Abstract
The purpose of the present study was to determine levels of adipokines and their relationship with stiffness parameters and disease activity index in SLE patients in comparison with healthy controls. Sixty SLE patients and 29 control subjects were enrolled in the study. Serum leptin and adiponectin levels were determined by commercial sandwich ELISA kits. Colour-coded carotid duplex sonography was performed using a Siemens SONOLINE Antares machine equipped with linear 5–13 MHz. SLEDAI, ECLAM and SLICC were evaluated in all patients. Data were analysed by software for statistical analysis (Prism 5.0). Median leptin is higher among SLE patients compared with controls (p 0.035). Median values of vascular stiffness and PSEM are increased in SLE compared with controls (p = 0.0003 and p = 0.007). Vascular strain and vascular distensibility are lower in SLE patients in comparison with controls (p = 0.0001 and p = 0.0006, respectively). Considering SLE patients, leptin levels correlate with vascular stiffness (r = 0.64, p < 0.0001) and PSEM (r = 0.63, p < 0.0001). Adiponectin levels correlate with vascular strain (r = 0.28, p 0.039) and negatively correlate with vascular stiffness (r = −0.38, p 0.039). Leptin levels correlate with disease activity (SLEDAI and ECLAM) and cumulative damage (SLICC) indexes. This study demonstrates higher values of leptin in SLE patients. Moreover, SLE patients show increased levels of vascular stiffness and PSEM and reduced values of vascular strain and distensibility. These results globally indicate a decline in arterial elasticity. We find a positive correlation of leptin with stiffness parameters. According to its atheroprotective action, adiponectin inversely correlates with stiffness parameters.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Premature cardiovascular disease (CVD) is a major cause of morbidity and mortality in patients with systemic lupus erythematosus (SLE), mainly in younger women [1]. SLE patients have an increased prevalence of subclinical atherosclerotic disease detected using several modalities [2–4]. Traditional risk factors contribute to the development of atherosclerosis in SLE [5–7]. Recently, a higher prevalence of the metabolic syndrome has been described in SLE patients [8–10]. However, these risk factors alone do not explain the excess CVD risk among SLE patients, and it has been suggested that the systemic inflammatory state itself predisposes to an acceleration of atherosclerotic process [6]. The obese state is now generally considered a low-grade systemic inflammation [11]. There is strong evidence that visceral adipose tissue accumulation is an important predictive factor of lipid, glucose or atherogenic disturbances [12]. Adipokines are proteins produced mainly by adipocytes. These molecules participate in a wide variety of physiological processes including food intake, insulin sensitivity, atherosclerosis, immunity and inflammation [13]. Several studies show that adipokine production is altered in obesity, cardiovascular and immune diseases. This is observed for leptin, adiponectin and resistin and other recently discovered adipokines [14–17]. Food intake, energy status, sex hormones and inflammation mediators mainly regulate leptin synthesis. A peculiar aspect of the leptin effect on the immune system is its action as proinflammatory cytokine. Leptin deficiency is associated not only with reduced inflammation in models of autoimmune diseases, but also with increased susceptibility to infections [18]. It is associated with increased plasma C-reactive protein concentrations, vascular proliferation, calcification and decreased arterial distensibility. Moreover, leptin contributes to an increase in blood pressure, and thus, probably plays an important role in the initiation and progression of atherosclerosis [19, 20]. The prospective west of Scotland coronary prevention study (WOSCOPS) [21] shows that leptin moderately but independently increases the relative risk of coronary artery disease. Adiponectin plays a central role in the maintenance of insulin sensitivity and in down-regulating inflammatory responses. Furthermore, adiponectin exerts a protective action against atherogenesis, and a low plasma adiponectin is now recognized to be an independent risk factor of cardiovascular morbidity [22, 23]. Non-invasive imaging techniques have been used to explore why SLE predisposes women to this high CVD risk [2, 24]. Stiffness parameters (vascular stiffness, distensibility, strain and pressure strain elastic modulus) measure the reduction in artery elasticity, and their role has been validated in different studies [25, 26]. On the basis of these data, the purpose of the present study was to determine levels of adipokines and their relationship with stiffness parameters and disease activity index in SLE patients in comparison with healthy controls.
