Abstract
Quick Sequential Organ Failure Assessment (qSOFA) was proposed to replace SIRS as a new screening tool for the identification of septic patients at high mortality. However, researches from infected patients outside of ICU especially in Emergency Department (ED) drew contradictory conclusions on the prognostic value of qSOFA. This systematic review evaluated qSOFA as a prognostic marker of infected patients outside of ICU. The primary outcome was hospital mortality or 28- or 30-day mortality. Data were pooled based on sensitivity and specificity. Twenty-four trials with 121,237 participants were included. qSOFA had a poor sensitivity (0.58 [95% CI 0.47–0.67], 0.54 [95% CI 0.43–0.65]) and moderate specificity (0.69 [95% CI 0.48–0.84], 0.77 [95% CI 0.66–0.86]) for prediction of mortality in patients outside of ICU and ED patients only. Studies that used in-hospital mortality showed a higher sensitivity (0.61 [95% CI 0.50–0.71] vs 0.32 [95% CI 0.15–0.49]) and lower specificity (0.70 [95% CI 0.59–0.82] vs 0.92 [95% CI 0.85–0.99]) than studies that used 28 or 30-day mortality. Studies with overall mortality < 10% showed higher specificity (0.89 [95% CI 0.82–0.95] vs 0.62 [95% CI 0.48–0.76]) than studies with overall mortality ≥ 10%. There is no difference in the accuracy of diagnosis of sepsis between positive qSOFA scores and SIRS criteria. qSOFA was poor sensitivity and moderate specificity in predicting mortality of infected patients outside of ICU especially in ED. Combining qSOFA and SIRS may be helpful in predicting mortality.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Sepsis, a life-threatening organ dysfunction caused by dysregulated host response to infection, affects millions of people around the world and kills as many as one in four each year [1,2,3]. The Emergency Department (ED) is often the initial setting for the diagnosis and treatment of acute sepsis, and has up to nearly 850,000 emergency department visits annually in the United States [4]. Prompt identification and appropriate treatment of sepsis in ED are crucial to improve the patient outcome [5]; therefore, early and specific marker of sepsis would be useful in ED, especially when clinical signs and symptoms are still insufficient for diagnosis [6].
Systemic inflammatory response syndrome (SIRS) was used as a screen criteria to patients with infection for the diagnosis of sepsis since 1992 [7]; however, more and more evidence pointed out its high false-positive rates in the diagnosis of sepsis [8]. Recently, the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) Task Force proposed the new quick Sequential (Sepsis-related) Organ Failure Assessment (qSOFA) to replace SIRS as a new screening tool for the identification of patients with sepsis [9]. The qSOFA score ranges from 0 to 3 points (one point for each of the following: respiratory rate > 21 breaths/min; systolic arterial blood pressure ≤ 100 mmHg; or altered mental status), and an increase of at least two points indicates a high mortality of sepsis patients. Several studies were recently published to compare the predictive performance of qSOFA with SIRS score for mortality in these patients [10]. However, conflicting conclusions were generated, especially in the patients in ED, and a meta-analysis was needed to verify the predictive performance of qSOFA score.
Several meta-analyses on the prognostic or diagnostic accuracy of qSOFA or SIRS were indeed published [11,12,13,14]; however, meta-analysis specially focusing on the ED patients was not yet published. The aim of this study was to obtain summary estimates of prognostic and diagnostic performance of qSOFA in outside ICU especially ED patients with infection. We also analyzed different subgroups of ED patients to make more precise conclusions.
Methods
Search strategy
We performed a comprehensive database searching in Medline (via PubMed), the Cochrane Library, ISI Web of Knowledge, and Science Direct for studies that evaluated the qSOFA score and/or SIRS as a tool for predicting the prognosis of sepsis in ED patients from the inception of each database through Dec 2017. The following terms were used: Quick Sepsis-related Organ Failure Assessment (qSOFA), systematic inflammatory response syndrome (SIRS), sepsis, septic, infection, prognosis. We also searched the reference list of each primary study identified and articles dealing with literature review. We also conducted searches of abstracts from major conferences. The titles and abstracts of studies which were potentially relevant were scanned and the full articles were reviewed when the studies seemed to meet the criteria or when information was insufficient to exclude them.
