Abstract
Pulmonary Embolism (PE) incidence increases with age. Data on mortality and prognosis in elderly patients with suspected PE are lacking. (1) To assess 30- and 90-day mortality in subjects with PE from an elderly population seen in the emergency department (ED); (2) to test the prognostic accuracy of a simplified Pulmonary Embolism Severity Index (sPESI) coupled to a highly sensitive cardiac Troponin T (hs-cTnT) level. A retrospective cohort study was performed, including patients evaluated in the ED of Vimercate Hospital for clinically suspected PE from 2010 to 2012. Study population: n = 470, 63.4 % women, mean age ± SD 73.06 ± 16.0 years, 40 % aged ≥80 and 77.7 % ≥65 years old, confirmed PE: 22.6 % (106 cases). Within 30 and 90 days, mortality among patients with confirmed PE was 14.2 % (8.8–22.0) and 20.8 % (16.5–41.7). In subjects aged ≥80 years, 30-day mortality was 18.9 % among patients with confirmed PE, and 12.6 % among those with PE excluded (p = 0.317). Ninety-day mortality rates were 29.7 and 19.9 %, respectively (p = 0.193). In patients with confirmed PE, Negative Predictive Value of sPESI was 94.1 % (80.3–99.3) for 30 days and 88.2 % (72.3–96.7) for 90-day mortality. Adding the hs-cTnT level to sPESI did not improve its performance. (1) In an elderly population referring to the ED with clinically suspected PE, mortality was high both in subjects with and without confirmed PE; (2) the ability of sPESI and hs-cTnT to predict PE mortality seems to be lower than reported in studies based on data from younger populations. Better risk stratification tools will be necessary to improve clinical management in this setting.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute pulmonary embolism (PE) is a major health problem, and its short-term mortality varies from less than 1 % to more than 60 % [1, 2]. Population aging is a global phenomenon [3]. The incidence of venous thromboembolism (VTE), particularly PE, increases with age, and the prevalence of major risk factors for VTE may differ according to age [4].
Appropriate risk stratification is essential to set reliable in- and outpatient treatment pathways in subjects with confirmed PE. Systematic reviews in a general population confirm that individuals with acute PE treated as outpatients have low incidences of recurrent VTE and mortality [5, 6]. The introduction of new oral anticoagulants agents may represent a simplification of initial therapy and a favorable condition to manage these subjects as outpatients with potential benefits like cost savings from a decrease in hospitalizations and fewer patients at risk for acquired infections or other in-hospital complications [7, 8].
PE short-term (30 days) mortality has been extensively studied in general populations, and several validated prognostic models to identify low-risk PE patients are available, like the original (GPS) and simplified (sGPS) versions of the Geneva Prognostic Score [9], the Hestia score [10], the original (PESI) and simplified versions of Pulmonary Embolism Severity Index (sPESI) [11, 12]. Moreover, highly sensitive cardiac Troponin T (hs-cTnT) testing has been proposed as a tool for the identification of low-risk PE patients in the general population [13–15].
However, few studies address the issue of mortality and risk stratification scores prognostic performance in elderly subjects with PE [16]. Furthermore, much less is known about prognosis and mortality of patients referred to the ED with suspected PE, in whom PE is excluded.
Patients managed in the ED of our hospital with suspected PE represent an aging population with a high prevalence of elderly (aged ≥65 years old) and very elderly (aged ≥80 years old) subjects, as stated elsewhere [17].
Therefore, the aims of this study were (1) to assess 30- and 90-day mortality in subjects with PE from an elderly population seen in the ED; and (2) to test the prognostic accuracy of sPESI coupled to the hs-cTnT level in this setting.
Materials and methods
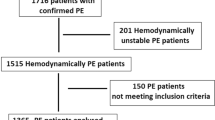
We performed a retrospective cohort study. Patients evaluated in the ED of Vimercate Hospital—a 500 bed general hospital—for clinically suspected PE (index episode) from January 1, 2010 to December 31, 2012 were included. In our hospital, data on D-dimer and quantitative hs-cTnT assay, Wells score and sPESI variables are available for patients with suspected PE. However, as in most cases of real-world clinical practice, the standard practice in the ED considers performing a pulmonary computerized tomography angiography (CTA) scan to exclude PE if suspected, based on an emergency physician’s gestalt approach. Thus, we recalculated a sPESI score retrospectively using recorded data.