Subjects and methods
Study population
Sixty eligible patients who met the Hocheberg’s modified ACR classification criteria for SLE [27], and 29 consecutive control subjects (CTR) with no history of autoimmune diseases were enrolled in the Rheumatology Department of “Campus Bio-Medico” University of Rome. In order to minimize the hormonal effects on adipokine levels, all patients and controls were females. Exclusion criteria were subjects younger than 18 years, pregnancy, estro-progestinic assumption, nephropathy (defined as creatinine clearance <50 ml/min calculated by Cockcroft–Gault formula or serum creatinine >1.1 mg/dl, nephritic or nephrotic syndrome), increased serum liver enzymes and history of cancer. None of the SLE patients consumed more than 12.5 mg/die of prednisone during the 6 months prior of the study.
The Ethical Committee of “Campus Bio-Medico” University of Rome approved the study, performed according to the declaration of Helsinki principles. All participants gave written informed consent.
Clinical and laboratory assessment
A clinical history and physical examination findings were collected through a case sheet, concerning: fertility or menopausal status, history of diabetes or hypertension, familiar or personal CVD history. Waist/Hip ratio and body mass index were evaluated and blood pressure (BP) was recorded according to the recent guidelines [28]. For SLE patients, disease activity was assessed at the time of enrolment in the study with the use of the European consensus lupus activity measurement (ECLAM), the systemic lupus erythematosus disease activity index (SLEDAI) and the systemic lupus international collaborating clinics (SLICC) damage index (SDI) [29]. Blood specimens were collected after an overnight fast and stored at −20°C until assayed.
Autoantibodies
SLE patients’ blood specimens were analysed by indirect immunofluorescence assay (IFI) to detect anti-nuclear antibodies (ANA) on commercial Hep-2 cells substrate (Immuno concepts, Sacramento, CA, USA) and anti-dsDNA antibodies on Crithidia luciliae substrate (The Binding Site Ltd. Birmingham, UK). Two observers using positive and negative reference samples in each run evaluated the results. ENA screen on sera from SLE patients was performed by commercial ELISA kit (Orgentec Diagnostika, GmbH, Mainz, Germany). Detection and characterization of anti-cardiolipin and anti-Beta2 glycoprotein I (IgG and IgM) were carried out by ELISA using commercially available kits (ORG 515 and ORG 521––ORGenTec-Diagnostika GmbH, Mainz, Germany), according to the manufacturer’s instructions. Lupus anticoagulant was assayed following the recommendations of the International Society of Thrombosis and Haemostasis [30].
Adipokines
Serum leptin levels were determined by commercial sandwich ELISA kits (Leptin sandwich ELISA kit EIA-2395, DRG Instruments GmbH, Germany) with a 6.2% intra-assay precision, a 6.5% inter-assay accuracy and an analytical sensitivity of 1 ng/ml. Serum levels of adiponectin were determined by commercial ELISA kit (Human Adiponectin ELISA kit Cat. No. A0512EK, AdipoGen, Seoul, Korea) with 4.59% intra-assay precision and 5.6% inter-assay accuracy. The reported analytical sensitivity was 100 pg/ml.
