Abstract
Self-administered adrenaline through an auto-injector is the main out-of-hospital treatment for anaphylaxis, and patients should be trained to promptly and correctly use the device. The aim of the study was to verify the proper use of the device and the correct drug administration, and to identify possible misuse by patients. In seven Italian Allergy clinics, patients who were previously provided with self-injectable adrenaline were recruited at the follow-up visit required for the renewal of their prescription. All patients completed a questionnaire covering details of their allergic reactions, and knowledge of the device. The correct use was verified by the physician using a trainer with a four-step examination. 242 patients were included; 46 patients (18 %) did not always carry the auto-injector, and 35 patients (14 %) reported situations in which they were doubtful about whether to use adrenaline. Only 39 % of patients properly managed the device, while some patients (6 %) failed in all four steps. The majority of patients considered it appropriate to use adrenaline at the onset of respiratory symptoms (56 %). The factor most closely related to proper use of the device was the education of the patient (p = 0.03), while age and the time from first prescription did not affect the ability to properly use the auto-injector. Even though accurate training is conducted, many patients are still unable to properly use the adrenaline auto-injector in case of anaphylaxis. Allergists should review the instructions provided to the patients every time a renewal of the auto-injector is prescribed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anaphylaxis is a severe systemic hypersensitivity reaction that can be elicited by different stimuli, and can involve multiple organs [1]. In European countries, it affects one in 300 of the population at some time in their lives [2]. Intramuscular adrenaline is the drug of choice for the treatment of anaphylaxis [1]. Delay in injecting adrenaline can result in a more severe prognosis or fatalities; therefore, early treatment of anaphylaxis is a priority to decrease anaphylaxis-related mortality and morbidity [3]. Because most cases of anaphylaxis develop outside the hospital, patients at risk of anaphylaxis must always carry the adrenaline auto-injector, and use it promptly and correctly in the setting of anaphylaxis [4]. Some different devices for self-administration of adrenaline are available for patients. However, these devices are subject to a possible misuse by patients and their families or caregivers [5]. Different factors have been associated to fatal anaphylaxis despite treatment with adrenaline: incorrect dose, failure to inject all the dose, delayed administration or an incorrect route of administration [6]. Moreover, adrenaline underuse is common in the community setting: in a survey, in 1885 patient survivors of anaphylaxis in the community, 73 % were non-users [7]; in a pediatric population of patients with food allergy, only 16.7 % of patients experiencing anaphylaxis used an adrenaline auto-injector [8]. It must also be considered that errors in handling the auto-injector can lead to unintentional injection, usually in a finger [9]. For all these reasons, patients’ familiarity with the use of the auto-injector device is crucial. The aim of this study was to verify the proper use of the device, the correct administration of drug, and to identify possible misuse by patients at risk of anaphylaxis.
Methods
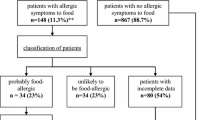
Consecutive patients, who had been diagnosed with anaphylaxis and who were previously provided with self-injectable adrenaline, were recruited at the follow-up visit, required for the renewal of the prescription, in seven Italian allergy clinics (Parma, Piacenza, Brescia, Verona, Padova, Mantova, Bergamo) between July and December 2013. In Italy, in fact, adrenaline auto-injector is provided and paid by the National Health System after prescription by an allergy specialist. The prescription must be renewed every 1 or 2 years after assessment of the continuing risk of anaphylaxis. All patients had received verbal or written information by an allergist about indications when adrenaline should be administered, and they were trained in administration with an appropriate trainer device on the occasion of the first prescription and subsequent follow-up visits. Participants were adult or adolescent patients who had been prescribed an adrenaline auto-injector for at least 1 year. There were no specific exclusion criteria apart from age. All patients completed a questionnaire covering demographic data, time from the first prescription, details of allergic reactions and knowledge of the device. If self-injectable adrenaline was used, patients were asked if other anti-allergic medications (antihistamine corticosteroids, beta2-agonists) were administered during the reactions before adrenaline or together with it. They were also asked when they would use the adrenaline auto-injector in case of exposure to the allergen. Finally, patients were asked to demonstrate how they use the auto-injector using a trainer injector without needles and medication, but otherwise identical to the original auto-injector prescribed to the patient, supplied by the manufacturers (Fastjekt® Trainer, MedaPharma, Solna, Sweden or Jext® Trainer, AlkAbellò, Horsholm, Denmark). This practical examination was scored in four steps that consisted of (1) removing correctly the safety cap, (2) properly handling the auto-injector, (3) selecting the mid-anterolateral thigh as the correct site of injection, (4) holding the auto-injector in place for at least 10 s. All participants gave their informed consent. The study was approved by the Ethics Committee of Guglielmo da Saliceto Hospital, Piacenza, Italy.