All data were obtained through the centralized electronic database of patients’ medical records of our hospital, which contains clinical, laboratory and radiological data. Helical computerized tomography scans were performed on a Brilliance Philips CT scanner (Philips, Cleveland, OH, USA,) which included 64-detector row capability. Levels of hs-cTnT were measured by means of a quantitative electrochemiluminescence immunoassay (Elecsys 2010 analyser, Roche Diagnostics, Mannheim, Germany), analytic range 3–10,000 pg/mL [18]. A level of 14 pg/mL was defined as the threshold between normal and elevated biomarker levels [14].
Pulmonary embolism was ruled out or confirmed on the basis of the absence or presence of a filling defect in one or more pulmonary arteries up to sub-segmental arteries in CTA, as stated at the time of the acquisition of images by certified radiologists belonging to the hospital team. All patients with confirmed PE were admitted to the hospital, and treated with anticoagulant therapy according to the international guidelines [1].
The sPESI score was calculated giving one point for the presence of every of the following parameters: (1) age >80 years; (2) history of cancer; (3) history of chronic cardiac or pulmonary disease (heart failure or chronic lung disease); (4) pulse rate ≥110 beats/minute; (5) systolic blood pressure <100 mm Hg; and (6) arterial oxyhemoglobin saturation <90 % measured at the time of PE diagnosis. Patients were classified into either a low-risk (0 points) or a high-risk (≥1 point[s]) group [12].
Vital status within 30 and 90 days was recorded for all patients. Unique personal identifiers were checked for the follow-up concerning mortality using the regional demographic register updated at January 31, 2014.
Because of the retrospective design, informed consent was not obtained from individual patients, but permission for data analysis and to perform the study was granted by the Institutional Research Ethics Committee, in accord with local and international recommendations and Helsinki declaration.
To determine the accuracy of each score to predict 30- and 90-day overall mortality, a Receiver operating characteristic (ROC) curve was constructed with sPESI score (low vs. high risk,) and sPESI plus hs-cTnT values (positive ≥14 pg/mL.). Sensitivity, Specificity, Positive and Negative Predictive Value were calculated. We assessed the discriminative power of scores to predict 30- and 90-day overall mortality by calculating the area under the curve (AUC).
Statistical analysis was performed using software SPSS version 18.0, (SPSS, Chicago, IL, USA). Student’s t test analysis was performed for continuous variables and Chi square test for differences between categorical variables. p values <0.05 were considered to be significant. Exact 95 % confidence intervals (95 %CI) around the observed incidences were calculated using the exact method and the method based on the approximation to a normal distribution, depending on the case.
Results
Out of the 492 patients evaluated in the ED with suspected PE, 22 cases were excluded for lacking hsTnT test results. The remaining 470 patients constituted the study population (298 women, 63.4 %), mean age ± SD 73.06 ± 16.0 years (median 77, range 16–99), 188 (40.0 %) patients were ≥80 years old, and 365 (77.7 %) ≥65 years old, with an overall prevalence of confirmed PE of 22.6 % (106 cases).
Considering the variables used to calculate sPESI score, patients with confirmed PE had a lower prevalence of chronic cardiopulmonary disease compared to those with excluded PE (6.6 vs. 17.0 %, p = 0.008), and a higher prevalence of arterial oxygen saturation below 90 % (27.4 vs. 17.6 %, p = 0.026) and positive (≥14 pg/mL) hs-cTnT levels (42.5 vs. 35.7 %, p < 0.001), Table 1.
Overall, 45 patients (9.6 %, 95 %CI 7.2–12.6) died within 30 days and 75 (16.0 %, 95 % CI 12.9–19.5) within 90 days. Among patients with PE, overall mortality within 30 and 90 days was 14.2 % (95 % CI 8.8–22.0) and 20.8 % (95 % CI 16.5–41.7), and 30-day mortality was 5.9 % (95 % CI 0.7–19.7) among subjects with low-risk and 18.1 % (95 % CI 9.2–26.9) in those with high-risk sPESI (p = 0.093). Outcomes within 30 and 90 days for low- and high-risk sPESI score patients with PE are shown in Table 2.
