Abstract
Prescription of non-vitamin K antagonist oral anticoagulants (NOACs) requires an assessment of renal function (RF) and the Cockcroft–Gault (CG) equation is traditionally recommended. The objective of the study was to evaluate the potential changes in NOACs management using different equations for estimating RF. In a post hoc analysis of a prospective cohort of patients with atrial fibrillation, we considered different equations: (1) CG for creatinine clearance (CrCl), (2) modification of diet in renal disease (MDRD), (3) CKD-EPI, (4) Berlin Initiative Study 1 (BIS-1) and (5) full age spectrum (FAS), for glomerular filtration rate (GFR). RF was classified according to CrCl in three categories: severely depressed (SD-RF) < 30 ml/min; moderately depressed (MD-RF) 30–49 ml/min; preserved/mildly depressed (P-RF) ≥ 50 ml/min. Concordances in the assignments were analyzed. A population of 402 patients (61.2% males, age 72 ± 11) was categorized according to CrCl: 12 patients (2.9%) as SD-RF, 81 (20.1%) as MD-RF, 309 (76.8%) as P-RF. A potential change in NOACs management could occur using GFR equations rather than CrCl in 16.9% of patients using MDRD formula, in 11.7% using BIS-1, in 14.7% using CKD-EPI and in 12.9% using the FAS equation. Important changes in RF estimates were more frequent in patients aged ≥ 75, but also BMI had a meaningful impact. Use of equations estimating GFR instead of the Cockcroft–Gault equation may result in changes in NOACs management in 12–17% of patients. In the elderly ≥ 75, more pronounced changes in RF classification are detectable according to different equations and NOACs dosing should be further investigated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Oral anticoagulants (OAC) are now the cornerstone of management of patients with atrial fibrillation (AF) [1]. After decades of use of vitamin-K antagonists [2], non-vitamin-K antagonists oral anticoagulant drugs (NOACs) recently became available in clinical practice, on the basis of evidence from randomized controlled trials (RCTs) [3,4,5,6,7,8].
The prescription of NOACs requires an assessment of renal function (RF). In accordance with RCTs, use of the Cockcroft–Gault equation is recommended to estimate creatinine clearance (CrCl) as a guide to eligibility for NOACs (if CrCl is ≥ 30 ml/min) [7, 9, 10] and appropriate NOACs dosing (if CrCl is between 30 and 49) [11] since NOACs elimination depends on RF, reemphasizing the importance of appropriate patient selection, drug dosing, and periodic monitoring of RF [11]. However, assessment of glomerular filtration rate (GFR) and not CrCl is nowadays the mainstay to evaluate renal function for categorizing the various stages of chronic kidney disease, and in daily practice clinicians often estimate GFR from the serum creatinine concentration, using several formulas developed from serum creatinine concentration [12].
In its clinical practice guidelines, the “Kidney Disease: Improving Global Outcome (KDIGO)” group recommends estimation of RF with the Chronic Kidney Disease Epidemiology Collaboration group (CKD-EPI) formula [13], thus evaluating GFR, in contrast with the RCTs on NOACs that uses the Cockcroft–Gault (CG) formula, to guide NOAC prescription.
Aim
The main objective of the study is to evaluate the potential changes in decision making focusing on the prescription NOACs (possibility to prescribe a full or a reduced dose) on the basis of different equations currently available for estimation of RF.
Our aim is also to assess the level of concordance among different equations for estimating the impairment of RF and to identify independent predictors of changes in patient allocation in different categories of RF, when using equations different from the CG formula.
Materials and methods
In this observational study, we analyzed all “real world” patients with AF who were enrolled in two prospective registries, one promoted by the ESC and a spontaneous non-founded one, performed at our Institution during the period between March 2016 and April 2017. No time overlap exists between the two registries. The population consisted of consecutive in- and out-patients presenting with AF to our institution. Both registries, characterized by a similar design and differentiated only by the time course, were approved by our local ethical committee and all the patients provided written informed consent. Atrial fibrillation (AF) was defined as the absence of P waves and irregular R–R interval on electrocardiogram. The types of AF were defined using the classification proposed by the European Society of Cardiology [1].
Inclusion and exclusion criteria
Enrollment required an age of at least 18 years and an ECG-confirmed diagnosis of AF, with a qualifying episode of AF documented in the 12 months prior to enrollment. The presence of AF at the time of inclusion was not required, and AF also need not represent the main reason for admission or referral.