Study selection criteria
Studies were included if they met the following criteria.
-
(1)
Adult patients outside of ICU with suspected or confirmed infection or sepsis.
-
(2)
RCT, propensity-matched cohort study (prospective or retrospective), or historically controlled study.
-
(3)
qSOFA as a predictive tool for predicting mortality or diagnosis of sepsis.
-
(4)
Sufficient data to calculate absolute numbers of true-positive, false-positive, false-negative, and true-negative results.
Data extraction and quality assessment
Following the initial screening, full articles were independently reviewed by two reviewers (Y-CL, Y-YL) with application of the same inclusion criteria. Disagreements were resolved by consensus. A predefined form was used to extract data from each study. We only included publications written in English. Two reviewers (Y-CL, Y-YL) independently assessed risk of bias of the included studies using the Quality Assessment of Diagnostic Accuracy Studies (QUADAS)-2 tool [15]. Disagreements were resolved by consensus. The qSOFA (positive if ≥ 2) and SIRS (positive if ≥ 2) score were defined following the proposed guideline [16, 17].
Statistical analysis
We presented the data as mean values for continuous variables and as frequencies for categorical variables. Results of individual studies were presented graphically by plotting sensitivity and specificity estimates on one-dimensional forest plots. Meta-analysis was performed by fitting bivariate models to our data. The estimates of pooled sensitivity, specificity, positive and negative likelihood ratios, with their 95% confidence intervals (CI) were calculated starting from parameter estimates obtained from bivariate models [18]. The effect of some predefined sources of heterogeneity (prospective vs retrospective study design; single-center vs multi-center; in-hospital mortality vs 28- or 30-day mortality; scores measured at ED arrival vs worst value; suspected vs confirmed infection; sepsis vs septic shock; overall mortality ≥ 10% vs overall mortality < 10%) was assessed by fitting bivariate meta-regression models with the inclusion of covariate terms. Bivariate meta-regression random effect model was also used in verifying the prognostic accuracy of qSOFA and SIRS criteria in diagnosis of sepsis. We performed all analysis using Review Manager (RevMan), and Stata15. A P value < 0.05 was considered statistically significant.
Results
Search results and description of studies
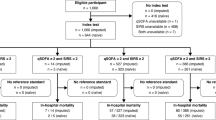
After screening titles and abstracts and completing full-text reviews, 24 studies met the inclusion criteria and were selected (Fig. 1). Table 1 described the characteristics of the 24 studies selected [9, 19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41]. Of the included studies, five studies (21%) were prospective studies, and the remaining were retrospective studies or hoc analysis. Seventeen studies (71%) included patients only in ED [19, 20, 25,26,27,28,29, 31, 33,34,35,36,37,38,39,40,41].
In the 17 studies from ED patients, 13 studies (76%) used in-hospital mortality as outcome measure, and four studies (24%) used 28- or 30-day mortality. Ten studies (59%) included patients with diagnosis of suspected or confirmed infection, and seven studies (41%) followed the diagnosis of sepsis or septic shock. Eleven studies (65%) measured the qSOFA at ED arrival, and six studies (35%) measured at the worst value during ED stay. The overall mortality rate in nine studies (53%) were over 10%, while eight studies (47%) were less than 10%. The mean age of patients in eight studies (47%) were over 65, and seven studies (41%) were less than 65, and data were not shown in the other two studies.
Quality assessment
Quality assessments using QUADAS-2 criteria are summarized in Fig. 2. Overall, the quality of the studies was deemed satisfactory.
Prognostic accuracy for mortality using positive qSOFA scores
Figures 3 and 4 showed the forest plots and the 95% confidence regions of the sensitivity and specificity of qSOFA criteria reported in the 24 included studies. The pooled sensitivity of qSOFA across all included studies was 0.58 (95% CI 0.47–0.67), and the specificity was 0.69 (95% CI 0.48–0.84). The pooled estimates of positive and negative likelihood ratios were 1.8 (95% CI 1.1–3.0) and 0.62 (95% CI 0.51–0.70), respectively (Table 2).
