler G, Wesselborg S (2003) Apoptotic cells induce migration of phagocytes via caspase-3-mediated release of a lipid attraction signal. Cell 113:717–730
Ojala PJ, Hirvonen TE, Hermansson M, Somerharju P, Parkkinen J (2007) Acyl chain-dependent effect of lysophosphatidylcholine on human neutrophils. J Leukoc Biol 82:1501–1509
Perez-Gilabert M, Veldink GA, Vliegenthart JF (1998) Oxidation of dilinoleoyl phosphatidylcholine by lipoxygenase 1 from soybeans. Arch Biochem Biophys 354:18–23
Mosmann T (1983) Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immunol Methods 65:55–63
Oyama Y, Hayashi A, Ueha T, Meakawa K (1994) Characterization of 2′,7′-dichlorofluorescin fluorescence in dissociated mammalian brain neurons: estimation on intracellular content of hydrogen peroxide. Brain Res 635:113–117
Matsumoto T, Kobayashi T, Kamata K (2007) Role of lysophosphatidylcholine (LPC) in atherosclerosis. Curr Med Chem 14:3209–3220
Takeshita S, Inoue N, Gao D, Rikitake Y, Kawashima S, Tawa R, Sakurai H, Yokoyama M (2000) Lysophosphatidylcholine enhances superoxide anions production via endothelial NADH/NADPH oxidase. J Atheroscler Thromb 7:238–246
Kume N, Cybulsky MI, Gimborne MJ (1992) Lysophosphatidylcholine, a component of atherogenic lipoproteins, induces mononuclear leukocyte adhesion molecules in cultured human and rabbit arterial endothelial cells. J Clin Invest 90:1138–1144
Croset M, Brossard N, Polette A, Lagarde M (2000) Characterization of plasma unsaturated lysophosphatidylcholine in human and rat. Biochem J 345:61–67
Waring P (2005) Redox active calcium ion channels and cell death. Arch Biochem Biophys 434:33–42
Watanabe N, Zmijewski JW, Takabe W, Umezu-Goto M, Le Goffe C, Sekine A, Landar A, Watanabe A, Aoki J, Arai H, Kodama T, Murphy MP, Kalyanaraman R, Darley-Usmar VM, Noguchi N (2006) Activation of mitogen-activated protein kinases by lysophosphatidylcholine-induced mitochondrial reactive oxygen species generation in endothelial cells. Am J Pathol 168:1737–1748
Komatsu D, Kato M, Nakayama J, Miyagawa S, Kamata T (2008) NADPH oxidase 1 plays a critical mediating role in oncogenic Ras-induced vascular endothelial growth factor expression. Oncogene 102:1–9
Bergmann SR, Ferguson TB Jr, Sobel BE (1981) Effects of amphiphiles on erythrocytes, coronary arteries, and perfused hearts. Am J Physiol 240:H229–H237
Bierbaum TJ, Bouma SR, Huestis WH (1979) A mechanism of erythrocyte lysis by lysophosphatidylcholine. Biochim Biophys Acta 555:102–110
Portman OW, Alexander M (1969) Lysophosphatidylcholine concentrations and metabolism in aortic intima plus inner media: effect of nutritionally induced atherosclerosis. J Lipid Res 10:158–165
Kugiyama M, Kern SA, Morrisett JD, Roberts R, Henry PD (1990) Impairment of endothelium-dependent arterial relaxation by lysolecithin in modified low-density lipoproteins. Nature 344:160–162
Zhou L, Shi M, Guo Z, Brisbon W, Hoover R, Yang H (2006) Different cytotoxic injuries induced by lysophosphatidylcholine and 7-ketocholesterol in mouse endothelial cells. Endothelium 13:213–226
Li Z, Mintzer E, Bittman R (2004) The critical micelle concentrations of lysophosphatidic acid and sphingosylphosphorylcholine. Chem Phys Lipids 130:197–201
Kim YL, Im YJ, Ha NC, Im DS (2007) Albumin inhibits cytotoxic activity of lysophosphatidylcholine by direct binding. Prostaglandins Other Lipid Mediat 83:130–138
Weltzien HU, Arnold B, Reuther R (1977) Quantitative studies on lysolecithin-mediated hemolysis. Use of ether-deoxy lysolecithin analogs with varying aliphatic chain-lengths. Biochim Biophys Acta 466:411–421
Okita M, Gaudette DC, Mills GB, Holub BJ (1997) Elevated levels and altered fatty acid composition of plasma lysophosphatidylcholine (lysoPC) in ovarian cancer patients. Int J Cancer 71:31–40
Murugesan G, Sandhya Rani MR, Gerber CE, Mukhopadhyay C, Ransohoff RM, Chisolm GM, Kottke-Marchant K (2003) Lysophosphatidylcholine regulates human microvascular endothelial cell expression of chemokines. J Mol Cell Cardiol 35:1375–1384
Ozaki H, Ishii K, Arai H, Kume N, Kita T (1999) Lysophosphatidylcholine activates mitogen-activated protein kinases by a tyrosine kinase-dependent pathway in bovine aortic endothelial cells. Atherosclerosis 143:261–266
Feuerstein GZ, Young PR (2000) Apoptosis in cardiac disease: stress and mitogen-activated signaling pathways. Cardiovasc Res 45:560–569
Jing Q, Xin S-M, Zhang W-B, Wang P, Qin Y-W, Pei G (2000) Lysophosphatidylcholine activates p38 and p42/44 mitogen-activated protein kinases in monocytic THP-1 cells, but only p38 activation is involved in its stimulated chemotaxis. Circ Res 87:52–59
Acknowledgment
This work was financially supported by a Korea Research Foundation Grant funded by the Korean Government (MOEHRD) (KRF-2007-531-C00067), Korea.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Park, C.H., Kim, M.R., Han, JM. et al. Lysophosphatidylcholine Exhibits Selective Cytotoxicity, Accompanied by ROS Formation, in RAW 264.7 Macrophages. Lipids 44, 425–435 (2009). https://doi.org/10.1007/s11745-009-3286-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11745-009-3286-6