Abstract
The classic myeloproliferative neoplasms (MPNs) include polycythemia vera and essential thrombocythemia; their molecular basis has been described only recently with the demonstration of recurrent mutations in JAK2 or MPL. While life expectancy may not be significantly shortened, arterial and venous thrombosis constitute the major causes of morbidity and mortality, together with disease evolution to myelofibrosis or transformation to acute leukemia. Therapy is currently aimed at reducing the rate of thrombosis without increasing the risk of hematologic transformation by inappropriate exposure to cytotoxic drugs. Nevertheless, the mechanism(s) finally responsible for the increased thrombotic tendency have not been clearly elucidated, although risk factors for thrombosis have been identified, and are currently employed for stratifying patients to the most appropriate therapeutic options. Abnormalities of blood cells, activation of neutrophils and platelets, and a hypercoagulability state, can all act in conjunction to lead to thrombosis. Intriguing data also point to the JAK2V617F mutation as both a marker and a mechanism for thrombosis. Better knowledge in the pathophysiology of these disorders, and the introduction of molecularly targeted drugs in clinical trials, anticipate the possibility of more specific and efficacious treatment of classic MPN, particularly as concerns the reduction of risk associated with vascular events.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Polycythemia vera (PV) and essential thrombocythemia (ET), together with Primary Myelofibrosis (PMF), represent the classic, Philadelphia-chromosome (Ph’)-negative chronic myeloproliferative neoplasms (MPNs), as they are listed in the recent classification from the World Health Organization (WHO) (Table 1) [1, 2]. These disorders had initially been grouped together by William Dameshek in 1951, based on similarities in their clinical phenotype and the hypothesis that they should be ascribed to an underlying global myeloproliferation [3]. The “classic” MPNs are kept separate from other myeloproliferative conditions that include chronic neutrophilic leukemia (CNL), chronic eosinophilic leukemia (CEL) and hypereosinophilic syndrome (HES), systemic mastocytosis (SM), unclassifiable forms of MPNs, as well as from Phildelphia chromosome/BCR-ABL-positive chronic myelogenous leukemia (CML) [4]. Furthermore, they should be differentiated accurately from non-neoplastic, reactive conditions. The 2008 WHO classification has been revised, compared to the previous one dated 2001, mainly because of the discovery of specific molecular abnormalities associated with these disorders reported in the prior 3 years .
The classic MPNs are common hematologic neoplasias, mainly affecting individuals over 50–60 years. In a survey [5] from the USA, the average 2001–2003 annual, age-adjusted, cumulative rate for PV, ET and PMF is 2.1 per 100,000, totaling to the rate of 13.3 per 100,000 among individuals aged greater than 80. However, due to their relatively smooth clinical course, many cases of PV or ET are probably not reported to registries, and even go undiagnosed, so that the true occurrence of these disorders is likely higher.
Molecular pathogenesis of MPN
The clonal origin of PV and ET in a common myeloid stem cell has been demonstrated long ago in clonality studies using enzymatic or genetic markers. These disorders share a number of biological features among which in particular is a hypersensitivity to cytokines, such as erythropoietin (Epo), thrombopoietin (Tpo), interleukin-3 (IL-3) and stem cell factor (SCF), that enables the presence of erythroid progenitor cells capable of proliferating and differentiating in the absence of Epo (so called “endogenous erythroid colonies”-EEC). Presence of EEC represents one of the accessory criteria used in the diagnosis of PV in the 2008 WHO criteria (Table 2). Both PV and ET are characterized by overproduction of mature blood elements, with predominance of erythroid and megakaryocytic lineage, respectively; and by a variable degree of bone marrow fibrosis, that may eventually contribute to the transformation to post-PV or post-ET myelofibrosis (PPV/PET-MF) [6]; extramedullary hematopoiesis, particularly in the spleen and the liver, typical of more advanced phases of the diseases, and particularly in case of transformation to PPV/PET-MF; the propensity to evolve to acute myelogenous leukemia; and, notably, an usually high rate of occurrence of thrombotic events, and, less commonly, of hemorrhages.