In seventeen studies specially focused on the ED patients, the pooled sensitivity of qSOFA across all included studies was 0.54 (95% CI 0.43–0.65), and the specificity was 0.77 (95% CI 0.66–0.86). The pooled estimates of positive and negative likelihood ratios were 2.4 (95% CI 1.8–3.2) and 0.6(95% CI 0.51–0.70), respectively (Table 2). The forest plots and the 95% confidence regions of the sensitivity and specificity are shown in Figs. 5 and 6.
Subgroup analysis for positive qSOFA scores in predicting mortality
Table 3 show the results of univariate meta-regression analysis (prospective, retrospective, single-center, multi-center, in-hospital mortality, 28- or 30-day mortality, scores measured at ED arrival or worst value, suspected or confirmed infection, sepsis or septic shock, overall mortality ≥ 10%, overall mortality < 10%) in identifying potential sources of heterogeneity in studies specially focused on ED patients. Results showed that outcome definition and overall mortality were important sources of heterogeneity. Studies that used in-hospital mortality showed a higher sensitivity and lower specificity than studies that used 28- or 30-day mortality. Studies with overall mortality < 10% showed higher specificity than studies with overall mortality ≥ 10%.
Diagnostic accuracy for sepsis using positive qSOFA scores and SIRS criteria in ED patients
To determine the role of qSOFA and SIRS in the diagnostic accuracy for sepsis, we used the Sepsis3.0 criteria [16] (Sepsis is defined as life-threatening organ dysfunction caused by a dysregulated host response to infection; organ dysfunction can be identified as an acute change in total SOFA score ≥ 2 points consequent to the infection) and focused the studies on ED patients. Five studies included the diagnosis accuracy of sepsis using qSOFA while three studies using SIRS; forest plots for the sensitivity and specificity analysis are shown in Fig. 7. The pooled sensitivity and specificity of positive qSOFA score for diagnosis of sepsis were 0.54 (95% CI 0.50–0.58) and 0.67 (95% CI 0.65–0.68), respectively. The pooled sensitivity and specificity of positive SIRS criteria were 0.72 (95% CI 0.67–0.77) and 0.71 (95% CI 0.69–0.73), respectively. There is no difference in the accuracy of diagnosis of sepsis between positive qSOFA scores and SIRS criteria (P > 0.05) (Table 4).
Discussion
Our meta-analysis evaluated the prognostic capability for predicting mortality and diagnosing sepsis of qSOFA in adult patients outside of ICU with suspected infection. We found that qSOFA was poorly sensitive but highly specific for prediction of mortality. For the studies specially focused on the ED patients, studies that used in-hospital mortality had a higher sensitivity and lower specificity than studies that used 28- or 30-day mortality. Studies with overall mortality < 10% had a higher specificity than studies with overall mortality ≥ 10%. We also found that there is no difference in the accuracy of diagnosis of sepsis between positive qSOFA and SIRS criteria.
Sepsis is a common emergency, and its prognosis is highly affected by the early diagnosis and treatment in the ED [6]. The Sepsis3.0 task force designed qSOFA criteria to replace SIRS to identify patients with suspected infection who would require early diagnosis and treatment [9]. Interestingly, our meta-analysis has found that qSOFA has a poor sensitivity for predicting mortality and diagnosing sepsis in outside of ICU adult patients especially ED patients. As early recognition of sepsis and promptly providing treatment is crucial to improve outcomes, our result will cause great concern about the use of qSOFA in the ED patients.
Our meta-analysis focus on the patients outside of ICU, especially subgroup analysis in ED patients, which is quite different with meta-analysis that published before [11,12,13,14]. Our study confirmed that qSOFA was poorly sensitive (0.54) and moderately specific (0.77) for prediction mortality in ED patients, which was consistent with two studies published before. In Fernando’s study [11], the sensitivity and specificity of qSOFA and SIRS in ED patients subgroup are (0.467, 0.813) and (0.836, 0.306), and in Song’s study [13], the sensitivity and specificity of qSOFA in ED patients subgroup are (0.47, 0.85).