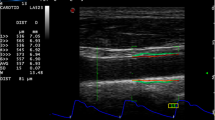
Carotid duplex sonography
Colour-coded carotid duplex sonography was performed in all patients in the supine decubitus position, during quiet respiration. The study was conducted by the same operator using a Siemens SONOLINE Antares (Colorado, USA) machine equipped with linear 5–13 MHz transducer placed on the patient’s neck with the least possible pressure so as not to compress the overlying jugular vein and to allow expansion of the carotid artery in all directions. The carotid view was achieved in longitudinal scan on the extracranial artery segment at 1 cm from the right and left common carotid bulb. In accordance with others, stiffness parameters were assessed evaluating the diameter changes of the common carotid between systole and diastole during a cardiac cycle. Common carotid diameters at systole (sDIA) and diastole (dDIA) were analysed in M-Mode approach as the major increase and reduction in the vessel-diameter during the cardiac cycle, after tracking the two interface walls for 10 consecutive cardiac cycles. The diameters were measured by means of a calibre in systole and diastole as the distance between the trailing edge of the anterior wall and the leading edge of the posterior wall. In accordance with previous studies, stiffness parameters [common carotid vascular strain (VS), vascular distensibility (VD), vascular stiffness (VSf) and pressure–strain elastic modulus (PSEM)] were calculated applying the following equations:
where sBP is the systolic blood pressure; dBP the diastolic blood pressure; and k the conversion factor from mmHg to Pa (k = 7×0-3).
All data are expressed as the mean of the right and left carotid measurements of each subjects.
Statistical analysis
Data were analysed by software for statistical analysis (Prism 5.0, Inc., San Diego, California, USA). Comparisons of continuous variables among groups were performed by Mann-Whitney U test. The categorical variables were analysed by Fisher F test. Correlations were calculated by Sperman’s tests. Two-sided p values <0.05 were considered statistically significant.
Results
Demographic and SLE features
Demographic and clinical characteristics of the population study are given in Table 1. No difference was found between the two groups with regard to age, fertile or menopausal status, BMI, hypertension and smoking history. All SLE patients are on steroids. Mean prednisone or equivalent daily dosage was 7.95 ± 5 mg.
Adipokines levels in SLE patients and controls
Adipokines levels in SLE patients and controls are reported in Table 2. No significant difference in leptin and adiponectin values of SLE patients, with or without antiphospholipid syndrome, was found. Twenty-eight out of fifty patients suffered from neuropsychiatric SLE according to criteria for the diagnosis of NP-SLE; 15 patients had haematological involvement (haemolytic anaemia and/or leucopoenia); 49 had history of myositis and/or arthritis. We did not find differences about leptin and adiponectin levels in the respective subgroups.
Stiffness parameters
The median values of vascular stiffness were increased in SLE compared with controls in the global group and in fertile subjects (p = 0.0003 and p = 0.0003, respectively). We did not find any difference in vascular stiffness between groups, considering menopausal subjects only (p = 0.14). We found higher median PSEM in SLE patients than controls (p = 0.0007) and above all in fertile women (p = 0.0011). The median PSEM values did not differ among menopausal subjects (p = 0.092). Vascular strain and vascular distensibility median values were higher in controls in comparison with SLE patients (p = 0.0001 and p = 0.0006, respectively). Fertile control subjects showed increased median values of vascular strain and vascular distensibility (p = 0.0001 and p = 0.0024, respectively).
We did not find any difference in vascular strain and vascular distensibility median values among menopausal women (p = 0.14 and p = 0.065, respectively) (Fig. 1).
Stiffness parameters correlation with cardiovascular risk factors
Considering SLE patients, vascular stiffness correlated with systolic blood pressure (r = 0.32, p = 0.032) and BMI (r = 0.58, p = 0.0001). We found positive correlations between PSEM and systolic blood pressure (r = 0.51, p = 0.0001) and BMI (r = 0.62, p = 0.0001). Vascular strain negatively correlated with BMI (r = −0.59, p = 0.0001). Vascular distensibility was negatively related to systolic blood pressure (r = −0.50, p = 0.0007) and BMI (r = −0.63, p = 0.0001).
There was no correlation between ecocolordoppler parameters and blood pressure or BMI in controls. No significant correlation was found between stiffness parameters, cumulative dose and duration of steroid intake.