Exclusion criteria were: atrial flutter episodes as the only supraventricular tachyarrhythmia; presence of a prosthetic mechanical valves or at least moderate-to-severe mitral stenosis, the latter characterizing patients as affected by “type 1 valvular AF” [14] and thus not suitable for NOACs according to RCTs and guidelines.
Data collection
For each patient, demographic, clinical, laboratory, and echocardiographic data were prospectively collected, as well as drug prescriptions. Moreover, information about AF pattern time since the first episode, symptoms and co-morbidities was acquired. Thromboembolic and hemorrhagic risks were calculated (CHA2DS2-VASc and HASBLED score) according to European Society of Cardiology guidelines [1].
In a retrospective analysis of the data prospectively collected in our registries, we focused on equations for RF evaluation. For estimating RF, the following equations were used: (1) the Cockcroft–Gault (CG) formula for CrCl [15]; (2) the modification of diet in renal disease (MDRD) [16], (3) CKD-EPI [17], (4) Berlin Initiative Study 1 (BIS-1) 1 [18] and (5) full age spectrum (FAS) [19] equations for GFR.
We also calculate a body surface area adjusted CG (BSA-CG) to reduce shortcomings of CG formula in accordance with Rostoker et al. who propose a modified CG formula taking into account the body surface area (BSA) to improve the accuracy of CrCl estimation [20].
Patients are stratified in three categories of RF on the basis of CrCl, calculated using CG formula, as follows: (1) severely depressed RF (SD-RF) < 30 ml/min; (2) moderately depressed RF (MD-RF) 30–49 ml/min; and (3) preserved/mildly depressed RF (P-RF) ≥ 50 ml/min. Concordance in the assignment to every specific class is analyzed according to different equations. The choice of the cutoffs is in line with the cutoffs commonly used for prescribing the appropriate dose of NOACs [11]. The same cutoff points are applied to the other equations analyzed in the study, in order to guide NOACs prescription, even if they do not correspond to the staging of chronic kidney disease proposed by KDIGO [13].
Statistical analysis
Continuous variables are expressed as mean ± SD, median and range. Among-group comparisons are made using a non-parametric analysis of variance (Kruskal–Wallis test). Categorical variables are reported as number of patients and percentages. Among-group comparisons are made using a χ2 test.
The concordance between the various proposed formulas, considered as the degree of agreement between the two formulae, is evaluated by Cohen’s kappa, which evaluates the consistency, taking into account the concordance due to the case. In practice, the coefficient of concordance (K) evaluates the performance of a formula compared to another (which can represent the clinical gold standard) [21]. Concordance is defined as follows: K < 0.20 poor; 0.20–0.40 modest; 0.41–0.60 moderate; 0.61–0.80 good; > 0.80 excellent [21].
We also calculate the intraclass correlation coefficients in a head-to-head comparison of different formulas estimating renal function, according to the method reported by Shrout and Fleiss [22].
Bland–Altman analysis is also used to compare the different equations for eGFR estimate. In detail, we plot, in a head-to-head fashion, the differences between the different formulas against the mean of the two values. We compare the difference of the two values with 0, and with 1 by means of one-sample t test. We consider outliers to be the cases outside of the upper and lower limits (± 1.96 SD). We do not enter allowed differences between the methods because the ideal allowed difference is 0, allowing to categorize in the same way the cases.
For the evaluation of independent predictors of changes in RF category, which can be associated with a change in the prescription and dosing of anticoagulant therapy, a univariate and stepwise multivariate logistic regression analysis was performed. The variables tested in univariate analysis were: sex, age ≥ 75 years, hypertension, diabetes, heart failure (NYHA class 3 or more or ejection fraction ≤ 40%), coronary artery disease, peripheral artery disease, stroke or systemic embolism, total and major bleedings, valvular disease (defined as the presence of at least moderate aortic or mitral disease or biological prosthetic valve requiring anticoagulation for AF only), dyslipidemia, smoking habit (former + current), alcohol consumption > 8 drink per week, presence of neoplastic disease (prior or current), CHA2DS2-VASc > 0 (> 1 if female), HASBLED score > 2, permanent AF, history of first episode of AF more than a month earlier, severely abnormal maximum indexed left atrial volume (> 48 ml/m2), body mass index (BMI) as a continuous variable.
The multivariate analysis was performed introducing in the model all the variables with a value of p < 0.10 in the univariate analysis.