In subjects aged ≥80 years, 30-day mortality was 18.9 % (95 % CI 7.9–35.2) among patients with confirmed PE and 12.6 % (95 %CI 7.3–17.9) among those with PE excluded (p = 0.317). Within 90 days mortality rates were 29.7 % (95 % CI 15.9–46.9) and 19.9 % (95 % CI 13.5–26.2), respectively, with p = 0.193.
In patients with PE, negative predictive value of sPESI score was 94.1 % (95 %CI 80.3–99.3) for mortality within 30 days and 88.2 % (95 % CI 72.3–96.7) for mortality within 90 days. Adding hs-cTnT levels to the sPESI score did not increase the performance of the test, Table 3.
For predicting mortality within 30 days in patients with PE, the ROC curve showed an AUC of 0.64 (95 % CI 0.51–0.76) for sPESI and 0.65 (95 % CI 0.52–0.77) adding hs-cTnT to sPESI. Figure 1 shows ROC plot of sPESI and sPESI plus hs-cTnT to predict mortality within 30 and 90 days in this population.
ROC plot of sPESI and sPESI plus hs-cTnT to predict mortality within 30 and 90 days in patients with PE. Area under the curve (AUC) sPESI, 30-day mortality = 0.64 (95 % CI 0.51–0.76). AUC sPESI and hs-cTnT, 30-day mortality = 0.65 (95 % CI 0.52–0.77). AUC sPESI, 90-day mortality = 0.60 (95 % CI 0.47–0.73). AUC sPESI and hs-cTnT, 90-day mortality = 0.63 (95 % CI 0.50–0.75). PE Pulmonary Embolism, sPESI simplified Pulmonary Embolism Severity Index, hs-cTnT highly sensitive cardiac Troponin T
Discussion
Even though population aging is a growing phenomenon and the incidence of PE increases with age, data on prognosis and mortality of elderly patients seen in the ED with suspected PE are lacking.
In our study, we found high 30- and 90-day mortality rates among patients from an elderly population referring to the ED, with confirmed and excluded PE, and some points should be highlighted.
First, 30-day mortality of patients as a whole is three times higher in those with high than in those with low sPESI. This figure is consistent with available data. On the other hand, in patients ≥80 years old, the difference in 30-day mortality between those with confirmed PE and those with PE suspected but excluded is not significant. In subjects with confirmed acute PE, we find a mortality of 14.2 and 20.8 % within 30 and 90 days, respectively, higher than the mortality reported in studies based on younger subjects. Within 30 days, the mortality rate in the sPESI score derivation cohort was 7.8 % [12]. Since in the sPESI score internal and external derivation cohort the follow-up was set at 30 days, only 30-day results may be compared. In the study by Zwierzina et al. [16], one of the very few available studies on risk stratification scores prognostic performance in elderly patients with a PE where short-term mortality predictive ability of GPS, PESI and sPESI were assessed; 30 day mortality was 3.8 %. Subjects included in this study were 449 out of 813 of those initially identified by having an objectively confirmed PE, with a minor representation of patients older than 80 years (29.6 %). In our study, 40 % of the subjects were aged 80 years or more, and almost 80 % (77.7) ≥65 years old, defining ours as an elderly and very elderly real-world population [17]. In the RIETE registry, one-third of PE patients aged above 90 years die during the first few months of therapy [19], confirming our finding of a higher mortality in very elderly subjects.
Second, and interestingly, we find markedly high mortality rates within 30 and 90 days even in the subjects in whom PE was excluded. The fact that these patients remain exposed to life-threatening diseases even after excluding PE may be an important point for emergency physicians who, in everyday clinical practice, must decide whether to hospitalize or discharge them.
Third, the accuracy of sPESI to predict short- and medium-term mortality in elderly and very elderly patients with PE seems to be lower than reported in studies performed in younger populations. Studies on risk stratification in PE patients like sGPS, Hestia, PESI, and sPESI [9–12] are mainly based on data from a general population, with aging people poorly represented. In a randomized clinical trial aimed to compare the effectiveness and safety of outpatient versus inpatient care for low-risk patients with acute, symptomatic PE, mean ages are as low as 47 and 49 years in the out-and inpatient management groups, respectively [20].