Our meta-analysis has several limitations. First, large amount of heterogeneity still exists among the included studies, although we have investigated some source of heterogeneity through subgroup analysis. Second, the definition of suspected infection varied among studies. Third, some studies applied qSOFA or SIRS score only to specific patients, such as older patients [26], community-acquired pneumonia patients [37], ED patients admitted to intensive care unit [19, 39], which is a potential source of bias. Finally, we found only five studies using positive qSOFA and three studies using positive SIRS criteria for assessing the accuracy of diagnosis of sepsis. The conclusion from this limited data is still farfetched.
Conclusions
In conclusion, our meta-analysis found that qSOFA showed a poor performance in predicting mortality of infected patients outside of ICU, especially in ED. Both qSOFA and SIRS were moderately accurate in diagnosing sepsis. Therefore, combining qSOFA and SIRS may be helpful in predicting mortality. Future studies should focus on combining qSOFA, SIRS, and other Point of Care Testing to accurately assess the diagnosis and prognosis of ED infected patients.
References
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, Kumar A, Sevransky JE, Sprung CL, Nunnally ME, Rochwerg B, Rubenfeld GD, Angus DC, Annane D, Beale RJ, Bellinghan GJ, Bernard GR, Chiche JD, Coopersmith C, De Backer DP, French CJ, Fujishima S, Gerlach H, Hidalgo JL, Hollenberg SM, Jones AE, Karnad DR, Kleinpell RM, Koh Y, Lisboa TC, Machado FR, Marini JJ, Marshall JC, Mazuski JE, McIntyre LA, McLean AS, Mehta S, Moreno RP, Myburgh J, Navalesi P, Nishida O, Osborn TM, Perner A, Plunkett CM, Ranieri M, Schorr CA, Seckel MA, Seymour CW, Shieh L, Shukri KA, Simpson SQ, Singer M, Thompson BT, Townsend SR, Van der Poll T, Vincent JL, Wiersinga WJ, Zimmerman JL, Dellinger RP (2017) Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Crit Care Med. https://doi.org/10.1097/ccm.0000000000002255
Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR (2001) Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 29(7):1303–1310
Lagu T, Rothberg MB, Shieh MS, Pekow PS, Steingrub JS, Lindenauer PK (2012) Hospitalizations, costs, and outcomes of severe sepsis in the United States 2003–2007. Crit Care Med 40(3):754–761. https://doi.org/10.1097/CCM.0b013e318232db65
Wang HE, Jones AR, Donnelly JP (2017) Revised national estimates of emergency department visits for sepsis in the United States. Crit Care Med 45(9):1443–1449. https://doi.org/10.1097/CCM.0000000000002538
Investigators P, Rowan KM, Angus DC, Bailey M, Barnato AE, Bellomo R, Canter RR, Coats TJ, Delaney A, Gimbel E, Grieve RD, Harrison DA, Higgins AM, Howe B, Huang DT, Kellum JA, Mouncey PR, Music E, Peake SL, Pike F, Reade MC, Sadique MZ, Singer M, Yealy DM (2017) Early, goal-directed therapy for septic shock—a patient-level meta-analysis. N Engl J Med 376(23):2223–2234. https://doi.org/10.1056/NEJMoa1701380
Viale P, Tedeschi S, Scudeller L, Attard L, Badia L, Bartoletti M, Cascavilla A, Cristini F, Dentale N, Fasulo G, Legnani G, Trapani F, Tumietto F, Verucchi G, Virgili G, Berlingeri A, Ambretti S, De Molo C, Brizi M, Cavazza M, Giannella M (2017) Infectious diseases team for the early management of severe sepsis and septic shock in the Emergency Department. Clin Infectious Dis 65(8):1253–1259. https://doi.org/10.1093/cid/cix548
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 101(6):1644–1655
Kaukonen KM, Bailey M, Pilcher D, Cooper DJ, Bellomo R (2015) Systemic inflammatory response syndrome criteria in defining severe sepsis. N Engl J Med 372(17):1629–1638. https://doi.org/10.1056/NEJMoa1415236