In the regression analysis, we built two models to avoid considering the same factors twice, once as predictor at univariate analysis and again as part of the CHA2DS2-VASc and HASBLED scores. In the first model, we introduced CHA2DS2-VASc and HASBLED (when statistically eligible) but without the variables suitable for the analysis contributing to calculate the scores. In the second model, regression analysis was performed excluding CHA2DS2-VASc and HASBLED, but introducing the variables nested in those scores, when statistically eligible for the analysis.
The results are presented by the odds ratio (OR), the 95% confidence interval (95% CI), and the p value. Values of p < 0.05 were considered statistically significant.
All analyses were performed using SPSS statistical software version 18.0 and MedCalc version 18.2.
Results
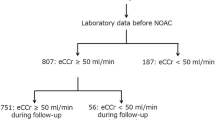
From the original cohort of 413 patients, 11 patients were excluded since AF was associated with prosthetic mechanical valves (9 cases) or mitral stenosis (at least moderate-to-severe) (2 cases), thus excluding candidacy to NOACs.
Population features
We considered 402 patients (246 male; 61.2%), with a mean age of 72 ± 11 (range 18–94 years), with general characteristics shown in Table 1.
According to CrCl, estimated by CG equation, 12 patients (3%) are allocated to the SD-RF group, 81 (20.1%) to the MD-RF group and 309 (76.9%) to the P-RF group. Mean age is 85 ± 4 years in SD-RF group, 80 ± 6 in MD-RF group, 70 ± 11 in P-RF group (p < 0.0001).
A detailed picture of the specific drugs prescribed for anticoagulation in our patients is shown in Table w1 (Supplementary web-only Appendix).
We calculate the percentages of patient re-allocated to each class of RF (corresponding to the cutoffs commonly used for prescribing the appropriate dose of NOACs) (Table 2) for each specific equation used for RF assessment. Some differences are found in the number of patients allocated to each category of eGFR, according to different equations. As shown in Table 2 by re-classifying RF according to CG adjusted for BSA, a change in RF class as compared to CG occurs in 30 cases (7.5%).
A change in RF class occurs in 68 cases (16.9%) using MDRD equation, in 47 cases (11.7%) using BIS-1 equation, in 59 cases (14.7%) using CKD-EPI equation and in 52 cases (12.9%) according to FAS equation.
Independent predictors of changes in RF class as compared to Cockcroft–Gault equation
We analyze what variables at multiple regression analysis are independent predictors of changes in RF class using alternative equations as compared to the classification of RF based on CG formula. The results are shown in Table 3 for individual variables and in the Tables w2–w5 in the Supplementary web-only Appendix.
Age ≥ 75 years predicts a change in RF classification, as compared to the classification based on CG formula, when using any of the equations for eGFR. For MDRD and CKD-EPI, the changes in RF classification, as compared to CG, are affected by many independent variables, while fewer variables condition the changes observed for BIS-1 and FAS equations. A lower BMI significantly changes the RF classification as compared to the classification based on CG, when the MDRD or the CKD-EPI equations are used. As shown in Tables w2–w5, the HAS-BLED score predicts a re-categorization of RF, suggesting that for some equations the patients higher risk of bleeding may have different estimate of RF, with some potential impact on drug dosing and consequent risk of bleeding.
Analysis of concordance among the different equations for estimating RF
Table 4 shows the level of concordance between all the different equations. Using Cohen’s weighted K test for the concordance of attribution to each class of eGFR, we found some degree of agreement between all the categorizations.
For all comparisons, the concordance was moderate (> 0.41) among the various proposed formulae, with the lowest concordance between CG equation and CKD-EPI (weighted K coefficient 0.571 IC 95%; 0.476–0.665) and MDRD equation (0.467 [0.367–0.566]) and the highest values between: (a) CG and BSA-CG equations [weighted K coefficient of 0.803 (0.736–0.869)]; (b) BSA-CG and BIS-1 equations [weighted K coefficient of 0.825 (0.762–0.887)]; CKD-EPI and MDRD equations [weighted K coefficient of 0.816 (0.743–0.888)]; FAS and BIS-1 equations [weighted K coefficient of 0.942 (0.904–0.979)].
Table w6 (Supplementary web-only Appendix) shows the intraclass correlation coefficients for the head-to-head comparisons of different formulas in estimating the allocation to specific RF classes. Compared with CG equation, BSA-CG showed the highest reliability and correlation, followed by FAS and BIS-1, while MDRD had the lowest reliability.