Statistical analysis
Stata software version 9.2 (STATA Corps, USA) was used for statistical analysis. Comparisons between groups were performed with Chi-squared test or Fisher exact test (if cells with small values). Associations between different variables and the ability in the use of the auto-injector were assessed using logistic regression analysis. p values less than 0.05 were regarded as statistically significant.
Results
A total of 246 patients were screened, four of whom, aged <12 years, were excluded as they could not be responsible for administering the medication, and it was not possible to carry out the assessment of the correct use of the device by trainer. Thus, 242 patients (mean age 42.6 ± 17.7 years; male 115, female 127) were included in the study. None refused to participate. Prescription indication included food allergy in 107 patients, hymenoptera venom allergy in 129 patients, latex allergy in five patients, and idiopathic anaphylaxis in one patient. Self-injectable adrenaline was prescribed a mean of 4.3 years prior the enrollment (range between 1 and 9 years) (Table 1). The self-injectable adrenaline had been used by 18 patients (7.4 %) for allergic reactions (13 patients with hymenoptera venom allergy and five with food allergy); 82 % of patients responded that they had the device with them at all times, while 44 patients (18 %, 25 with hymenoptera venom allergy and 19 with food allergy) did not always carry on the auto-injector; the difference between the two groups of patients was not significant; 35 patients (14 %) reported situations in which they were uncertain whether to use adrenaline, also in that case without significant difference between those with hymenoptera venom allergy compared to those with food allergy. If a suspected contact with the culprit allergen occurred, 23 % indicated that they would inject adrenaline for cutaneous symptoms, 56 % at onset of respiratory symptoms, 1 % at onset of gastrointestinal symptoms and 19 % only for hypotension and shock; 72.5 % of patients reported that their family members were trained in the use of the auto-injector, and would be able to administer the drug in case of anaphylaxis. The results of the demonstration by patients are shown in Table 2.
Although 93 % of patients responded that they believed they knew the correct use of the auto-injector, only 39 % of patients showed all four steps of auto-injector use correctly, while the majority committed at least one error; 15 patients (6 %) failed in all four steps. The major misuses were the following: 53 patients (22 %) did not correctly pull off the safety cap, 63 patients (26 %) did not handle the injector correctly, in 90 patients (37 %) the site of injection was wrong and 92 patients (38 %) did not hold in place the injector for 10 s. Among the 18 patients who used self-injectable adrenaline, 11 (61 %) properly managed the device while seven patients failed at least one step (Table 3); none failed all the steps. Compared to non-users, the number of user patients who performed all four steps correctly was significantly higher (61 vs 37 %, p = 0.04); 39 % of them had taken antihistamine and corticosteroids before adrenaline auto-injector or together with it. In the multivariate analysis, the factor most closely related to the proper use of the device was the education of the patient (p = 0.03). Age was inversely related to the proper use of the auto-injector, significantly in the univariate analysis (p = 0.02) but not in multivariate analysis (p = 0.15). The time from first prescription did not affect the ability to properly use the auto-injector.
Discussion
Adrenaline by intramuscular injection is the mainstay of emergency drug treatment of anaphylaxis, because it is the only agent rapidly counteracting the effects on target organs of the mediators released by mast cells and basophils following the exposure to the culprit allergen [10]. However, there is evidence that adrenaline is significantly underused by physicians, especially in the emergency department, while it is more frequently used by most allergists when they must directly treat anaphylactic reactions [11–13]. Due to the need of an immediate intervention at the onset of the reaction, patients should be able to administer adrenaline by themselves. Adrenaline sublingual tablets are currently under development to offer to patients a way of administration more friendly than the injection [14, 15], but today the only available formulations for patients are the auto-injectors, that have been demonstrated to be effective and safe in both adults and children, even though no placebo-controlled trials have been conducted for obvious ethical reasons [16]. However, as for physicians, patients also use adrenaline much less than needed. In the 2000s, one study addressed a population of children with recurrent episodes of anaphylaxis, and reports that the auto-injector device was used in only 29 % of cases [17].Such low use is confirmed in more recent studies in adolescents [18, 19] and adults [20]. The most recent study involved children and teenagers recruited in 14 pediatric allergy clinics in UK, and shows that an adrenaline auto-injector was used only by 16.7 % of participants experiencing anaphylaxis [8]. It is important to understand why most patients do not use adrenaline. A questionnaire-based survey explored the barriers to carriage or use of auto-injectors: inconsistent health professional advice, perceived stigma of carrying a ‘weapon-like’ device, poor device design and limited patient training were identified as the most frequent barriers [21]. In the study from UK, the most common reasons given by patients for not using the auto-injector were ‘thought adrenaline unnecessary’ (54.4 %) and ‘unsure adrenaline necessary’ (19.1 %) [8]. In addition, to use the auto-injector is not enough, because the device must be handled correctly to make adrenaline effective.