In 2005, the first recurrent molecular abnormality of MPNs, represented by a point mutation in JAK2 exon 14, was identified. The mutation causes a valine-to-phenylalanine substitution at position 617 (V617F) in the JH2 (JAK Homolog) auto-inhibitory domain, and results in a gain-of-function of JAK2 that autonomously activates downstream signaling pathways, including JAK-STAT, PI3K/Akt, and ERK1/2 MAPK [7]. Factor-dependent cell lines become growth-factor independent after transduction with the V617F allele. Furthermore, mice transplanted with JAK2V617F transduced cells in a retroviral expression model developed a PV-like phenotype, eventually followed by hematological and histopathological modifications suggestive of myelofibrotic transformation [7, 8]. More recently, transgenic mice have been developed that express lower ratio of mutated versus wild-type JAK2. These mice display an ET-like phenotype with thrombocytosis but not erythrocytosis nor leukocytosis. Overall, these animal models indicate that the JAK2V617F allele is sufficient to induce a MPN-like disease, and that the ratio of mutated and un-mutated allele influences phenotype.
The JAK2V617F mutation is found in over 95% of PV and 60% of ET or PMF patients. In most PV patients, as opposed to a minority of ET patients, only the mutated allele is found in hematopoietic cells (homozygosity) due to a process of mitotic recombination [8–10]. Subsequently, in some patients with a diagnosis of V617F-negative PV, other genetic abnormalities (including mutations, deletions, insertions) were found in JAK2 exon 12 [11]. These mutations induce a constitutive activation of JAK-STAT pathway at an even greater level than the V617F allele, and cause a PV phenotype when expressed in a mouse transplant model. Therefore, exon 12 abnormalities functionally overlap with the V617F allele, but typically, they are associated with a “pure” erythroid phenotype. Another recurrent molecular abnormality is represented by mutations involving codon 515 of MPL [12, 13], the gene encoding the receptor for the cytokine thrombopoietin (Tpo). These point mutations (that lead to a W to L, K or A transition) are located in a RWFQP motif in the transmembrane-juxtamembrane junction of the receptor. Substitutions at W515 probably alter the inactive conformation of Mpl, and result in its ligand-independent activation. The expression of the W515L allele in mice results in extreme thrombocytosis and leukocytosis, bone marrow reticulin fibrosis, extramedullary hematopoiesis, and significant shortening of life span, mimicking human primary myelofibrosis rather than PV or ET. However, MPL mutations have been detected both in patients with PMF (≅ 8%) and ET, and in whom they account for up to 9% of JAK2V617F-negative cases [12–14]. They have not yet been reported in PV. ET patients harboring MPL mutation display significantly higher platelet count than MPL wild type, while their hemoglobin levels are lower [15, 16], as previously observed also in PMF patients [14]. The coexistence of MPL mutations and the JAK2V617F allele is reported in some patients [14, 15]. The presence of JAK2 or MPL mutations represents a major criteria in the revised 2008 WHO diagnostic criteria (Table 2), although it must be realized that up to 30–40% of ET or PMF patients do not have mutations in either JAK2 or MPL, and are mutational undefined [1].
It is still controversial how a single mutation in JAK2 or MPL might associate with different clinical phenotypes. Several not mutually exclusive possibilities may be the explanation. Different diseases may be associated with a variable burden of hematopoietic cells bearing the mutant V617F allele (with PV and ET being at the highest and lowest side, respectively). In addition, it is likely that genetic mutational events other than JAK2 or MPL collaborate in the pathogenesis of MPNs, and may also anticipate those mutations as recently reported for TET-2 mutations [17]. In addition, individual characteristics, genetic modifiers, or epigenetic modulators may contribute to phenotypic heterogeneity of MPNs [18].
Thrombosis in MPNs: clinical aspects
Thrombosis, hemorrhage, evolution to post-polycythemic or post-thrombocythemic myelofibrosis, and transformation to AML represent the most relevant events occurring in the course of MPNs. However, while there are a relatively large number of studies retrospectively investigating thrombosis occurrence and characteristics in MPN, there is a shortage of prospective trials. These are essentially represented by the “Bergamo trial”, that compared hydroxyurea (HU) versus no treatment in 114 ET patients [19], the experimental (n = 518) [20] and observational (n = 1,638) [21] arms of the European Collaboration on Low-dose Aspirin in Polycythemia Vera (ECLAP) trial, and the Primary Thrombocythemia-1 (PT-1) [22] study in 809 patients with ET.