Comparing CG estimates with the results of other formulas, the mean differences with the Bland–Altman test were always significantly different from 0 (p < 0.05). The plots of differences between CG and other formulas against the arithmetic mean of the same comparison are shown in figure w1 to w4. The outliers were 22 (5.5%) comparing CG with MDRD, 17 (4.2%) with BIS-1, 16 (4%) with CKD-EPI and 22 (5.5%) with FAS equation.
Discussion
Our results show that using the equations proposed for estimating GFR may imply that for every 6–9 patients the different categorization of RF could result in a substantially different management of NOACs, in terms of drug dosing or even avoidance of prescription according to the evidence-based recommendations.
According to the Food and Drug Administration (FDA) Guidance for Industry, published in 1998 and directed to pharmaceutical companies and researchers, drug dosing has been traditionally based on pharmacokinetic studies where kidney function is assessed using creatinine clearance levels estimated from the CG equation [23]. However, the accuracy of CG equation in estimating RF is questionable, especially when age and BMI are at extreme ranges [24], and in a study focused on classification of RF according to classes proposed by the FDA, the MDRD equation, as compared to CG equation, has a greater rate of concordance with the gold standard of GFR measured with inulin clearance for both assignment to RF categories recommended by the FDA and adjustment of specific drug dosing [25]. In another comparative study using inulin clearance as the gold standard for RF evaluation in individuals with and without kidney dysfunction, the MDRD equation is slightly more precise than the CG equation, but only at a low GFR, and the limitations of CG in comparison with the gold standard are evident, with CG leading to overestimation of RF in obesity, and underestimation in underweight and older age patients [24].
In recent studies evaluating also CKD-EPI, always using inulin clearance as the gold standard for RF evaluation, the CKD-EPI formula gives the best overall accuracy and agreement after classification in subgroups of GFR [17, 26], while MDRD has the best diagnostic accuracy when GFR ranges from 15 to 29 ml/min per 1.73 m2 [26]. More recently, the BIS-1 equation is proposed to principally analyze eGFR in elderly populations: this equation is created using 3 variables (age, gender and serum creatinine) to avoid the risk of RF overestimation that use of CG, MDRD and CKD-EPI equations may imply in elderly subjects [18]. BIS-1 represents the first attempt to tailor a formula to the aged population. Another formula recently proposed, the FAS equation, is found to have improved validity and continuity across the full age spectrum and to overcome the problem of implausible eGFR assessment in the elderly [19].
In clinical practice, clinicians have to face the difficulty of choosing the right formula for the right patient to start the right treatment according to a reliable assessment of RF. According to our data, the grading of RF impairment may change according to the specific equation adopted for estimating RF and management of NOAC may consequently vary since the concordance between CG formula and other equations, specifically the MDRD or CKD-EPI equations, is suboptimal.
In a more general view, not limited to NOACs prescription, it is unclear which formula can be recommended for clinical practice among the many equations proposed for calculating eGFR on the basis of serum creatinine [13, 27]. The KDIGO document recommends use of the CKD-EPI equation [13], while randomized trials exploring NOACs versus warfarin used the CrCl estimate by CG equation [3,4,5,6, 11, 27, 28]. Moreover, many laboratories report eGFR calculated with MDRD formula, as a routine when serum creatinine is measured. Every clinician should perhaps be informed about the existence of limited concordance and potentially different information impacting on clinical decision making.
The main differences that we found in the allocation of patients to a specific class of RF more frequently were related to patients initially classified in the group with MD-RF according to CrCl estimated by the CG equation. In our study, only 3% of patients with AF had an SD-RF according to the reference equation for NOACs prescription, i.e., CG equation. This percentage is in agreement with findings from large registries, meta-analyses and observational studies conduced in AF patients, for example, 2.0% in the Global Anticoagulant Registry in the FIELD (GARFIELD) study [29], 2.7% in the Danish national registries [30], and 3.7% in EORP-AF general pilot registry [31].