Seymour CW, Liu VX, Iwashyna TJ, Brunkhorst FM, Rea TD, Scherag A, Rubenfeld G, Kahn JM, Shankar-Hari M, Singer M, Deutschman CS, Escobar GJ, Angus DC (2016) Assessment of clinical criteria for sepsis: for the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 315(8):762–774. https://doi.org/10.1001/jama.2016.0288
Innocenti F, Tozzi C, Donnini C, De Villa E, Conti A, Zanobetti M, Pini R (2018) SOFA score in septic patients: incremental prognostic value over age, comorbidities, and parameters of sepsis severity. Intern Emerg Med 13(3):405–412. https://doi.org/10.1007/s11739-017-1629-5
Fernando SM, Tran A, Taljaard M, Cheng W, Rochwerg B, Seely AJE, Perry JJ (2018) Prognostic accuracy of the quick sequential organ failure assessment for mortality in patients with suspected infection: a systematic review and meta-analysis. Ann Intern Med. https://doi.org/10.7326/m17-2820
Serafim R, Gomes JA, Salluh J, Povoa P (2018) A comparison of the Quick-SOFA and systemic inflammatory response syndrome criteria for the diagnosis of sepsis and prediction of mortality: a systematic review and meta-analysis. Chest 153(3):646–655. https://doi.org/10.1016/j.chest.2017.12.015
Song JU, Sin CK, Park HK, Shim SR, Lee J (2018) Performance of the quick Sequential (sepsis-related) Organ Failure Assessment score as a prognostic tool in infected patients outside the intensive care unit: a systematic review and meta-analysis. Crit Care 22(1):28. https://doi.org/10.1186/s13054-018-1952-x
Maitra S, Som A, Bhattacharjee S (2018) Accuracy of quick Sequential Organ Failure Assessment (qSOFA) score and systemic inflammatory response syndrome (SIRS) criteria for predicting mortality in hospitalized patients with suspected infection: a meta-analysis of observational studies: predictive accuracy of qSOFA: a meta-analysis. Clin Microbiol Infect. https://doi.org/10.1016/j.cmi.2018.03.032
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM, Group Q (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155(8):529–536. https://doi.org/10.7326/0003-4819-155-8-201110180-00009
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC (2016) The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 315(8):801–810. https://doi.org/10.1001/jama.2016.0287
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G, International Sepsis Definitions C (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Intensive Care Med 29(4):530–538. https://doi.org/10.1007/s00134-003-1662-x
Reitsma JB, Glas AS, Rutjes AW, Scholten RJ, Bossuyt PM, Zwinderman AH (2005) Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol 58(10):982–990. https://doi.org/10.1016/j.jclinepi.2005.02.022
April MD, Aguirre J, Tannenbaum LI, Moore T, Pingree A, Thaxton RE, Sessions DJ, Lantry JH (2017) Sepsis clinical criteria in Emergency Department patients admitted to an intensive care unit: an external validation study of quick sequential organ failure assessment. J Emerg Med 52(5):622–631. https://doi.org/10.1016/j.jemermed.2016.10.012
Askim A, Moser F, Gustad LT, Stene H, Gundersen M, Asvold BO, Dale J, Bjornsen LP, Damas JK, Solligard E (2017) Poor performance of quick-SOFA (qSOFA) score in predicting severe sepsis and mortality—a prospective study of patients admitted with infection to the emergency department. Scand J Trauma Resuscitation Emerg Med 25(1):56. https://doi.org/10.1186/s13049-017-0399-4
Churpek MM, Snyder A, Han X, Sokol S, Pettit N, Howell MD, Edelson DP (2017) Quick sepsis-related organ failure assessment, systemic inflammatory response syndrome, and early warning scores for detecting clinical deterioration in infected patients outside the intensive care unit. Am J Respir Crit Care Med 195(7):906–911. https://doi.org/10.1164/rccm.201604-0854OC
