Abstract
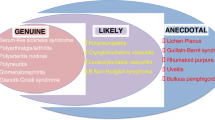
Hepatitis C Virus (HCV) is a major health problem, infecting about 3 % of people worldwide and leading to liver as well as extrahepatic diseases. This justifies the definition of HCV infection as a systemic disease. Based on available data, the link between the virus and some of these extrahepatic disorders is certain, whereas for some others needs further confirmation. HCV-related lymphoproliferative disorders, ranging from benign, but pre-lymphomatous conditions, like mixed cryoglobulinemia, to frank lymphomas, represent the extrahepatic manifestations most closely related to HCV. The primary involvement of the liver and lymphatic system corresponds to the double viral tropism, being HCV able to infect both hepatic and lymphatic cells. Other HCV-associated disorders include renal, endocrine, dermatological, cardiovascular, rheumatologic and central nervous system diseases. On the whole, the HCV disease appears a very important, mainly hidden, public health problem leading to heavy direct and indirect costs. The possibility that HCV may be eradicated following antiviral therapy is important for both the therapeutic and preventive points of view, making the HCV disease an ideal model for pathogenetic studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatitis C virus (HCV) infection is a global health problem, affecting approximately 170 million people worldwide, and causing chronic hepatitis, liver cirrhosis and hepatocellular carcinoma with liver-related mortality in about 350,000 people/year. However, these data are underestimated do not taking into account the extrahepatic aspects that make the infection a systemic disease. Early after its discovery, it was shown that HCV is not only hepatotropic but also lymphotropic [1–3]. It was also shown that several extrahepatic manifestations (EHMs-HCV) can complicate HCV infection [4–6] including, first, lymphoproliferative and/or autoimmune disorders [7]. The present review will focus on the principal data available about the non-strictly hepatic manifestations of HCV, justifying the systemic nature of the consequences of such a chronic infection.
HCV and lymphoproliferative disorders
Mixed cryoglobulinemia
Mixed cryoglobulinemia (MC) is the most frequent, best known and strictly HCV-associated EHMs-HCV (>90 % MC HCV+ in some studies) [7–9]. MC may be defined a both autoimmune and B-lymphoproliferative disorder (LPD) that may evolve to a frank malignancy in about 8–10 % of cases [6, 10–14]. The definition refers to the presence of serum Igs that reversibly precipitate at low temperatures (<37 °C) (cryoglobulins, CGs) and are represented by circulating immune complex (CIC) typically consisting of an IgM RF (mono-oligoclonal in type II MC, or polyclonal in type III MC) and polyclonal Igs (most frequently IgGs) including anti-HCV antibodies [11]. MC has been generally reported, at least subclinically, in the majority of HCV patients, even if data may widely vary in different geographical areas (from <20 to >50 %) [4, 6, 15–17]. Only a minority of MC patients (5 to >30 %) shows a symptomatic MC or MC syndrome (MCS) (usually women aged more than 50 years), but even asymptomatic patients might develop MCS in the future [12]. The clinical manifestations of MCS are secondary to a systemic vasculitis characterized by the deposition of CGs in the vessels and can be classified as one of the CIC-mediated systemic vasculitis involving small-sized vessels. First described by Meltzer and Franklin [18] as a triad of purpura, fatigue and arthralgia, the various involvement of different organs and tissues (mainly skin, joints, renal, peripheral nerves) leads to variable clinical presentation and evolution [12, 19]. Palpable purpura (leukocytoclastic vasculitis) and petechiae most often affects the legs. Papules, ulcers, and livedo can also occur and can affect any skin site. A sicca syndrome, to be differentiated from the primary Sjogren syndrome (SS), occurs in MC and also in HCV patients without MC [20]. In the worst cases, a severe involvement of the kidney (see also below) and the peripheral and central nervous system is observed [6]. The peripheral neuropathy including mixed neuropathies (prevalently sensitive, axonal) is common in MC (80–90 % of cases), and also in HCV without MC [21]. Several studies, including personal observations, showed an association between MCS and severe liver damage. However, discordant data exist [22]. Circulating CGs, RF, and a low C4 represents the serum hallmarks of MC. In a large study, a significantly lower cumulative 10th-year survival, calculated from time of diagnosis, was scored in MCS patients versus the control population [12]. Various attempts at defining a clinical classification have been made since the 1990s and recently, preliminary classification criteria were developed according to the results of an international, European study [20], and then validated [23].