Patients with impairment in RF are at increased risk for thromboembolic and bleeding events, especially if the impairment is severe [30, 32]. An increased risk of bleeding was reported in very old (≥ 80 years) patients treated with vitamin-K antagonist and was similarly predicted by CG, MDRD and CKD-EPI formulas [33], but this finding needs to be reassessed in the context of treatment with NOACs in view of the importance of renal function for NOAC dosing in the specific context of very old and more vulnerable patients. According to the current guidelines [1], patients with a CrCl < 30 ml/min are not recommended NOACs. The factor Xa inhibitors are currently approved in Europe and in the U.S. for use in patients with CrCl 15–30 mL/min, with a reduced dose regimen only on the basis of pharmacokinetic data, since no controlled data on outcomes in terms of effectiveness and safety are available in patients with advanced CKD (CrCL < 25–30 mL/min) [11].
Our study shows that prescription and management of NOACs, in view of their important dependence on RF, could vary in a substantial proportion of patients according to the use of different formulae for RF classification and that this may have important implications on NOACs dosing, as well as on the possibility to actually prescribe the drug according to available evidence. Using MDRD, BIS-1, CKD-EPI and FAS equations, instead of the CG formula, from one- to two-thirds of the patients initially allocated to the SD-RF group were changed their allocation category and moved to a higher eGFR group (Table 2).
A similar variation is found for MD-RF group, since using MDRD or CKD-EPI equations, a great proportion of patients (59.3 and 46.9%, respectively) modified RF class allocation. On the other hand, when using BIS-1 and FAS formulae, this allocation change is found in a lower percentage of patients (22.2 and 25.9%, respectively). This phenomenon is less evident when analyzing the patients allocated to the P-RF group on the basis of CG formula, since reallocation occurs in around 4–8% of cases. The limited agreement between the CG equation and every alternative eGFR equation taken into account, found with Cohen’s weighted k, is also confirmed by the Bland–Altman test.
Discordance between MDRD, CKD-EPI and CG formulas with regard to dosing of NOACs has also been reported by Manzano-Fernandez et al. [34]. Similar analyses comparing BIS-1 and FAS equations to mentioned formulae in AF patients are lacking and, in this perspective, our study provides novel inputs for clinical management of NOACs, that could be considered for additional prospective studies.
In view of our results, if an equation for eGFR has to be selected as an alternative to the traditional evaluation of CrCl with the Cockcroft Gault equation, the BIS-1 equation should be the object of special consideration in view of a better concordance as compared with other equations for eGFR, combined with the better precision and accuracy demonstrated for patients aged 70 years or older [18]. In view of the limitations of the CG equation in appropriately estimating RF as compared to the gold standard of inulin clearance [24, 25], prospective evaluations considering the safety and efficacy of NOACs prescriptions on the basis of the newest formulas for eGFR should be promoted, especially in the elderly aged ≥ 75 years. Indeed, an advanced age (≥ 75 years) is an independent predictor of changes in RF class with any of the equations for eGFR that were tested and, therefore, further studies on NOACs management according to RF are especially needed in this group of patients, usually the most fragile with regard to both thrombotic and hemorrhagic events. Also, patients at the extremes of BMI deserve additional investigations for appropriate assessment of RF and NOACs dosing.
The National Kidney Disease Education Program (NKDEP) updated its guidelines in 2009, indicating the use of either the CG equation for CrCl or the MDRD equation for eGFR for appropriate drug dosing according to RF [35]. Also, the FDA updated in 2010 the guidance, by recommending that manufacturers have to provide drug dosing recommendations on the basis of both an eCrCl and eGFR assessment [36]. Unfortunately, during the development of NOACs dosing recommendations did not consider eGFR and further investigation targeted to further NOACs safety and efficacy according to a different approach to drug dosing, especially in some patients subgroups (elderly, extremes of body weight, etc.) .
Our finding are of interest for the planning of future cohort studies targeted to evaluate the impact in terms of safety (bleeding) and efficacy (stroke or systemic embolism) of clinical use, as an alternative to CG formula, of one of the equations proposed for eGFR, in accordance with the guidance released by FDA in 2010 recommending indications on drug dosing on the basis of both eCrCl and eGFR assessments [36].
Our study has some limitations, linked to its observational nature and we cannot exclude the presence of some confounding unmeasured factors, or binarily categorized variables. For RF classification, we used the cutoff points of FDA that differ from those of the National Kidney Foundation thresholds for normal and mild renal impairment (90 and 60, respectively) [37], but our intention was a comparison with limits for NOACs prescription and not grading a renal dysfunction. Another caveat could be the comparison between CG equation (that estimate CrCl) and formulas that estimate eGFR (that are indexed for BSA approximated to 1.73 m2) can be an object of criticism; however, the CG equation adjusted by BSA has been also considered, even if it is rarely used in daily practice and not recommended by guidelines on NOACs management [1, 10, 11]. To allow more accurate comparisons, other authors [38] have “de-normalized” the results of the equations to avoid over or underestimation in overweight or skinny patients; but in the daily practice this approach is not usually applied.