The cumulative rate of thrombosis ranges from 2.5 to 5.0% per patient-year in PV, and from 1.9 to 3% per patient-year in ET, according to the patient risk category [21, 22]. The initial thrombotic event may occur at the time of diagnosis, or in the follow-up period. In a recent survey from Italian GIMEMA group, the calculated recurrence rate is 5.6% per patient-year, and the cumulative probability is 49.9% at 10 years [23]. Arterial thromboses represent 60–70% of all cardiovascular events, and include acute myocardial infarction (AMI), ischemic stroke, and peripheral arterial occlusion. Venous thromboses, such as deep venous thrombosis of the extremities and pulmonary embolism, are more common in PV than ET. Splanchnic vein thromboses (SVT), including portal vein thrombosis, mesenteric thrombosis, and thrombosis of the hepatic veins causing Budd–Chiari syndrome, have an unusually high prevalence among MPN patients [24]. The involvement of the microcirculatory system, particularly common in ET patients, manifests as erythromelalgia, transient ischemic attacks (TIA), visual or hearing transitory defects, recurrent headache, and peripheral paresthesia.
Fatal cardiovascular events and disease transformation to myelofibrosis or AML account for most of the deaths in PV and ET. The mortality rate is increased in PV patients in an age-dependent manner [25], while life expectancy may be normal in the majority of patients with ET [25]. However, even in the latter, survival becomes worst after 10–15 years from diagnosis, according to some studies.
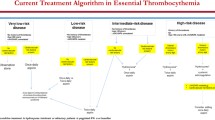
Since cardiovascular events represent the leading cause of morbidity and mortality in the course of PV and ET, the criteria for stratifying patients are currently based on this clinical end-point [26]. Older age (>60 years), and a previous history of thrombosis are considered as standard risk factors for thrombosis in both PV and ET (Table 3), which have been validated in several studies [21]. In the presence of either of these, a patient is defined “at high-risk”, while when neither of these is present, the disease is low-risk (Table 3). The contribution of generic cardiovascular risk factors, such as hypertension, diabetes, hyperlipidemia, smoking, or genetic alterations of hemostatic factors is still controversial, although ET subjects presenting any of these abnormalities may belong to an intermediate-risk category.
Pathophysiology of thrombosis in MPNs
The pathogenesis of thrombosis in the classic MPNs is multifactorial and complex. Rheological abnormalities due to an increased red cell mass in PV, abnormalities in platelet function, involvement of leukocytes and possibly of endothelial cells, and activation of the coagulation system favoring a hypercoagulable state may all collaborate to produce the thrombotic diathesis of MPN [27].
However, neither thrombocytosis nor increased hematocrit per se has been clearly associated with occurrence of thrombosis [28]. In a study in a small population of PV patients, a striking correlation between the occurrence of thrombosis and hematocrit level is demonstrated [29], and this study has represented the “gold standard” in the field. Nevertheless, this paradigm has been challenged recently by a retrospective analysis within the ECLAP trial where a time-dependent multivariate analysis fails to show any correlation between an hematocrit level in the range <45% up to 52% and the occurrence of major cardiovascular events [28]. However, the lower threshold are not easily tolerated by most subjects because of the need for frequent phlebotomies, and the resulting severe, often symptomatic, iron deficiency. In addition, the lack of a clear correlation between thrombosis and hematocrit, as discussed above, has prompted a prospective clinical trial in Italy (CytoPV; EudraCT 2007-006694-91) whose primary endpoint is to analyze the appropriateness of a target hematocrit level of up to 45% or in the range 45–50% in respect to thrombosis risk in PV patients.
The same analysis of the ECLAP trial also shows that platelet count in the range <300 × 109/L to >500 × 109/L does not impact on thrombosis, consistent with a case control study from the PVSG-01 trial where the platelet count at the closest observation prior to thrombosis was not associated with the thrombotic event itself [28]. In addition, in a series of 99 young ET patients with extreme thrombocytosis, no clear impact of platelet count on thrombotic events can be demonstrated, irrespective of the use of cytotoxic treatment [30]. Conversely, it is commonly held that extreme thrombocytosis in the course of MPN (in the excess of 1,500 × 109/L) is associated with increased bleeding due to an acquired von Willebrand disease, although definite studies in this regard are not available. Finally, reactive thrombocytosis, even at extreme levels, is not associated with an increased risk of thrombosis, that in the few reported causes was probably ascribable to the underlying cause (i.e., thrombophilia associated with cancer) rather than to the increased platelet count per se.