Concerning the therapeutic approach of MCS, the individuation of the viral etiology justified the use of antiviral drugs in addition to the classic symptomatic/pathogenetic therapies. Starting from the first pioneer studies [24, 25], the antiviral approach evolved following the modifications of anti-HCV therapy and, at present, the combination of pegylated IFN (Peg-IFN) plus ribavirin has been suggested as standard of care (SoC) for mild to moderate MCS [6, 26–28]. Evidence for the strong correlation between a complete viral eradication and resolution or consistent improvement of MCS has been produced and a role played by occult viral persistence in lymphatic cells shown [29, 30]. The effects of viral eradication in HCV-related LPDs confirm the etiopathogenetic role played by HCV. A regression of B-cell pathogenetic clones after viral eradication and new expansion in case of virological relapse was shown [31, 32]. For these reasons, the goal of therapy in HCV MCS should be to eradicate the virus. However, a cautious attitude could be suggested in consideration of the side effects possibly induced by IFN in a MC background (i.e., possible worsening of neuropathy, anemia). The introduction of new, more effective, direct anti-HCV drugs is of high interest, as also suggested by preliminary personal observations. For patients with severe vasculitis, including cases of renal insufficiency or intestinal ischemia, control of disease with potent immunosuppressive regimens (i.e., anti-CD20 Rituximab, RTX), with or without plasmapheresis, is usually required. The use of RTX in MCS was shown to be safe and useful in improving main manifestations, especially cutaneous [33–38]. Its use was initially limited to patients without advanced liver disease due to the risk of a hepatitis flare. However, in a study involving patients with MCS and severe liver disease, RTX was not only useful but also safe. Surprisingly, a consistent improvement of the cirrhosis syndrome was observed in some decompensated patients [35]. An IFN-based etiologic treatment in combination with RTX was also suggested to be suitable and effective in HCV MCS patients [39, 40].
Lymphoma and monoclonal gammopathies
The very close association between MC and HCV infection leads to the hypothesis that HCV may be involved in the pathogenesis of lymphoma as well [4, 7, 9]. A significant association between HCV and B-cell non-Hodgkin’s lymphoma (NHL) was initially reported in Italian subjects [41, 42] and confirmed in the large majority of studies [43, 44]. Some discordant data from northern countries [6] suggested the contribution of genetic factors. This association involves different histopathological types of B-cell NHL, the most strictly associated being the lymphoplasmacytic, marginal zone and diffuse large B-cell lymphoma [44]. A serum monoclonal gammopathy (MG), more frequently type IgMk and diagnosed as MG of uncertain significance (MGUS), was frequently observed in HCV patients, in most cases associated with a 2a/c genotype [45]. Clinical remission following effective antiviral therapy was especially observed in low-grade B-cell NHL and, in particular, in splenic marginal zone lymphoma (SMZL) [46]. Furthermore, the preventive value of viral eradication against the lymphomagenetic evolution of HCV infection was observed in some studies [47]. Consequently, the inclusion of antiviral therapy, alone or in combination with RTX, seems to be rational in the therapy of low-grade HCV-positive NHL [31, 46, 48]. In intermediate to high grade NHL, anti-HCV therapy may be helpful in prolonging the disease-free period [49]. Results of further, sufficiently large and controlled trials, will be precious in order to better standardize the therapeutic approach.
Pathogenesis of HCV-related LPDs
Available data suggest that HCV-related LPDs are the result of multiple and cooperating mechanisms and events belonging to three principal categories: an important and sustained activation of the B-cell compartment; an inhibition of B-cell apoptosis; genetic/epigenetic and environmental factors (Fig. 1).