In consideration of the observational nature of our study, a direct measurement of GFR using clearance of inuline or of another marker was not available in our patient population. We, therefore, followed usual practice, which considers that an estimation of GFR may be sufficient for clinical decision making [39].
Conclusions
NOACs management requires careful estimation of RF and the use of the Cockcroft–Gault equation has been traditionally suggested. However, the known limitations of the CG equation in estimating RF as compared to evaluations of RF based on inulin clearance, and the indication from FDA that equations for estimating GFR can be an alternative to the Cockcroft–Gault equation for drug dosing, suggest the need to investigate the impact of equations for eGFR on clinical management of NOACs. We find in an observational study that when evaluating patients with AF for prescription and dosing of NOACs, adoption of the equations proposed for estimating GFR instead of the Cockcroft–Gault equation for estimating CrCl implies that in every 6–9 patients, the different classification of RF results in a substantially different management of NOACs in terms of drug dosing or even avoidance of prescription according to evidence-based recommendations.
Moreover, the most pronounced changes in RF classification using equations for eGFR are detected in the elderly aged ≥ 75. In view of the vulnerability and frailty of most of these patients, further studies on NOACs dosing according to the equations available for eGFR evaluation should be promoted in this setting, as well as at the extremes of BMI.
References
Kirchhof P, Benussi S, Kotecha D et al (2016) 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. The Task Force for the management of atrial fibrillation of the European Society of Cardiology (ESC), Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC, endorsed by the European Stroke Organisation. Eur Heart J
Hart RG, Pearce LA, Aguilar MI (2007) Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med 146:857–867
Connolly SJ, Ezekowitz MD, Yusuf S et al (2009) Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 361:1139–1151
Patel MR, Mahaffey KW, Garg J et al (2011) Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med 365:883–891
Granger CB, Alexander JH, McMurray JJ et al (2011) Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med 365:981–992
Giugliano RP, Ruff CT, Braunwald E et al (2013) Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med 369:2093–2104
Ruff CT, Giugliano RP, Braunwald E et al (2014) Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet 383:955–962
Lip G, Freedman B, De Caterina R, Potpara TS (2017) Stroke prevention in atrial fibrillation: Past, present and future. Comparing the guidelines and practical decision-making. Thromb Haemost 117:1230–1239
Camm AJ, Lip GY, De Caterina R et al (2012) 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J 33:2719–2747
Devereaux PJ, Yang H, Yusuf S et al (2008) Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): a randomised controlled trial. Lancet 371:1839–1847
Heidbuchel H, Verhamme P, Alings M et al (2015) Updated European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist anticoagulants in patients with non-valvular atrial fibrillation. Europace 17:1467–1507
Stevens LA, Coresh J, Greene T, Levey AS (2006) Assessing kidney function–measured and estimated glomerular filtration rate. N Engl J Med 354:2473–2483
(2013) KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney international 3:1–150
Lip GYH, Collet JP, Caterina R et al (2017) Antithrombotic therapy in atrial fibrillation associated with valvular heart disease: a joint consensus document from the European Heart Rhythm Association (EHRA) and European Society of Cardiology Working Group on Thrombosis, endorsed by the ESC Working Group on Valvular Heart Disease, Cardiac Arrhythmia Society of Southern Africa (CASSA), Heart Rhythm Society (HRS), Asia Pacific Heart Rhythm Society (APHRS), South African Heart (SA Heart) Association and Sociedad Latinoamericana de Estimulación Cardíaca y Electrofisiología (SOLEACE). Europace 19:1757–1758
Cockcroft DW, Gault MH (1976) Prediction of creatinine clearance from serum creatinine. Nephron 16:31–41
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 130:461–470
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Schaeffner ES, Ebert N, Delanaye P et al (2012) Two novel equations to estimate kidney function in persons aged 70 years or older. Ann Intern Med 157:471–481
Pottel H, Hoste L, Dubourg L et al (2016) An estimated glomerular filtration rate equation for the full age spectrum. Nephrol Dial Transplant 31:798–806