Finally, adding cardiac troponin testing by using hs-cTnT levels does not improve sPESI ability to predict mortality in elderly patients. Several studies confirm that elevated troponin levels identify patients with PE at high risk of short-time death, [15] and the prognostic efficacy of a combination of indexes employing sPESI plus cardiac Troponin T, but with very older patients under-represented [21]. Actually, the same approach has not proved to be effective in our very elderly population. In the aforementioned study, the percentage of patients aged over 80 years does not exceed 20 %, and the reported mortality rates are significantly lower than those we observed [21]. Thus, our finding of high mortality rates in subjects aged 80 years or more with and without PE confirms this as a different clinical setting, raising questions on the applicability in older patients of risk stratification tools developed on the basis of data of younger populations.
The main limitation of our study is the small sample size. We attempted to avoid possible selection bias by including all consecutive patients evaluated in the ED for clinically suspected PE. Moreover, none of the included patients were lost to follow-up. Thus, despite its small size, our study population would reproduce a real-world representative sample of an elderly and very elderly patients setting. However, since confidence intervals are wide as a consequence of the small sample size, our results need to be confirmed in larger cohorts. Other limitations are that, since it is a retrospective study, no definite conclusions can be drawn on the high mortality rates among high- and low-risk patients, and that specific causes of death were not retrievable.
We conclude that in an elderly population seen in the ED with a clinically suspected PE, mortality is high in patients with and without a confirmed PE. The ability of sPESI to predict mortality is lower than reported in studies based on data from younger populations, and adding cardiac troponin testing does not improve it. Even though our results should be confirmed by prospective, larger cohorts, they suggest that better risk stratification tools will be necessary to improve clinical management of elderly and very elderly patients with suspected PE.
References
Kearon C, Akl EA, Comerota AJ, Prandoni P, Bounameaux H, Goldhaber SZ, Nelson ME, Wells PS, Gould MK, Dentali F, Crowther M, Kahn SR (2012) American College of Chest Physicians. Antithrombotic therapy for VTE disease: antithrombotic therapy and prevention of thrombosis, 9th ed.: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141(2 Suppl):e419S–e494S
Becattini C, Agnelli G (2007) Acute pulmonary embolism: risk stratification in the emergency department. Intern Emerg Med 2(2):119–129
Stein PD, Hull RD, Kayali F, Ghali WA, Alshab AK, Olson RE (2004) Venous thromboembolism according to age. The impact of an aging population. Arch Intern Med 164:2260–2265
Ageno W, Agnelli G, Imberti D, Moia M, Palareti G, Pistelli R, Verso M (2013) Prevalence of risk factors for venous thromboembolism in the Italian population: results of a cross-sectional study from the Master Registry. Intern Emerg Med 8(7):575–580. doi:10.1007/s11739-011-0644-1
Piran S, Le Gal G, Wells PS, Gandara E, Righini M, Rodger MA, Carrier M (2013) Outpatient treatment of symptomatic pulmonary embolism: a systematic review and meta-analysis. Thromb Res 132:515–519
Squizzato A, Galli M, Dentali F, Ageno W (2009) Outpatient treatment and early discharge of symptomatic pulmonary embolism: a systematic review. Eur Respir J 33:1148–1155
Aujesky D, Stone RA, Kim S, Crick EJ, Fine MJ (2008) Length of hospital stay and post discharge mortality in patients with pulmonary embolism: a statewide perspective. Arch Intern Med 168:706–712