Hypothetical pathogenetic cascade explaining the development of lymphoproliferative disorders (LPDs) during HCV chronic infection. HCV-related LPDs seem to be the result of multiple and cooperating mechanisms and events. Available data suggest that these latter belong to three principal categories: (1) an important and sustained activation of the B-cell compartment, possibly explained by several factors including the antigenic stimulation consequent to the chronic infection of liver/B cells, the E2-CD81 binding, a direct action of some HCV proteins, some cytokines (BAFF); (2) a prolonged B-cell survival/inhibition of B-cell apoptosis induced by t(14;18) translocation and other factors (possibly including different genetic aberrations and cytokines), (3) on a background of predisposing genetic-epigenetic and/or environmental factors conditioning the LPD clinical manifestation. The occurrence of additional genetic aberrations, favored by the abnormal B-cell survival, would lead to the frank malignancy. Refer to the text for a more detailed description
A sustained antigenic stimulation due to the chronic HCV infection was shown to play an important predisposing role. Intrahepatic lymphatic follicle-like nodules are a peculiarity of HCV infection and sites of clonal B-cell expansion [11]. Isolated B cells have been shown to produce the WA cross-idiotype, a RF typical of MC [50]. Deeper analysis of BCR sequence and affinity showed a homology with anti-HCV protein. A more specific role of some viral antigens (NS3 and E2) in inducing HCV-related LPDs was proposed [51]. Interestingly, the HCV E2 protein was shown to be able to bind to the CD81 expressed on B cells leading to a lower B-cell activation threshold [52]. In addition, Igs isolated from a HCV NHL were able to bind E2 protein and a sequence homology was found between HCV E2 and IgG variable domains [53, 54]. The role played by the viral lymphotropism in the pathogenesis of HCV-related LPDs was initially suggested by the observation of significantly higher prevalence of PBMC or bone marrow cell infection in HCV+ patients with than without MCS [1, 55]; such observations were also confirmed by studies on in vivo and in vitro animal models [56, 57]. Interestingly, in an in vitro model, HCV-infected cells showed an increased rate of mutations of oncogenes and Ig genes, probably by the induction of an error prone DNA polymerase and the activation-induced cytidine deaminase (AID) [58]. This hypothesis was supported by the detection of abnormal levels of AID in B cells of HCV patients [59]. Concerning a possible direct role of viral proteins, the major interest was addressed to the effects of HCV core protein. Interestingly, in different transgenic models, the expression of HCV core was correlated with the development of lymphoma [60, 61]. Finally, an altered expression of some isoforms of the p53 family genes, the DNp63 and DNp73, previously described to be overexpressed in human cancers including lymphoma, was found in both B-cell lines expressing the HCV core protein and in primary B cells from patients with LPDs [62]. In the HCV-related lymphomagenetic process, an important step, possibly inducing “points of no-return”, is the occurring of chromosomal aberrations. In this context, the (14;18) translocation, causing the enhanced transcription of Bcl-2 protein and abnormal survival of B cells, was deeply described as strictly associated to type II HCV MC [10, 31, 63]. In addition, the regression of t(14;18)-positive B-cell clones after antiviral therapy with a new expansion of the translocated clones in patients who virologically relapsed was shown [29–32]. Furthermore, alterations of the ploidy grade, with a similar rate to the one characterizing the NHL, were recently described in HCV patients [64]. Several reports suggested the role of particular cytokines and chemokines, even if a profile typical for HCV LPDs is still not fully defined. These include IFNγ, TNFα, MIP-1α, MIP-1β, CXCL-10, CXCR-3, CXCL13 (BCA-1 or BLC), CXCL-11, IL-1α and osteopontin (OPN) [65–68]. A particular attention was focused on the role of B-cell activating factor, Baff or BLyS. In HCV patients, increased Baff serum levels have been found, especially in subjects with LPDs [69]. A particular genetic variant (−871 T) of Baff promoter was found with higher frequency in HCV patients with than without MC, strongly suggesting a key role of genetic factors in Baff overexpression [70, 71]. Finally, as already shown for other diseases, the role of microRNAs is possibly critical in the pathogenesis of HCV-related LPDs representing a field of interest, even if only a few data are nowadays available [72].
Renal pathology
Several renal manifestations have been associated with HCV infection, the most common being membranoproliferative glomerulonephritis (MPGN) [73–75]. HCV-associated membranous or proliferative glomerulonephritis or focal segmental glomerulosclerosis have been also described [22, 74].The strongest association was reported for cryoglobulinaemic MPGN (MC-MPGN) [6, 73, 74]. The presence of a renal involvement is one of the worst prognostic indices in the natural history of MCS [12] and in the etiologic treatment [76] even if its course can be variable. The urine analysis and creatinine determination should be suggested in HCV patients.
Endocrine pathology
The prevalence of thyroid disorders is generally high in HCV-positive patients [77] and most frequently represented by antithyroid peroxidase antibodies in female subjects [77]. Hypothyroidism has been frequently observed, especially in HCV MC [78], and an association with papillary thyroid carcinoma was also shown [79, 80]. The possibility that IFN treatment may unmask autoimmune thyroid disease must be also taken into account [81]. Overall, a careful monitoring of the thyroid in HCV patients should be suggested.
Interesting and still incompletely understood data exist about the relationship between HCV (especially type 3) infection and glucose metabolism. Several studies showed that HCV could lead to the development of type 2 diabetes mellitus, possibly as a result of HCV-induced metabolic disturbances [82]. However, discordant data exist [83] and the argument is still object of debate. Insulin resistance was observed in 30–70 % of HCV patients [84], improved after viral eradication [85] and was interpreted as the effect of several factors including proinflammatory cytokines/adipokines, advanced liver disease or HCV-related steatosis. Careful monitoring of glycaemia in patients with HCV infection is recommended.