We investigated the proper use of adrenaline auto-injectors in a real-life population of adolescent and adult patients at risk of anaphylaxis, who were already prescribed and trained in the correct use of the adrenaline auto-injector by allergists. The assessment was made during a routine follow-up visit that patients underwent at regular intervals. Despite all patients being trained in the administration of the adrenaline auto-injector at the time of the first prescription and during subsequent follow-up visits, only 39 % could demonstrate a correct use of the device, while most patients could not simulate the administration in a fully correct manner. This is a serious concern since they would not be able to successfully manage a life-threatening allergic reaction in the community setting. These rates are similar to the rates reported by Sicherer et al. [22] and Topal et al. [23] in children and parents of allergic pediatric patients. In these studies, 38 and 39.4 % of subjects correctly used the device, and the most common errors were the removal of safety cap and holding the injector in place. In another recent study, in a group of 101 patients, 56 % missed three or more steps, the most common error being not holding the auto-injector in place for at least 10 s after triggering [24]. Using a different scoring system, Segal and collaborators find that only 5.6 % of subjects perform the five steps of the procedure correctly [25]. Nevertheless, the authors document the positive effect of reinstruction on children’s and parents’ ability to use the device. Age and the time since the first prescription do not influence the ability to use the device, while patients who have used adrenaline in the past and patients with higher education show greater skills in the use of their auto-injector. More than a third of patients who report auto-injector use made at least one error with the trainer device. In a real setting of anaphylaxis, these errors could compromise the proper administration of the drug. Moreover, though accidental exposures to the allergen can occur despite avoidance measures, almost one-fifth of patients report that they do not always carry on the auto-injector. This suggests the need to reinforce patients’ education. Moreover, the patient’s preference for a particular device should be taken into account. A user-centered design process led to the development of two prototype adrenaline auto-injectors (INT01 and INT02) providing a unidirectional perceived injection end, a self-retracting needle, and, with INT02, voice instructions to guide the administration. Compared with the available EpiPen and Twin-Ject, the rate of preference is higher for the new devices, and significantly higher for INT02 [26].Recently, Camargo et al. in a large number of adults, children and caregivers tested the preference for the new auto-injector Auvi-Q, that provides audio and visual cues for patients, versus EpiPen with regard to method of instruction, preference to carry, and device size and shape. The new device is preferred by patients and caregivers regardless of their being experienced or inexperienced in the self-management of anaphylaxis [27]. However, simple modifications, such as changing in EpiPen the gray safety cap to red, placing a yellow arrow pointing to the black injection tip, and providing a written and visual instruction sheet for each trainer device, were also effective in increasing its correct use and decreasing common errors by untrained users [28].
In conclusion, our survey, conducted in a real-life setting in which patients at risk of anaphylaxis attend routine follow-up visits, shows that the training of patients made by an allergist does not guarantee the persistence of the acquired competency in the adrenaline auto-injector, and this suggests the necessity to repeat training at all visits to improve patients’ abilities. Moreover, primary care physicians and other health care workers such as pharmacists should also be actively involved in the education of patients at risk of anaphylaxis.
References
Simons FE, Ardusso LR, Bilò MB, El-Gamal YM, Ledford DK, Ring J, World Allergy Organization et al (2011) World Allergy Organization guidelines for the assessment and management of anaphylaxis. World Allergy Organ J 4:13–37
Panesar SS, Javad S, de Silva D, Nwaru BI, Hickstein L, Muraro A, EAACI Food Allergy and Anaphylaxis Group et al (2013) The epidemiology of anaphylaxis in Europe: a systematic review. Allergy 68:1353–1361
Pumphrey RSH (2000) Lessons for management of anaphylaxis from a study of fatal reactions. Clin Exp Allergy 30:1144–1150
Rudders SA, Banerji A (2013) An update on self-injectable epinephrine. Curr Opin Allergy Clin Immunol 13:432–437