On the other hand, leukocytosis has been shown to represent an additional independent risk factor for thrombosis [31]. In a retrospective analysis of the ECLAP observational arm in PV patients, adjusted for potential confounders such as cytoreductive and antithrombotic treatment, a leukocyte count greater than 10 × 109/L is found to be associated with a raised rate of thrombosis; particularly, in patients with a leukocyte count greater than 15 × 109/L. The hazard ratio of thrombosis in general is 1.71 (95% CI 1.10–2.65) and 2.84 (95% CI 1.25–6.46) in the case of acute myocardial infarction. Similarly, in a retrospective cohort of 1,063 patients with ET, those subjects with a baseline leukocyte count greater than 11 × 109/L have a significantly higher risk of major thrombosis as compared to those with normal leukocytes (lower than 8 × 109/L). Furthermore, by combining leukocyte and platelet count in different patient categories, the group of patients with the highest thrombosis rate (2.95% patients/year) is constituted of subjects with leukocytosis, a lower platelet count, and a JAK2V6217F mutated genotype, independently from conventional risk factors. Similar observations are reported by Wolanskyi et al. in a retrospective study in 322 ET patients. Leukocytosis also helped in better definition of risk, at least retrospectively. In fact, “low-risk” ET patients could be separated into two categories with an overall prevalence of thrombosis of 55 and 20%, respectively, based on an absolute leukocyte count greater or lower than 8.7 × 109/L.
A JAK2V617F mutated status in ET [32–34], and a high V617F allelic burden in both ET [33, 35] and PV [36], have been variably associated with an increased risk of thrombosis [37]. Three independent meta-analyses have re-evaluated published series. In one of these, 2,905 patients with ET, among whom there were 778 with thrombosis, were included [38]. The results indicate that a JAK2V617F mutated status is associated with an increased risk of venous thrombosis (OR 2.09, 95% CI 1.44–3.05), arterial thrombosis (OR 1.96, 95% CI 1.43–2.67), and thrombosis at presentation (OR 1.88, 95% CI 1.38–2.56). In the analysis from Dahabreh et al. [39], 2,436 patients were included with an overall incidence of thrombosis of 26.4%; risk of arterial (OR 1.68, 95% CI 1.31–2.15) and venous (OR 2.5, 95% CI 1.71–3.66) thromboses were significantly increased in JAK2V617F mutated patients compared to wild-type. Similar conclusions are obtained by Lussana et al. [40] who analyzed 3,150 patients, confirming that the rate of thrombotic events is significantly higher in JAK2V617F-mutated (32 vs. 20% in un-mutated patients; OR for total thrombosis, 1.92, 95% CI 1.4–2.53). The OR for arterial thrombosis is 1.77 (95% CI 1.29–2.43) and 2.49 (95% CI 1.71–3.61) for venous thrombosis; also, although the information is limited to a few studies, the risk of microcirculatory disorders is found to be significantly higher among JAK2V617F-mutated patients (OR 2.1, 95% CI 1.18–3.63). Furthermore, the rare ET patients (2–4% of mutated subjects) who were homozygous for the mutation, have an exceedingly high risk of total thrombosis, after multivariate adjustment for potential confounders (HR 3.97, 95% CI 1.34–11.7) [35]. Studies in PV are fewer, and the results are less homogeneous. However, in a prospective study on 173 PV who were genotyped at diagnosis, those subjects who have a mutated allele burden greater than 75% have a 3.56-fold higher relative risk (95% CI 1.47–7.1) of total thrombosis, that was largely accounted for by thromboses during the follow-up period (RR 7.1, 95% CI 1.6–10.1) [36].
There is a strong association between the presence of an underlying MPN and SVT [41]. In a recent survey on 241 such patients, the JAK2V617F mutation is found in 45% of Budd–Chiari syndromes and 34% of portal vein thromboses [24]. The OR of a SVT in the presence of a JAK2V617F mutation is 53.98 (95% CI 13.10–222.45) compared to JAK2 wild-type subjects; this justifies the routine genotyping of SVT patients [42].