Donnelly JP, Safford MM, Shapiro NI, Baddley JW, Wang HE (2017) Application of the Third International Consensus Definitions for Sepsis (Sepsis-3) classification: a retrospective population-based cohort study. Lancet Infect Dis 17(6):661–670. https://doi.org/10.1016/S1473-3099(17)30117-2
Finkelsztein EJ, Jones DS, Ma KC, Pabon MA, Delgado T, Nakahira K, Arbo JE, Berlin DA, Schenck EJ, Choi AM, Siempos II (2017) Comparison of qSOFA and SIRS for predicting adverse outcomes of patients with suspicion of sepsis outside the intensive care unit. Crit Care 21(1):73. https://doi.org/10.1186/s13054-017-1658-5
Forward E, Konecny P, Burston J, Adhikari S, Doolan H, Jensen T (2017) Predictive validity of the qSOFA criteria for sepsis in non-ICU inpatients. Intensive Care Med 43(6):945–946. https://doi.org/10.1007/s00134-017-4776-2
Freund Y, Lemachatti N, Krastinova E, Van Laer M, Claessens YE, Avondo A, Occelli C, Feral-Pierssens AL, Truchot J, Ortega M, Carneiro B, Pernet J, Claret PG, Dami F, Bloom B, Riou B, Beaune S, French Society of Emergency Medicine Collaborators G (2017) Prognostic accuracy of sepsis-3 criteria for in-hospital mortality among patients with suspected infection presenting to the Emergency Department. Jama 317(3):301–308. https://doi.org/10.1001/jama.2016.20329
Gonzalez Del Castillo J, Julian-Jimenez A, Gonzalez-Martinez F, Alvarez-Manzanares J, Pinera P, Navarro-Bustos C, Martinez-Ortiz de Zarate M, Llopis-Roca F, Deban Fernandez M, Gamazo-Del Rio J, Garcia-Lamberechts EJ, Martin-Sanchez FJ, Representing the Infectious Disease Group of the Spanish Emergency Medicine S (2017) Prognostic accuracy of SIRS criteria, qSOFA score and GYM score for 30-day-mortality in older non-severely dependent infected patients attended in the emergency department. Eur J Clin Microbiol Infectious Dis 36(12):2361–2369. https://doi.org/10.1007/s10096-017-3068-7
Guirgis FW, Puskarich MA, Smotherman C, Sterling SA, Gautam S, Moore FA, Jones AE (2017) Development of a simple sequential organ failure assessment score for risk assessment of Emergency Department patients with sepsis. J Intensive Care Med. https://doi.org/10.1177/0885066617741284
Haydar S, Spanier M, Weems P, Wood S, Strout T (2017) Comparison of QSOFA score and SIRS criteria as screening mechanisms for emergency department sepsis. Am J Emerg Med 35(11):1730–1733. https://doi.org/10.1016/j.ajem.2017.07.001
Henning DJ, Puskarich MA, Self WH, Howell MD, Donnino MW, Yealy DM, Jones AE, Shapiro NI (2017) An Emergency Department validation of the SEP-3 sepsis and septic shock definitions and comparison with 1992 consensus definitions. Ann Emerg Med 70(4):544–552. https://doi.org/10.1016/j.annemergmed.2017.01.008 (e545)
Huson MA, Kalkman R, Grobusch MP, van der Poll T (2017) Predictive value of the qSOFA score in patients with suspected infection in a resource limited setting in Gabon. Travel Med Infectious Dis 15:76–77. https://doi.org/10.1016/j.tmaid.2016.10.014
Hwang SY, Jo IJ, Lee SU, Lee TR, Yoon H, Cha WC, Sim MS, Shin TG (2017) Low accuracy of positive qSOFA criteria for predicting 28-day mortality in critically ill septic patients during the early period after emergency department presentation. Ann Emerg Med. https://doi.org/10.1016/j.annemergmed.2017.05.022
Kolditz M, Scherag A, Rohde G, Ewig S, Welte T, Pletz M, Group CS (2016) Comparison of the qSOFA and CRB-65 for risk prediction in patients with community-acquired pneumonia. Intensive Care Med 42(12):2108–2110. https://doi.org/10.1007/s00134-016-4517-y
Moskowitz A, Patel PV, Grossestreuer AV, Chase M, Shapiro NI, Berg K, Cocchi MN, Holmberg MJ, Donnino MW, Center for Resuscitation S (2017) Quick sequential organ failure assessment and systemic inflammatory response syndrome criteria as predictors of critical care intervention among patients with suspected infection. Crit Care Med 45(11):1813–1819. https://doi.org/10.1097/CCM.0000000000002622