Adipokines correlation with stiffness parameters
Leptin positively correlated with vascular stiffness (r = 0.64, p < 0.0001) and PSEM (r = 0.63, p < 0.0001). This adipokine negatively correlated with vascular strain (r = −0.6, p < 0.0001) and vascular distensibility (r = −0.64, p < 0.0001).
Adiponectin levels inversely correlated with vascular stiffness (r = −0.38, p = 0.0039) and PSEM (r = −0.36, p = 0.006). We found a direct correlation between adiponectin and vascular Strain (r = 0.27, p = 0.03) and vascular distensibility (r = 0.36, p = 0.005).
Leptin correlation with disease activity indexes
We found a positive correlation between leptin and SLE-specific disease activity index SLEDAI (r = 0.54, p < 0.0001) and ECLAM (r = 0.58, p < 0.0001) and cumulative damage (SLICC) index (r =0.4, p= 0.0023). There is no correlation between the reported indexes and the adiponectin levels. We did not find any correlation with disease activity indexes considering stiffness parameters (Fig. 2).
Discussion
Although survival in SLE patients dramatically improved in the past decades, an increased incidence and prevalence of CVD is reported. Autopsy studies demonstrate that the coronary vessels of SLE patients have atherosclerotic plaque, and most cardiovascular events are not attributable to active vasculitis [1, 31]. Current data clearly show that even young fertile SLE women are at high CVD risk. This phenomenon has been called “premature atherosclerosis”. Unfortunately, to date, no single risk factor or group of risk factors has been uniformly helpful in predicting which patients will have atherosclerotic cardiovascular events. Nonetheless, the development of novel laboratory markers, the identification of genetic polymorphisms linked to cardiovascular risk factors, and new imaging techniques have all held the promise of a better prediction of cardiovascular events in SLE patients [6, 7, 31]. Several studies have investigated subclinical atherosclerosis in SLE by measurement of IMT, yielding conflicting results. A recent study shows risk factors for increased carotid intima-media thickness in paediatric SLE patients [32]. Recently, Cacciapaglia et al. and de Leeuw et al. showed higher IMT values in SLE patients than in controls, independently of previous CVD [2, 33]. Vascular stiffness parameters are related to premature atherosclerosis and cardiovascular diseases in different settings of population [34]. According to these data, we find that SLE patients, compared with controls, show increased levels of vascular stiffness and PSEM and reduced values of vascular strain and distensibility. These results globally indicate a decline in arterial elasticity. Literature data agree in underlying the increased vascular stiffness among SLE patients. Shang et al. and Brodszki et al. show augmented arterial stiffness in SLE at common carotid level and at abdominal aorta and popliteal artery levels [35, 36]. Moreover, Chow et al. demonstrate that young SLE patients, with a mean age of 17 years, present increased vascular stiffness [37].
In a recent paper, carotid ultrasonography was performed in 250 women with SLE and plasma leptin levels were measured. In this cohort, leptin levels are associated with the presence of subclinical atherosclerosis, even after accounting for traditional cardiac and disease factors [38].
In our studies stiffness parameters are related to BMI and systolic blood pressure. BMI is recognized as a determinant factor in the development of cardiovascular disease. Recent and current data support the implication of adipose tissue in atherogenesis. In fact, visceral adipose tissue secretes a wide spectrum of molecules that constitutes a network with cytokines released by immune cells. Parts of this network are tumour necrosis factor-alfa (TNF-alfa), interleukin-6 (IL-6), macrophage and monocyte chemoattractant protein (MCP-1) and plasminogen activator inhibitor (PAI-1); all these molecules are implied in atherogenesis [16, 17].