Therefore, both leukocytosis and JAK2V617F mutational status may represent novel disease-associated risk factors that should be incorporated in the current risk stratification; unlike age and history of thrombosis, they are potentially modifiable with therapy. Notwithstanding, at the present time, firm evidence that leukocytosis has a causative role in the pathogenesis of cardiovascular events in MPN rather than being simply a marker associated with the events, is lacking, and prospective validation in clinical trials is warranted; the same holds true for JAK2V617F mutation and the burden of mutated allele. Nevertheless, there is increasing experimental evidence to support a pathogenetic role of neutrophils in MPN thrombosis. Activated neutrophils and platelets can be detected in the circulation of MPN patients, particularly in those who are JAK2V617F mutated. Activated neutrophils display overexpression of membrane adhesion molecules such as the β2 integrin CD11b, express leukocyte alkaline phosphatase in a JAK2V617F-dependent manner [36, 43], and have a characteristic gene expression profile. Plasma levels of neutrophil-derived enzymes, such as myeloperoxidase and elastase, are typically increased [44]. An increased percentage of platelet-leukocyte aggregates has been detected in the circulation of ET and PV patients, indirectly shown to be dependent on leukocyte CD11b expression, and is reduced by aspirin treatment (Fig. 1). A thrombophilic condition in MPN patients, supported by elevated plasma markers of hyper-coagulation, may be facilitated by the activated neutrophils and platelets [45]. It can contribute to the acquired activated protein C resistance (APC) associated with low free protein-S levels that have been detected in ET or PV patients [46] and also interact with a JAK2V617F mutated status by further raising the risk of thrombosis in younger ET patients [47].
Indications for treatment
The cornerstone of treatment in low-risk patients with PV is represented by phlebotomy (Table 4), aiming at reaching and maintaining a target hematocrit level that is currently set at less than 45% in men and less than 42% in women, according to the Polycythemia Vera Study Group (PVSG) 01 trial. In high-risk patients, cytotoxic therapy should be instituted. Hydroxyurea (HU) is the drug of choice because of its effectiveness in reducing life-threatening cardiovascular events, and the lack of clear evidence for a leukemogenic potential of the drug. Low-dose aspirin (80–100 mg/die) is recommended in all PV patients, irrespective of the risk category (Table 4), in the absence of specific contra-indications. Use of aspirin is supported by results of the ECLAP study that enrolled 518 PV patients without clear indication or contraindication to aspirin in a double blind, placebo-controlled randomized trial of low-dose aspirin (100 mg daily) and followed for a mean of 2.8 years. The risk of combined primary endpoints (cardiovascular death, non-fatal myocardial infarction, non-fatal stroke and major venous thromboembolism) is significantly lowered in the aspirin group (relative risk 0.40; 95% CI, 0.18–0.91; P = 0.02); total and cardiovascular mortality are reduced of 46 and 59%, respectively. Moreover, low-dose aspirin does not increase the risk of major bleeding significantly.
In younger PV patients at high risk because of a previous thrombosis, in those who are low-risk but require therapy because of progressive myeloproliferation, or have cytogenetic abnormalities, or are resistant or intolerant to HU, an alternative is represented by interferon-alpha (IFN-α). In a recent French multicenter study of pegylated-IFNalpha-2a in 40 PV patients [48], 95% of the patients reach a complete hematological response, and during a median follow-up of 31 months, no thromboembolic event was recorded. Noteworthy, 90% of the patients show a progressive reduction in the percentage of mutated V617F allele in granulocytes, and in 7 of 29 patients, V617F mutated cells can no longer be demonstrated, consistent with complete molecular remission. Finally, in all PV patients, independent of their risk-category, identification and correction, whenever possible, of additional generic cardiovascular risk factors, particularly smoking habits, should be pursued.