Dermatological manifestations
Several dermatological manifestations have been associated with HCV infection including, first, the cryoglobulinemic vasculitis (see before), porphyria cutanea tarda (PCT) and lichen planus (LP). Others, including pyoderma gangrenosum, erythema nodosum, and urticaria, have been described in only anecdotal observations and need confirmation. The association between PCT and LP and HCV infection appeared strict in several studies mainly performed in southern Europe and Japan [4, 86–88]. However, it was suggested that the infection plays an indirect role, probably acting as a triggering factor in subjects predisposed due to genetic factors and/or liver disorders (hepatic iron overload, liver cirrhosis) [5, 87].
Cardiovascular manifestations
Recent studies suggest that HCV is involved in the development of dilated cardiomyopathy, hypertrophic cardiomyopathy and arrhythmogenic right ventricular cardiomyopathy in addition to myocarditis. These associations are still object of debate [6].
The influence of HCV infection on aortic atherosclerosis risk was mostly evident in case of active viral replication and in some geographic areas [89, 90]. In an Italian study, HCV RNA sequences, including HCV replication intermediates, were found in the plaque tissue isolated from anti-HCV patients, including serum HCV RNA-negative subjects [89], suggesting a direct local action of the virus [89]. More recently, other studies performed on HCV mono-infected or HCV–HIV co-infected patients confirmed the link between carotid atherosclerosis and HCV chronic infection [91–93].
Rheumatologic disorders
Polyarthralgia is the most common rheumatologic symptom described in HCV-infected patients [5, 78]. HCV arthritis could be part of the MCS or be independent [94]. HCV-associated oligoarticular or polyarticular non-erosive arthritis can clinically mimic rheumatoid arthritis, although anti-cyclic citrullinated peptide (anti-CCP) antibodies and erosive joint changes are generally absent.
Central nervous system (CNS) abnormalities
Mild neurocognitive impairment, depression, anxiety and other psychiatric disorders have been frequently reported in HCV infection [95, 96]. An alteration of the neuro-endocrine-immune system response has been observed and could play a key role [96]. Serum tryptophan (TRP) and kynurenine levels were lower in HCV patients than in controls [97], but returned toward physiological levels after viral eradication and psychopathology improved, thus suggesting a direct viral role [98]. Overall, the CNS abnormalities observed during HCV infection greatly cooperate in the impairment of the quality of life of HCV patients with corresponding important direct and indirect costs [96].
In conclusion, HCV infection induces a systemic, complex disease whose varying manifestations deserve to be correctly recognized and managed. The possibility that HCV may be eradicated following effective antiviral therapy is important for both the therapeutic, preventive and pathogenetic points of view.
References
Zignego AL, Macchia D, Monti M et al (1992) Infection of peripheral mononuclear blood cells by hepatitis C virus. J Hepatol 15:382–386
Zignego AL, De Carli M, Monti M et al (1995) Hepatitis C virus infection of mononuclear cells from peripheral blood and liver infiltrates in chronically infected patients. J Med Virol 47:58–64
Zignego AL, Giannini C, Monti M, Gragnani L (2007) Hepatitis C virus lymphotropism: lessons from a decade of studies. Dig Liver Dis 39(Suppl 1):S38–S45
Zignego AL, Brechot C (1999) Extrahepatic manifestations of HCV infection: facts and controversies. J Hepatol 31:369–376
Cacoub P, Renou C, Rosenthal E et al (2000) Extrahepatic manifestations associated with hepatitis C virus infection. A prospective multicenter study of 321 patients. The GERMIVIC. Groupe d’Etude et de Recherche en Medecine Interne et Maladies Infectieuses sur le Virus de l’Hepatite C. Medicine (Baltimore) 79:47–56
Zignego AL, Ferri C, Pileri SA, Caini P, Bianchi FB (2007) Extrahepatic manifestations of Hepatitis C Virus infection: a general overview and guidelines for a clinical approach. Dig Liver Dis 39:2–17