Song TT, Worm M, Lieberman P (2014) Anaphylaxis treatment: current barriers to adrenaline auto-injector use. Allergy. doi:10.1111/all.12387
Simons FE (2004) First-aid treatment of anaphylaxis to food: focus on epinephrine. J Allergy Clin Immunol 113:837–844
Simons FE, Clark S, Camargo CA Jr (2009) Anaphylaxis in the community: learning from the survivors. J Allergy Clin Immunol 124:301–306
Noimark L, Wales J, Du Toit G, Pastacaldi C, Haddad D, Gardner J et al (2012) The use of adrenaline autoinjectors by children and teenagers. Clin Exp Allergy 42:284–292
Carrascosa MF, Gallastegui-Menéndez A, Teja-Santamaría C, Caviedes JR (2013) Accidental finger ischaemia induced by epinephrine autoinjector. BMJ Case Rep 2013:18. doi:10.1136/bcr-2013-200783
Simons FE, Ardusso LR, Bilò MB, Dimov V, Ebisawa M, El-Gamal YM, World Allergy Organization et al (2012) 2012 update: World Allergy Organization guidelines for the assessment and management of anaphylaxis. Curr Opin Allergy Clin Immunol 12:389–399
Banerji A, Rudders S, Clark S, Wei W, Long AA, Camargo CA Jr (2014) Retrospective study of drug-induced anaphylaxis treated in the emergency department or hospital: patient characteristics, management, and 1-year follow-up. J Allergy Clin Immunol Pract 2:46–51
Sclar DA, Lieberman PL (2014) Anaphylaxis: underdiagnosis, underreported, and undertreated. Am J Med 127(1 Suppl):A1–A5
Fineman S, Dowling P, O’Rourke D (2013) Allergists’ self-reported adherence to anaphylaxis practice parameters and perceived barriers to care: an American College of Allergy, Asthma and Immunology member survey. Ann Allergy Asthma Immunol 111:529–536
Muraro A, Roberts G, Simons FE (2008) New visions for anaphylaxis: an iPAC summary and future trends. Pediatr Allergy Immunol 19(Suppl 19):40–45
Rawas-Qalaji MM, Rachid O, Simons FE, Simons KJ (2013) Long-term stability of epinephrine sublingual tablets for the potential first-aid treatment of anaphylaxis. Ann Allergy Asthma Immunol 111:568–570
Sheikh A, Simons FE, Barbour V, Worth A (2012) Adrenaline auto-injectors for the treatment of anaphylaxis with and without cardiovascular collapse in the community. Cochrane Database Syst Rev 8:CD008935
Gold MS, Sainsbury R (2000) First aid anaphylaxis management in children who were prescribed an epinephrine autoinjector device (EpiPen). J Allergy Clin Immunol 106:171–176
Gallagher M, Worth A, Cunningham-Burley S, Sheikh A (2011) Epinephrine auto-injector use in adolescents at risk of anaphylaxis: a qualitative study in Scotland, UK. Clin Exp Allergy 41:869–877
Floxtra-de Blok BM, Doriene van Ginkel C, Roerdink EM, Kroeze MA, Stel AA, van der Meulen GN, Dubois AE (2011) Extremely low prevalence of epinephrine autoinjectors in high-risk food-allergic adolescents in Dutch high schools. Pediatr Allergy Immunol 22:374–377
Amirzadeh A, Verma P, Lee S, Klaustermeyer W (2010) Epinephrine auto-injector use and demographics in a veterans administration population. Allergy Asthma Proc 31:304–307
Money AG, Barnett J, Kuljis J, Lucas J (2013) Patient perception of epinephrine auto-injectors: exploring barriers to use. Scand J Caring Sci 27:335–344
Sicherer SH, Forman JA, Noone SA (2000) Use assessment of self-administered epinephrine among food-allergic children and pediatricians. Pediatrics 105:359–362
Topal E, Bakirtas A, Yilmaz O, Ertoy IH, Arga M, Demirsoy MS, Turktas I (2013) A real-life study on acquired skills from using an adrenaline autoinjector. Int Arch Allergy Immunol 160:301–306
Bonds RS, Asawa A, Ghazi AI (2015) Misuse of medical devices: a persistent problem in self-management of asthma and allergic disease. Ann Allergy Asthma Immunol 114:74–76
Segal N, Garty BZ, Hoffer V, Levy Y (2012) Effect of instruction on the ability to use a self-administered epinephrine injector. Isr Med Assoc J 14:14–17
Guerlain S, Hugine A, Wang L (2010) A comparison of 4 epinephrine autoinjector delivery: usability and patient preference. Ann Allergy Asthma Immunol 104:172–177
Camargo CA Jr, Guana A, Wang S, Simons FE (2013) Auvi-Q versus EpiPen: preferences of adults, caregivers, and childrens. J Allergy Clin Immunol Pract 1:266–272
Bakirtas A, Arga M, Catal F, Derinoz O, Demirsoy MS, Turktas I (2011) Make-up of the epinephrine autoinjector: the effects on its use by untrained users. Pediatr Allergy Immunol 22:729–733
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
The study was approved by the Ethical Committee of Guglielmo da Saliceto Hospital, Piacenza, Italy.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ridolo, E., Montagni, M., Bonzano, L. et al. How far from correct is the use of adrenaline auto-injectors? A survey in Italian patients. Intern Emerg Med 10, 937–941 (2015). https://doi.org/10.1007/s11739-015-1255-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-015-1255-z