Low-risk patients with asymptomatic ET do not need specific therapy, while aspirin is usually employed in those in the intermediate-risk category (Table 4), although in the absence of evidence-based data. On the other hand, aspirin is effective against symptoms attributable to microvascular disturbances; full doses of aspirin (up to 500 mg/die or even more) may be required for controlling pain in the acute phase of erythromelalgia or other disturbances of microvasculature, particularly migraine, and other neurological symptoms. Extreme thrombocytosis is considered a contraindication to aspirin for a supposedly greater risk of bleeding due to an acquired vonWillebrand disease, but formal proof is lacking. Aspirin should be employed with caution in association with anagrelide [22] due to the anti-aggregating properties of the drug.
The indications for treatment of high-risk ET patients are similar to PV (Table 4); the choice of HU is supported by two randomized studies. HU reduces the percentage of patients developing thrombosis from 24 to 3.6% among 148 high-risk ET patients randomized to hydroxyurea versus no treatment in the “Bergamo” trial [19]. Hydroxyurea is also superior to anagrelide in the randomized PT-1 trial, which enrolled 809 high-risk patients on the top of low-dose aspirin [22], and shows a protective effect against arterial thrombosis while the rate of venous thrombosis is lower in the anagrelide arm. The target level at which platelet count should be maintained with therapy in high-risk patients is not evidence-based; however, it is currently set at 400–450 × 109/L. Indications for interferon-alpha are substantially the same as for PV, in the lack of randomized studies comparing IFN-α with conventional therapies. Anagrelide, an imidazoquinazolin compound that reduces platelet number by inhibiting maturation of megakaryocytes, is currently approved as second-line treatment for ET in subjects who are intolerant to HU, or in whom platelet count does not reduce to target levels notwithstanding a full dose of HU. In the latter instance, association of HU with anagrelide might be worthwhile. Independent of the patient’s risk-category, identification and correction of generic cardiovascular risk factors should be addressed. Additional specific therapeutic issues, such as therapy in the pregnant woman with ET or PV, are discussed in recent reviews, such as [49]. Finally, there is great expectation for the results of therapy with novel molecularly targeted drugs that act as JAK2 inhibitors, although it must be realized that effects on the thrombotic tendency of MPN will require some time before they can be meaningfully evaluated [50].
References
Tefferi A, Thiele J, Orazi A, Kvasnicka HM, Barbui T, Hanson CA, Barosi G, Verstovsek S, Birgegard G, Mesa R, Reilly JT, Gisslinger H, Vannucchi AM, Cervantes F, Finazzi G, Hoffman R, Gilliland DG, Bloomfield CD, Vardiman JW (2007) Proposals and rationale for revision of the World Health Organization diagnostic criteria for polycythemia vera, essential thrombocythemia, and primary myelofibrosis: recommendations from an ad hoc international expert panel. Blood 110:1092–1097
Vannucchi AM, Guglielmelli P, Tefferi A (2009) Advances in understanding and management of myeloproliferative neoplasms. CA Cancer J Clin 59:171–191
Tefferi A (2008) The history of myeloproliferative disorders: before and after Dameshek. Leukemia 22:3–13
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Vardiman JW (ed) (2008) WHO classification of tumors of haematopoietic and lymphoid tissues. International Agency for Research on Cancer, Lyon
Rollison DE, Howlader N, Smith MT, Strom SS, Merritt WD, Ries LA, Edwards BK, List AF (2008) Epidemiology of Myelodysplastic Syndromes and Chronic Myeloproliferative Disorders in the United States, 2001–2004: utilizing Data from the NAACCR and SEER Programs. Blood 112:45–52