Park HK, Kim WY, Kim MC, Jung W, Ko BS (2017) Quick sequential organ failure assessment compared to systemic inflammatory response syndrome for predicting sepsis in emergency department. J Crit Care 42:12–17. https://doi.org/10.1016/j.jcrc.2017.06.020
Peake SL, Delaney A, Bailey M, Bellomo R (2017) Potential Impact of the 2016 consensus definitions of sepsis and septic shock on future sepsis research. Ann Emerg Med 70(4):553–561. https://doi.org/10.1016/j.annemergmed.2017.04.007 (e551)
Quinten VM, van Meurs M, Wolffensperger AE, Ter Maaten JC, Ligtenberg JJM (2017) Sepsis patients in the emergency department: stratification using the clinical impression score, predisposition, infection, response and organ dysfunction score or quick sequential organ failure assessment score? Eur J Emerg Med. https://doi.org/10.1097/mej.0000000000000460
Ranzani OT, Prina E, Menendez R, Ceccato A, Cilloniz C, Mendez R, Gabarrus A, Barbeta E, Bassi GL, Ferrer M, Torres A (2017) New Sepsis Definition (Sepsis-3) and community-acquired pneumonia mortality. A validation and clinical decision-making study. Am J Respir Crit Care Med 196(10):1287–1297. https://doi.org/10.1164/rccm.201611-2262oc
Shetty A, MacDonald SP, Williams JM, van Bockxmeer J, de Groot B, Esteve Cuevas LM, Ansems A, Green M, Thompson K, Lander H, Greenslade J, Finfer S, Iredell J (2017) Lactate ≥ 2 mmol/L plus qSOFA improves utility over qSOFA alone in emergency department patients presenting with suspected sepsis. Emerg Med Aust EMA 29(6):626–634. https://doi.org/10.1111/1742-6723.12894
Wang JY, Chen YX, Guo SB, Mei X, Yang P (2016) Predictive performance of quick sepsis-related organ failure assessment for mortality and ICU admission in patients with infection at the ED. Am J Emerg Med 34(9):1788–1793. https://doi.org/10.1016/j.ajem.2016.06.015
Weigle H, Trigonis R, Bunn D, Krakauer D, Long L, Perkins J (2016) 345 severe sepsis: what gets it right? A comparison of the quick sequential organ failure assessment versus systemic inflammatory response syndrome criteria. Ann Emerg Med 68(4):S132–S133
Williams JM, Greenslade JH, McKenzie JV, Chu K, Brown AFT, Lipman J (2017) Systemic inflammatory response syndrome, quick sequential organ function assessment, and organ dysfunction: insights from a prospective database of ED patients with infection. Chest 151(3):586–596. https://doi.org/10.1016/j.chest.2016.10.057
Acknowledgements
We thank professor Shu-Zhang Cui of Emergency Department of Tianjin Medical University General Hospital for the guidance of analysis.
Funding
This study was supported by grants from the National Natural Science Foundation (nos. 81601714, 81701931, 81871593).
Author information
Authors and Affiliations
Contributions
Y-CL had the idea for and designed the study, searched the scientific literature, collected, analyzed, and interpreted data, and wrote critically revised the report. Y-YL searched the scientific literature, collected data, and drafted and critically revised the report. XZ statistically analyzed and interpreted the data. S-TS, Y-LG, BL and CL helped to search the scientific literature and collect the data. Y-FC had the idea for and designed the study, supervised the study, and gave administrative, technical, and material support.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Statement of human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, YC., Luo, YY., Zhang, X. et al. Quick Sequential Organ Failure Assessment as a prognostic factor for infected patients outside the intensive care unit: a systematic review and meta-analysis. Intern Emerg Med 14, 603–615 (2019). https://doi.org/10.1007/s11739-019-02036-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-019-02036-0