Zignego AL, Ferri C, Giannini C et al (1997) Hepatitis C virus infection in mixed cryoglobulinemia and B-cell non-Hodgkin’s lymphoma: evidence for a pathogenetic role. Arch Virol 142:545–555
Misiani R, Bellavita P, Fenili D et al (1992) Hepatitis C virus infection in patients with essential mixed cryoglobulinemia. Ann Intern Med 117:573–577
Ferri C, Monti M, La Civita L et al (1993) Infection of peripheral blood mononuclear cells by hepatitis C virus in mixed cryoglobulinemia. Blood 82:3701–3704
Zignego AL, Giannelli F, Marrocchi ME et al (1997) Frequency of bcl-2 rearrangement in patients with mixed cryoglobulinemia and HCV-positive liver diseases. Clin Exp Rheumatol 15:711–712
Sansonno D, De Vita S, Iacobelli AR et al (1998) Clonal analysis of intrahepatic B cells from HCV-infected patients with and without mixed cryoglobulinemia. J Immunol 160:3594–3601
Ferri C, Sebastiani M, Giuggioli D et al (2004) Mixed cryoglobulinemia: demographic, clinical, and serologic features and survival in 231 patients. Semin Arthritis Rheum 33:355–374
Vallat L, Benhamou Y, Gutierrez M et al (2004) Clonal B cell populations in the blood and liver of patients with chronic hepatitis C virus infection. Arthritis Rheum 50:3668–3678
Craxi A, Laffi G, Zignego AL (2008) Hepatitis C virus (HCV) infection: a systemic disease. Mol Aspects Med 29:85–95
Lunel F, Musset L, Cacoub P et al (1994) Cryoglobulinemia in chronic liver diseases: role of hepatitis C virus and liver damage. Gastroenterology 106:1291–1300
Verbaan H, Carlson J, Eriksson S et al (1999) Extrahepatic manifestations of chronic hepatitis C infection and the interrelationship between primary Sjogren’s syndrome and hepatitis C in Swedish patients. J Intern Med 245:127–132
Zignego AL, Ferri C, Giannini C et al (1996) Hepatitis C virus genotype analysis in patients with type II mixed cryoglobulinemia. Ann Intern Med 124:31–34
Meltzer M, Franklin EC, Elias K, McCluskey RT, Cooper N (1966) Cryoglobulinemia—a clinical and laboratory study. II. Cryoglobulins with rheumatoid factor activity. Am J Med 40:837–856
Cacoub P, Lidove O, Maisonobe T et al (2002) Interferon-alpha and ribavirin treatment in patients with hepatitis C virus-related systemic vasculitis. Arthritis Rheum 46:3317–3326
De Vita S, Quartuccio L, Salvin S et al (2012) Cryoglobulinaemia related to Sjogren’s syndrome or HCV infection: differences based on the pattern of bone marrow involvement, lymphoma evolution and laboratory tests after parotidectomy. Rheumatology (Oxford) 51:627–633
Tembl JI, Ferrer JM, Sevilla MT et al (1999) Neurologic complications associated with hepatitis C virus infection. Neurology 53:861–864
Zignego AL, Giannini C, Ferri C (2007) Hepatitis C virus-related lymphoproliferative disorders: an overview. World J Gastroenterol 13:2467–2478
Quartuccio L, Isola M, Corazza L et al (2012) Performance of the preliminary classification criteria for cryoglobulinemic vasculitis and clinical manifestations in hepatitis C virus-unrelated cryoglobulinemic vasculitis. Clin Exp Rheumatol 30 (1 Suppl 70):48–52
Ferri C, Marzo E, Longombardo G et al (1993) Interferon-alpha in mixed cryoglobulinemia patients: a randomized, crossover-controlled trial. Blood 81:1132–1136
Marcellin P, Descamps V, Martinot-Peignoux M et al (1993) Cryoglobulinemia with vasculitis associated with hepatitis C virus infection. Gastroenterology 104:272–277
De Vita S, Soldano F, Isola M et al (2011) Preliminary classification criteria for the cryoglobulinaemic vasculitis. Ann Rheum Dis 70:1183–1190
Mazzaro C, Monti G, Saccardo F et al (2011) Efficacy and safety of peginterferon alfa-2b plus ribavirin for HCV-positive mixed cryoglobulinemia: a multicentre open-label study. Clin Exp Rheumatol 29:933–941
Adinolfi LE, Utili R, Zampino R et al (1997) Effects of long-term course of alpha-interferon in patients with chronic hepatitis C associated to mixed cryoglobulinaemia. Eur J Gastroenterol Hepatol 9:1067–1072
Giannini C, Giannelli F, Zignego A (2006) Association between mixed cryoglobulinemia, translocation (14;18), and persistence of occult HCV lymphoid infection after treatment. Hepatology 43:1166–1167
Giannini C, Petrarca A, Monti M et al (2008) Association between persistent lymphatic infection by hepatitis C virus after antiviral treatment and mixed cryoglobulinemia. Blood 111:2943–2945