In a preliminary paper, our group demonstrated hyperexpression of leptin in SLE patients, notably, among fertile subjects [9]; moreover, we find that in SLE patients, leptin correlates with parameters related to the metabolic syndrome and to cardiovascular risk factors. To compare two different models of autoimmune diseases, we study leptin levels and metabolic and cardiovascular risk factors in Sjogren Syndrome and Systemic Lupus Erythematosus. Leptin levels are higher in SLE and SS than in controls. Among SS patients, leptin correlates with insulin levels, HOMA-IR, BMI, waist circumference and systolic blood pressure. We conclude that leptin might be involved in the metabolic imbalance and is related to different cardiovascular disease risk factors in patients with two different autoimmune diseases [39].
In the present study, we confirm higher leptin levels in SLE patients with respect to controls; moreover, we find a positive correlation of leptin with stiffness parameters.
Leptin exerts many proatherogenic effects, and its role in atherogenesis has been widely investigated. In fact, this adipokine has been implied in endothelial dysfunction interfering with NO production and NO-mediated vasorelaxion. Moreover, leptin promotes oxidative stress, increasing reactive oxygen species (ROS) production, possibly acting at respiratory chain level. Experimental models show that leptin induces small muscle cell proliferation and migration and facilitates plaque destabilization and subsequent thrombosis. Finally, leptin exerts proinflammatory properties, leading to an increased production of cytokines as TNF-α, IL-1, IL-6 and switching the phenotype toward a TH1 response [20, 21]. According to its atheroprotective action, in our studies adiponectin inversely correlates with stiffness parameters.
In vitro data underline that adiponectin defends endothelial cells against oxidative injury and dysfunction. In fact, this adipokine reduces adhesion molecules expression on endothelial surface, stimulates NO production, thereby improving endothelium-dependent vasodilation, and seems to suppress endothelial cells apoptosis. Moreover, adiponectin antagonizes macrophage to foam cells transformation and smooth muscle cell proliferation and migration. Adiponectin suppresses vascular remodelling, increasing tissue inhibitors of matrix metalloproteinases. Furthermore, this adipokine shows immunomodulating actions, up-regulating interleukin-10 (IL-10) and interleukin-1 receptor antagonist (IL-1Ra) and down-regulating TNF-alfa and IL-6 [23]. Chronic inflammation plays a crucial role in atherogenesis among SLE patients. Indeed, traditional CVD risk factors do not fully explain the increased propensity toward CVD described in SLE. According to that, in our study leptin correlates with SLE-specific disease activity index SLEDAI and ECLAM. These data possibly indicate a participation of SLE-related inflammation such as autoantibody production, inflammatory cytokines, oxidative stress and renal involvement, in early atherosclerotic disease. Moreover, we find a positive correlation between leptin and SLE cumulative damage (SLICC) index. These data support a role of the molecule not only in atherogenesis, but also in chronic inflammation.
In conclusion, we find increased values of stiffness parameters in SLE patients, especially among fertile women, indicating a high prevalence of subclinical atherosclerosis. Stiffness parameters are related to adipokines, and leptin is also related to disease activity. As a consequence, to antagonize atherosclerosis it is necessary to have not only a tight control of traditional CVD risk factors, but also an intensive management of disease activity.