Rostoker G, Andrivet P, Pham I, Griuncelli M, Adnot S (2007) A modified Cockcroft-Gault formula taking into account the body surface area gives a more accurate estimation of the glomerular filtration rate. J Nephrol 20:576–585
Viera AJ, Garrett JM (2005) Understanding interobserver agreement: the kappa statistic. Fam Med 37:360–363
Shrout PE, Fleiss JL (1979) Intraclass correlations: uses in assessing rater reliability. Psychol Bull 86:420–428
(1998) Food and Drug Administration: guidance for industry: pharmacokinetics in patients with impaired renal function— study design, data analysis, and impact on dosing and labeling. Department of Health and Human Services, Rockville, May. https://www.fda.gov/downloads/drugs/guidances/ucm204959.pdf
Cirillo M, Anastasio P, De Santo NG (2005) Relationship of gender, age, and body mass index to errors in predicted kidney function. Nephrol Dial Transplant 20:1791–1798
Stevens LA, Nolin TD, Richardson MM et al (2009) Comparison of drug dosing recommendations based on measured GFR and kidney function estimating equations. Am J Kidney Dis 54:33–42
Michels WM, Grootendorst DC, Verduijn M, Elliott EG, Dekker FW, Krediet RT (2010) Performance of the Cockcroft-Gault, MDRD, and new CKD-EPI formulas in relation to GFR, age, and body size. Clin J Am Soc Nephrol 5:1003–1009
Boriani G, Savelieva I, Dan GA et al (2015) Chronic kidney disease in patients with cardiac rhythm disturbances or implantable electrical devices: clinical significance and implications for decision making-a position paper of the European Heart Rhythm Association endorsed by the Heart Rhythm Society and the Asia Pacific Heart Rhythm Society. Europace 17:1169–1196
January CT, Wann LS, Alpert JS et al (2014) 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 64:e1–76
Kakkar AK, Mueller I, Bassand JP et al (2013) Risk profiles and antithrombotic treatment of patients newly diagnosed with atrial fibrillation at risk of stroke: perspectives from the international, observational, prospective GARFIELD registry. PLoS One 8:e63479
Olesen JB, Lip GY, Kamper AL et al (2012) Stroke and bleeding in atrial fibrillation with chronic kidney disease. N Engl J Med 367:625–635
Boriani G, Laroche C, Diemberger I et al (2016) Glomerular filtration rate in patients with atrial fibrillation and 1-year outcomes. Sci Rep 6:30271
Fanikos J, Burnett AE, Mahan CE, Dobesh PP (2017) Renal function considerations for stroke prevention in atrial fibrillation. Am J Med 130(9):1015–1023
Lip GY, Andreotti F, Fauchier L et al (2011) Bleeding risk assessment and management in atrial fibrillation patients: a position document from the European Heart Rhythm Association, endorsed by the European Society of Cardiology Working Group on Thrombosis. Europace 13:723–746
Manzano-Fernández S, Andreu-Cayuelas JM, Marín F et al (2015) Comparison of estimated glomerular filtration rate equations for dosing new oral anticoagulants in patients with atrial fibrillation. Rev Esp Cardiol (Engl Ed) 68:497–504
NKDEP (2010) NKDEP. National Kidney Disease Education Program. Chronic kidney disease and drug dosing: information for providers. http://www.nkdep.nih.gov/professionals/CKD_DrugDosing_508.pdf
(2010) US Food and Drug Administration (2010). Draft guidance for industry: pharmacokinetics in patient with impaired kidney function—study design DA, and impact on dosing and labeling. http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM204959.pdf
Levey AS, Coresh J, Balk E et al (2003) National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med 139:137–147
Hawkins NM, Jhund PS, Pozzi A et al (2016) Severity of renal impairment in patients with heart failure and atrial fibrillation: implications for non-vitamin K antagonist oral anticoagulant dose adjustment. Eur J Heart Fail 18:1162–1171
Stevens LA, Levey AS (2009) Measured GFR as a confirmatory test for estimated GFR. J Am Soc Nephrol 20:2305–2313
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Statements on human and animal rights
The study had been approved by the appropriate institutional research ethics committee. All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Gregory Yoke Hong Lip and Giuseppe Boriani are joint senior authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Malavasi, V.L., Pettorelli, D., Fantecchi, E. et al. Variations in clinical management of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation according to different equations for estimating renal function. Intern Emerg Med 13, 1059–1067 (2018). https://doi.org/10.1007/s11739-018-1857-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-018-1857-3