Zignego AL, Ferri C, Giannelli F et al (2002) Prevalence of bcl-2 rearrangement in patients with hepatitis C virus-related mixed cryoglobulinemia with or without B-cell lymphomas. Ann Intern Med 137:571–580
Giannelli F, Moscarella S, Giannini C et al (2003) Effect of antiviral treatment in patients with chronic HCV infection and t(14;18) translocation. Blood 102:1196–1201
Zaja F, De Vita S, Mazzaro C et al (2003) Efficacy and safety of rituximab in type II mixed cryoglobulinemia. Blood 101:3827–3834
Visentini M, Ludovisi S, Petrarca A et al (2011) A phase II, single-arm multicenter study of low-dose rituximab for refractory mixed cryoglobulinemia secondary to hepatitis C virus infection. Autoimmun Rev 10:714–719
Petrarca A, Rigacci L, Caini P et al (2010) Safety and efficacy of rituximab in patients with hepatitis C virus-related mixed cryoglobulinemia and severe liver disease. Blood 116:335–342
Quartuccio L, Petrarca A, Mansutti E et al (2010) Efficacy of rituximab in severe and mild abdominal vasculitis in the course of mixed cryoglobulinemia. Clin Exp Rheumatol 28:84–87
Ferri C, Cacoub P, Mazzaro C et al (2011) Treatment with rituximab in patients with mixed cryoglobulinemia syndrome: results of multicenter cohort study and review of the literature. Autoimmun Rev
De Vita S, Quartuccio L, Isola M et al (2012) A randomized controlled trial of rituximab for the treatment of severe cryoglobulinemic vasculitis. Arthritis Rheum 64:843–853
Dammacco F, Tucci FA, Lauletta G et al (2010) Pegylated interferon-alpha, ribavirin, and rituximab combined therapy of hepatitis C virus-related mixed cryoglobulinemia: a long-term study. Blood 116:343–353
Pietrogrande M, De Vita S, Zignego AL et al (2011) Recommendations for the management of mixed cryoglobulinemia syndrome in hepatitis C virus-infected patients. Autoimmun Rev 10:444–454
Ferri C, La Civita L, Caracciolo F, Zignego AL (1994) Non-Hodgkin’s lymphoma: possible role of hepatitis C virus [letter]. JAMA 272:355–356
Ferri C, Caracciolo F, Zignego AL et al (1994) Hepatitis C virus infection in patients with non-Hodgkin’s lymphoma. Br J Haematol 88:392–394
Zuckerman E, Zuckerman T, Levine AM et al (1997) Hepatitis C virus infection in patients with B-cell non-Hodgkin lymphoma. Ann Intern Med 127:423–428
de Sanjose S, Benavente Y, Vajdic CM et al (2008) Hepatitis C and non-Hodgkin lymphoma among 4784 cases and 6269 controls from the International Lymphoma Epidemiology Consortium. Clin Gastroenterol Hepatol 6:451–458
Andreone P, Zignego AL, Cursaro C et al (1998) Prevalence of monoclonal gammopathies in patients with hepatitis C virus infection. Ann Intern Med 129:294–298
Hermine O, Lefrere F, Bronowicki JP et al (2002) Regression of splenic lymphoma with villous lymphocytes after treatment of hepatitis C virus infection. N Engl J Med 347:89–94
Kawamura Y, Ikeda K, Arase Y et al (2007) Viral elimination reduces incidence of malignant lymphoma in patients with hepatitis C. Am J Med 120:1034–1041
Vallisa D, Bernuzzi P, Arcaini L et al (2005) Role of anti-hepatitis C virus (HCV) treatment in HCV-related, low-grade, B-cell, non-Hodgkin’s lymphoma: a multicenter Italian experience. J Clin Oncol 23:468–473
La Mura V, De Renzo A, Perna F et al (2008) Antiviral therapy after complete response to chemotherapy could be efficacious in HCV-positive non-Hodgkin’s lymphoma. J Hepatol 49:557–563
Sansonno D, Lauletta G, De Re V et al (2004) Intrahepatic B cell clonal expansions and extrahepatic manifestations of chronic HCV infection. Eur J Immunol 34:126–136
De Re V, Sansonno D, Simula MP et al (2006) HCV-NS3 and IgG-Fc crossreactive IgM in patients with type II mixed cryoglobulinemia and B-cell clonal proliferations. Leukemia 20:1145–1154
Pileri P, Uematsu Y, Campagnoli S et al (1998) Binding of hepatitis C virus to CD81. Science 282:938–941
Hu YW, Rocheleau L, Larke B et al (2005) Immunoglobulin mimicry by hepatitis C virus envelope protein E2. Virology 332:538–549
Ferri S, Dal Pero F, Bortoletto G et al (2006) Detailed analysis of the E2-IgM complex in hepatitis C-related type II mixed cryoglobulinaemia. J Viral Hepat 13:166–176