References
Abu-Shakra M, Codish S, Zeller L, Wolak T, Sukenik S (2008) Atherosclerotic cardiovascular disease in systemic lupus erythematosus: the Beer Sheva experience. Isr Med Assoc J 10:43–44
Cacciapaglia F, Zardi EM, Coppolino G, Buzzulini F, Margiotta D, Arcarese L et al (2009) Stiffness parameters, intima-media thickness and early atherosclerosis in systemic lupus erythematosus patients. Lupus 18:249–256
Roman MJ, Shanker BA, Davis A et al (2003) Prevalence and correlates of accelerated atherosclerosis in systemic lupus erythematosus. N Eng J Med 349:2399–2406
El Magadmi M, Bodill H, Ahmad Y et al (2004) Systemic lupus erythematosus: an independent risk factor for endothelial dysfunction in women. Circulation 110:399–404
McMahon M, Grossman J, Skaggs B, Fitzgerald J, Sahakian L, Ragavendra N et al (2009) Dysfunctional proinflammatory high-density lipoproteins confer increased risk of atherosclerosis in women with systemic lupus erythematosus. Arthritis Rheum 30:2428–2437
Ahmad Y, Shelmerdine J, Bodill H, Lunt M, Pattrick MG, Teh LS et al (2007) Subclinical atherosclerosis in systemic lupus erythematosus (SLE): the relative contribution of classic risk factors and the lupus phenotype. Rheumatology (Oxford) 46:983–988
Doria A, Shoenfeld Y, Wu R (2003) Risk factors for subclinical atherosclerosis in a prospective cohort of patients with systemic lupus erythematosus. Ann Rheum Dis 62:1071–1077
Pereira RM, de Carvalho JF, Bonfá E (2009) Metabolic syndrome in rheumatological diseases. Autoimmun Rev 8:415–419
Vadacca M, Margiotta D, Rigon A, Cacciapaglia F, Coppolino G, Amoroso A et al (2009) Adipokines and systemic lupus erythematosus: relationship with metabolic syndrome and cardiovascular disease risk factors. J Rheumatol 36:295–297
Chung CP, Avalos I, Oeser A, Gebretsadik T, Shintani A, Raggi P et al (2007) High prevalence of the metabolic syndrome in patients with systemic lupus erythematosus: association with disease characteristics and cardiovascular risk factors. Ann Rheum Dis 66:208–214
Ohman MK, Wright AP, Wickenheiser KJ, Luo W, Eitzman DT (2009) Visceral adipose tissue and atherosclerosis. Curr Vasc Pharmacol 7:169–179
Calabrò P, Golia E, Maddaloni V, Malvezzi M, Casillo B, Marotta C et al (2009) Adipose tissue mediated inflammation: the missing link between obesity and cardiovascular disease? Intern Emerg Med 4:25–34
Antuna-Puente B, Feve B, Fellahi S, Bastard JP (2008) Adipokines: the missing link between insulin resistance and obesity. Diabetes Metab 34:2–11
Lambert M, O’Loughlin J, Delvin EE, Levy E, Chiolero A, Paradis G (2009) Association between insulin, leptin, adiponectin and blood pressure in youth. J Hypertens 27:1025–1032
Bo S, Gambino R, Gentile L, Pagano G, Rosato R, Saracco GM et al (2009) High-normal blood pressure is associated with a cluster of cardiovascular and metabolic risk factors: a population-based study. J Hypertens 27:102–108
Tilg H, Moshen AR (2006) Adipocytochinines: mediators linking adipose tissue, inflammation and immunity. Nature 6:772–783
Lau DCW, Dhillon B, Yan H, Szmitko PE, Verma S (2005) Adipokines: molecular links between obesity and atherosclerosis. Am J Physiol Heart Circ Physiol 288:2031–2041
Lam QL, Lu L (2007) Role of leptin in Immunity. Cellular & Molecular Immunology 4:1–13
Bełtowski J (2006) Role of leptin in blood pressure regulation and arterial hypertension. J Hypertens 24:789–801
Beltowsku J (2006) Leptin and atherosclerosis. Atherosclerosis 189:47–60
Wallace AM, McMahon AD, Packard CJ, Kelly A, Shepherd J, Gaw A, Sattar N (2001) Plasmaleptin and the risk of cardiovascular disease in the west of Scotland coronary prevention study (WOSCOPS). Circulation 104:3052–3056