Park B, Messina L, Dargon P, Huang W, Ciocca R, Anderson FA (2009) Recent trends in clinical outcomes and resource utilization for pulmonary embolism in the United States: findings from the nationwide inpatient sample. Chest 136:983–990
Klok FA, Mos IC, Nijkeuter M, Righini M, Perrier A, Le Gal G, Huisman MV (2008) Simplification of the revised Geneva score for assessing clinical probability of pulmonary embolism. Arch Intern Med 168:2131–2136
Zondag W, Mos IC, Creemers-Schild D, Hoogerbrugge AD, Dekkers OM, Dolsma J, Eijsvogel M, Faber LM, Hofstee HM, Hovens MM, Jonkers GJ, Van Kralingen KW, Kruip MJ, Vlasveld T, de Vreede MJ, Huisman MV (2011) Hestia Study Investigators. Outpatient treatment in patients with acute pulmonary embolism: the Hestia Study. J Thromb Haemost 9:1500–1507
Aujesky D, Obrosky DS, Stone RA, Auble TE, Perrier A, Cornuz J, Roy PM, Fine MJ (2005) Derivation and validation of a prognostic model for pulmonary embolism. Am J Resp Crit Care Med 172:1041–1046
Jimenez D, Aujesky D, Moores L, Gomez V, Lobo JL, Uresandi F, Otero R, Monreal M, Muriel A, Yusen RD (2010) RIETE Investigators. Simplification of the pulmonary embolism severity index for prognostication in patients with acute symptomatic pulmonary embolism. Arch Intern Med 170:1383–1389
Lindner G, Pfortmueller CA, Braun CT, Exadaktylos AK (2014) Non-acute myocardial infarction-related causes of elevated high-sensitive troponin T in the emergency room: a cross-sectional analysis. Intern Emerg Med 9(3):335–339. doi:10.1007/s11739-013-1030-y
Lankeit M, Friesen D, Aschoff J, Dellas C, Hasenfuss G, Katus H, Konstantinides S, Giannitsis E (2010) Highly sensitive troponin T assay in normotensive patients with acute pulmonary embolism. Eur Heart J 31:1836–1844
Becattini C, Vedovati MC, Agnelli G (2007) Prognostic value of troponins in acute pulmonary embolism: a meta-analysis. Circulation 116:427–433
Zwierzina D, Limacher A, Méan M, Righini M, Jaeger K, Beer HJ, Frauchiger B, Osterwalder J, Kucher N, Matter CM, Banyai M, Angelillo-Scherrer A, Lämmle B, Egloff M, Aschwanden M, Mazzolai L, Hugli O, Husmann M, Bounameaux H, Cornuz J, Rodondi N, Aujesky D (2012) Prospective comparison of clinical prognostic scores in elder patients with a pulmonary embolism. J Thromb Haemost 10:2270–2276
Polo Friz H, Pasciuti L, Meloni DF, Crippa M, Villa G, Molteni M, Primitz L, Del Sorbo D, Delgrossi G, Cimminiello C (2014) A higher d-dimer threshold safely rules-out pulmonary embolism in very elderly emergency department patients. Thromb Res. 2014(133):380–383
Giannitsis E, Kurz K, Hallermayer K, Jarausch J, Jaffe AS, Katus HA (2010) Analytical validation of a high-sensitivity cardiac troponin T assay. Clin Chem 56:254–261
Vasco B, Villalba JC, Lopez-Jimenez L, Falga C, Montes J, Trujillo-Santos J, Monreal M (2009) RIETE Investigators. Venous thromboembolism in nonagenarians. Findings from the RIETE registry. Thromb Haemost 101:1112–1118
Aujesky D, Roy PM, Verschuren F, Righini M, Osterwalder J, Egloff M, Renaud B, Verhamme P, Stone RA, Legall C, Sanchez O, Pugh NA, NGako A, Cornuz J, Hugli O, Beer HJ, Perrier A, Fine MJ, Yealy DM (2011) Outpatient versus inpatient treatment for patients with acute pulmonary embolism: an international, open-label, randomised, non-inferiority trial. Lancet 378:41–48
Lankeit M, Jiménez D, Kostrubiec M, Dellas C, Hasenfuss G, Pruszczyk P, Konstantinides S (2011) Predictive value of the high-sensitivity troponin T assay and the simplified Pulmonary Embolism Severity Index in hemodynamically stable patients with acute pulmonary embolism: a prospective validation study. Circulation 124:2716–2724
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Polo Friz, H., Molteni, M., Del Sorbo, D. et al. Mortality at 30 and 90 days in elderly patients with pulmonary embolism: a retrospective cohort study. Intern Emerg Med 10, 431–436 (2015). https://doi.org/10.1007/s11739-014-1179-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-014-1179-z