Galli M, Zehender G, Monti G et al (1995) Hepatitis C virus RNA in the bone marrow of patients with mixed cryoglobulinemia and in subjects with noncryoglobulinemic chronic hepatitis type C. J Infect Dis 171:672–675
Bronowicki JP, Loriot MA, Thiers V et al (1998) Hepatitis C virus persistence in human hematopoietic cells injected into SCID mice. Hepatology 28:211–218
Sung VM, Shimodaira S, Doughty AL et al (2003) Establishment of B-cell lymphoma cell lines persistently infected with hepatitis C virus in vivo and in vitro: the apoptotic effects of virus infection. J Virol 77:2134–2146
Machida K, Cheng KT, Sung VM et al (2004) Hepatitis C virus induces a mutator phenotype: enhanced mutations of immunoglobulin and protooncogenes. Proc Natl Acad Sci USA 101:4262–4267
Ito M, Murakami K, Suzuki T et al (2010) Enhanced expression of lymphomagenesis-related genes in peripheral blood B cells of chronic hepatitis C patients. Clin Immunol 135:459–465
Kasama Y, Sekiguchi S, Saito M et al (2010) Persistent expression of the full genome of hepatitis C virus in B cells induces spontaneous development of B-cell lymphomas in vivo. Blood 116:4926–4933
Tsukiyama-Kohara K, Sekiguchi S, Kasama Y et al (2011) Hepatitis C virus-related lymphomagenesis in a mouse model. ISRN Hematol 2011:167501
Alisi A, Giannini C, Spaziani A et al (2008) Involvement of PI3K in HCV-related lymphoproliferative disorders. J Cell Physiol 214:396–404
Zignego AL, Giannelli F, Marrocchi ME et al (2000) T(14;18) translocation in chronic hepatitis C virus infection. Hepatology 31:474–479
Goldberg-Bittman L, Kitay-Cohen Y, Hadari R et al (2008) Random aneuploidy in chronic hepatitis C patients. Cancer Genet Cytogenet 180:20–23
Saadoun D, Bieche I, Maisonobe T et al (2005) Involvement of chemokines and type 1 cytokines in the pathogenesis of hepatitis C virus-associated mixed cryoglobulinemia vasculitis neuropathy. Arthritis Rheum 52:2917–2925
Sansonno D, Tucci FA, Troiani L et al (2008) Increased serum levels of the chemokine CXCL13 and up-regulation of its gene expression are distinctive features of HCV-related cryoglobulinemia and correlate with active cutaneous vasculitis. Blood 112:1620–1627
Libra M, Mangano K, Anzaldi M et al (2006) Analysis of interleukin (IL)-1beta IL-1 receptor antagonist, soluble IL-1 receptor type II and IL-1 accessory protein in HCV-associated lymphoproliferative disorders. Oncol Rep 15:1305–1308
Libra M, Indelicato M, De Re V et al (2005) Elevated serum levels of osteopontin in HCV-associated lymphoproliferative disorders. Cancer Biol Ther 4:1192–1194
De Vita S, Quartuccio L, Fabris M (2008) Hepatitis C virus infection, mixed cryoglobulinemia and BLyS upregulation: targeting the infectious trigger, the autoimmune response, or both? Autoimmun Rev 8:95–99
Giannini C, Gragnani L, Piluso A et al (2008) Can BAFF promoter polymorphism be a predisposing condition for HCV-related mixed cryoglobulinemia? Blood 112:4353–4354
Gragnani L, Piluso A, Giannini C et al (2011) Genetic determinants in hepatitis C virus-associated mixed cryoglobulinemia: role of polymorphic variants of BAFF promoter and Fcgamma receptors. Arthritis Rheum 63:1446–1451
Peveling-Oberhag J, Crisman G, Schmidt A et al (2012) Dysregulation of global microRNA expression in splenic marginal zone lymphoma and influence of chronic hepatitis C virus infection. Leukemia (e-pub ahead of print)
Pasquariello A, Ferri C, Moriconi L et al (1993) Cryoglobulinemic membranoproliferative glomerulonephritis associated with hepatitis C virus. Am J Nephrol 13:300–304
Johnson RJ, Gretch DR, Yamabe H et al (1993) Membranoproliferative glomerulonephritis associated with hepatitis C virus infection. N Engl J Med 328:465–470
Daghestani L, Pomeroy C (1999) Renal manifestations of hepatitis C infection. Am J Med 106:347–354
Saadoun D, Resche-Rigon M, Thibault V, Piette JC, Cacoub P (2006) Antiviral therapy for hepatitis C virus-associated mixed cryoglobulinemia vasculitis: a long-term follow-up study. Arthritis Rheum 54:3696–3706
Fernandez-Soto L, Gonzalez A, Escobar-Jimenez F et al (1998) Increased risk of autoimmune thyroid disease in hepatitis C vs hepatitis B before, during, and after discontinuing interferon therapy. Arch Intern Med 158:1445–1448