Kadowaki T, Yamauchi T, Kubota N, Hara K, Ueki K, Tobe K (2006) Adiponectin and adiponectin receptors in insulin resistance, diabetes, and metabolic syndrome. J Clin Invest 116:1784–1792
Han SH (2007) Adiponectin and cardiovascular disease. J Am Coll Cardiol 49:531–538
Tziomalos K, Tziomalos K, Sivanadarajah N, Mikhailidis DP, Boumpas DT, Seifalian AM (2008) Increased risk of vascular events in systemic lupus erythematosus: is arterial stiffness a predictor of vascular risk? Clin Exp Rheumatol 26:1134–1145
Mattace-Raso FU, van der Cammen TJ, Hofman A, van Popele NM, Bos ML, Schalekamp MA et al (2006) Arterial stiffness and risk of coronary heart disease and stroke: the Rotterdam Study. Circulation 113:657–663
Parati G, Bernardi L (2006) How to assess arterial compliance in humans. J Hypertens 24:1009–1012
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40:1725
Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G et al (2007) Guidelines for the management of arterial hypertension: the task force for the managementof arterial hypertension of the European society of hypertension (ESH) and of the European society of cardiology (ESC). J Hypertens 25:1105–1187
Griffiths B, Mosca M, Gordon C (2005) Assessment of patients with systemic lupus erythematosus and the use of lupus disease activity indices. Best Pract Res Clin Rheumatol 19:685–708
Brandt JT, Triplett DA, Alving B, Scharrer I (1995) Criteria for the diagnosis of lupusanticoagulants: an update On behalf of the Subcommittee on Lupus Anticoagulant/Antiphospholipid Antibody of the Scientific and Standardization Committee of the ISTH. Thromb Haemost 74:1185–1190
Von Feldt JM (2008) The cardiovascular threat of lupus. Nat Clin Pract Rheumatol 4:505
Schanberg LE, Sandborg C, Barnhart HX, Ardoin SP, Yow E, Evans GW et al (2009) Atherosclerosis prevention in pediatric lupus erythematosus investigators. prematureatherosclerosis in pediatric systemic lupus erythematosus: risk factors for increased carotidintima-media thickness in the atherosclerosis prevention in pediatric lupus erythematosuscohort. Arthritis Rheum 60:1496–1507
De Leeuw K, Smit AJ, de Groot E, van Roon AM, Kallenberg CG, Bijl M. Longitudinal study on premature atherosclerosis in patients with systemic lupus erythematosus. Atherosclerosis 2009; 25
Cypiene A, Kovaite M, Venalis A, Dadoniene J, Rugiene R, Petrulioniene Z et al (2009) Arterialwall dysfunction in systemic lupus erythematosus. Lupus 18:522–529
Shang Q, Tam LS, Li EK, Yip GW, Yu CM (2008) Increased arterial stiffness correlated with disease activity in systemic lupus erythematosus. Lupus 17:1096–1102
Brodszki J, Bengtsson C, Länne T, Nived O, Sturfelt G, Marsál K (2004) Abnormal mechanical properties of larger arteries in postmenopausal women with systemic lupus erythematosus. Lupus 13:917–923
Chow PC, Ho MH, Lee TL, Lau YL, Cheung YF (2007) Relation of arterial stiffness to left ventricular structure and function in adolescents and young adults with pediatric-onset systemic lupus erythematosus. J Rheumatol 6:1345–1352
McMahon M, Skaggs BJ, Sahakian L, Grossman J, FitzGerald J, et al. High plasma leptin levels confer increased risk of atherosclerosis in women with systemic lupus erythematosus, and are associated with inflammatory oxidised lipids. Ann Rheum Dis 2011; June 13
Vadacca M, Margiotta D, Sambataro G, Cacciapaglia F, Rigon A, Buzzulini F, Afeltra A (2010) Leptin levels in patients affected by Sjogren’s syndrome and systemic lupus erythematosus. Ann Rheum Dis 69(Suppl3):573
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vadacca, M., Zardi, E.M., Margiotta, D. et al. Leptin, adiponectin and vascular stiffness parameters in women with systemic lupus erythematosus. Intern Emerg Med 8, 705–712 (2013). https://doi.org/10.1007/s11739-011-0726-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-011-0726-0