Cacoub P, Poynard T, Ghillani P et al (1999) Extrahepatic manifestations of chronic hepatitis C. MULTIVIRC Group. Multidepartment Virus C. Arthritis Rheum. 42:2204–2212
Antonelli A, Ferri C, Fallahi P (1999) Thyroid cancer in patients with hepatitis C infection. JAMA 281:1588
Antonelli A, Ferri C, Fallahi P et al (2002) Thyroid cancer in HCV-related mixed cryoglobulinemia patients. Clin Exp Rheumatol 20:693–696
Deutsch M, Dourakis S, Manesis EK et al (1997) Thyroid abnormalities in chronic viral hepatitis and their relationship to interferon alfa therapy. Hepatology 26:206–210
Arase Y, Suzuki F, Suzuki Y et al (2009) Sustained virological response reduces incidence of onset of type 2 diabetes in chronic hepatitis C. Hepatology 49:739–744
Chen T, Jia H, Li J et al (2009) New onset diabetes mellitus after liver transplantation and hepatitis C virus infection: meta-analysis of clinical studies. Transpl Int 22:408–415
Hanouneh IA, Feldstein AE, Lopez R et al (2008) Clinical significance of metabolic syndrome in the setting of chronic hepatitis C virus infection. Clin Gastroenterol Hepatol 6:584–589
Kawaguchi T, Ide T, Taniguchi E et al (2007) Clearance of HCV improves insulin resistance, beta-cell function, and hepatic expression of insulin receptor substrate 1 and 2. Am J Gastroenterol 102:570–576
Fargion S, Piperno A, Cappellini MD et al (1992) Hepatitis C virus and porphyria cutanea tarda: evidence of a strong association. Hepatology 16:1322–1326
Ferri C, Baicchi U, la Civita L et al (1993) Hepatitis C virus-related autoimmunity in patients with porphyria cutanea tarda. Eur J Clin Invest 23:851–855
Petti S, Rabiei M, De Luca M, Scully C (2011) The magnitude of the association between hepatitis C virus infection and oral lichen planus: meta-analysis and case control study. Odontology 99:168–178
Boddi M, Abbate R, Chellini B et al (2009) Hepatitis C virus RNA localization in human carotid plaques. J Clin Virol 47:72–75
Ishizaka N, Ishizaka Y, Takahashi E et al (2002) Association between hepatitis C virus seropositivity, carotid-artery plaque, and intima-media thickening. Lancet 359:133–135
Petta S, Torres D, Fazio G et al (2012) Carotid atherosclerosis and chronic hepatitis C: a prospective study of risk associations. Hepatology 55:1317–1323
Sosner P, Wangermez M, Chagneau-Derrode C, Le Moal G, Silvain C (2012) Atherosclerosis risk in HIV-infected patients: the influence of hepatitis C virus co-infection. Atherosclerosis 222:274–277
Adinolfi LE, Restivo L, Zampino R et al (2012) Chronic HCV infection is a risk of atherosclerosis. Role of HCV and HCV-related steatosis. Atherosclerosis 221:496–502
Liu FC, Chao YC, Hou TY et al (2008) Usefulness of anti-CCP antibodies in patients with hepatitis C virus infection with or without arthritis, rheumatoid factor, or cryoglobulinemia. Clin Rheumatol 27:463–467
McAndrews MP, Farcnik K, Carlen P et al (2005) Prevalence and significance of neurocognitive dysfunction in hepatitis C in the absence of correlated risk factors. Hepatology 41:801–808
Stasi C, Zignego AL, Laffi G, Rosselli M (2011) The liver-cytokine-brain circuit in interferon-based treatment of patients with chronic viral hepatitis. J Viral Hepat 18:525–532
Cozzi A, Zignego AL, Carpendo R et al (2006) Low serum tryptophan levels, reduced macrophage IDO activity and high frequency of psychopathology in HCV patients. J Viral Hepat 13:402–408
Zignego AL, Cozzi A, Carpenedo R et al (2007) HCV patients, psychopathology and tryptophan metabolism: analysis of the effects of pegylated interferon plus ribavirin treatment 1. Dig Liver Dis 39(Suppl 1):S107–S111
Acknowledgments
This work was supported by grants from the “Associazione Italiana per la Ricerca sul Cancro” (AIRC) Investigator Grant #1461, “Istituto Toscano Tumori” (ITT), “Fondazione Istituto di Ricerche Virologiche Oretta Bartolomei Corsi”, “Fondazione Cassa di Risparmio di Pistoia e Pescia” and “Ente Cassa di Risparmio di Firenze”.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zignego, A.L., Gragnani, L., Giannini, C. et al. The hepatitis C virus infection as a systemic disease. Intern Emerg Med 7 (Suppl 3), 201–208 (2012). https://doi.org/10.1007/s11739-012-0825-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-012-0825-6