Barosi G, Mesa RA, Thiele J, Cervantes F, Campbell PJ, Verstovsek S, Dupriez B, Levine RL, Passamonti F, Gotlib J, Reilly JT, Vannucchi AM, Hanson CA, Solberg LA, Orazi A, Tefferi A (2008) Proposed criteria for the diagnosis of post-polycythemia vera and post-essential thrombocythemia myelofibrosis: a consensus statement from the international working group for myelofibrosis research and treatment. Leukemia 22:437–438
Levine RL, Pardanani A, Tefferi A, Gilliland DG (2007) Role of JAK2 in the pathogenesis and therapy of myeloproliferative disorders. Nat Rev Cancer 7:673–683
James C, Ugo V, Le Couedic JP, Staerk J, Delhommeau F, Lacout C, Garcon L, Raslova H, Berger R, Bennaceur-Griscelli A, Villeval JL, Constantinescu SN, Casadevall N, Vainchenker W (2005) A unique clonal JAK2 mutation leading to constitutive signalling causes polycythaemia vera. Nature 434:1144–1148
Kralovics R, Passamonti F, Buser AS, Teo SS, Tiedt R, Passweg JR, Tichelli A, Cazzola M, Skoda RC (2005) A gain-of-function mutation of JAK2 in myeloproliferative disorders. N Engl J Med 352:1779–1790
Levine RL, Wadleigh M, Cools J, Ebert BL, Wernig G, Huntly BJ, Boggon TJ, Wlodarska I, Clark JJ, Moore S, Adelsperger J, Koo S, Lee JC, Gabriel S, Mercher T, D’Andrea A, Frohling S, Dohner K, Marynen P, Vandenberghe P, Mesa RA, Tefferi A, Griffin JD, Eck MJ, Sellers WR, Meyerson M, Golub TR, Lee SJ, Gilliland DG (2005) Activating mutation in the tyrosine kinase JAK2 in polycythemia vera, essential thrombocythemia, and Myeloid Metaplasia with myelofibrosis. Cancer Cell 7:387–397
Scott LM, Tong W, Levine RL, Scott MA, Beer PA, Stratton MR, Futreal PA, Erber WN, McMullin MF, Harrison CN, Warren AJ, Gilliland DG, Lodish HF, Green AR (2007) JAK2 exon 12 mutations in polycythemia vera and idiopathic erythrocytosis. N Engl J Med 356:459–468
Pardanani AD, Levine RL, Lasho T, Pikman Y, Mesa RA, Wadleigh M, Steensma DP, Elliott MA, Wolanskyj AP, Hogan WJ, McClure RF, Litzow MR, Gilliland DG, Tefferi A (2006) MPL515 mutations in myeloproliferative and other myeloid disorders: a study of 1182 patients. Blood 108:3472–3476
Pikman Y, Lee BH, Mercher T, McDowell E, Ebert BL, Gozo M, Cuker A, Wernig G, Moore S, Galinsky I, DeAngelo DJ, Clark JJ, Lee SJ, Golub TR, Wadleigh M, Gilliland DG, Levine RL (2006) MPLW515L is a novel somatic activating mutation in myelofibrosis with myeloid metaplasia. PLoS Med 3:e270
Guglielmelli P, Pancrazzi A, Bergamaschi G, Rosti V, Villani L, Antonioli E, Bosi A, Barosi G, Vannucchi AM (2007) Anaemia characterises patients with myelofibrosis harbouring Mpl mutation. Br J Haematol 137:244–247
Vannucchi AM, Antonioli E, Guglielmelli P, Pancrazzi A, Guerini V, Barosi G, Ruggeri M, Specchia G, Lo Coco F, Delaini F, Villani L, Finotto S, Ammatuna E, Alterini R, Carrai V, Capaccioli G, Di Lollo S, Liso V, Rambaldi A, Bosi A, Barbui T (2008) Characteristics and clinical correlates of MPL 515 W > L/K mutation in essential thrombocythemia. Blood 112:844–847
Beer PA, Campbell P, Scott LM, Bench AJ, Erber WN, Bareford D, Wilkins B, Reilly JT, Hasselbalch HC, Bowman R, Wheatley K, Buck G, Harrison C, Green AR (2008) MPL mutations in myeloproliferative disorders: analysis of the PT-1 cohort. Blood 112:141–149
Delhommeau F, Dupont S, Della Valle V, James C, Trannoy S, Masse A, Kosmider O, Le Couedic JP, Robert F, Alberdi A, Lecluse Y, Plo I, Dreyfus FJ, Marzac C, Casadevall N, Lacombe C, Romana SP, Dessen P, Soulier J, Viguie F, Fontenay M, Vainchenker W, Bernard OA (2009) Mutation in TET2 in myeloid cancers. N Engl J Med 360:2289–2301
Vannucchi AM, Guglielmelli P (2008) Molecular pathophysiology of Philadelphia-negative myeloproliferative disorders: beyond JAK2 and MPL mutations. Haematologica 93:972–976
Cortelazzo S, Finazzi G, Ruggeri M, Vestri O, Galli M, Rodeghiero F, Barbui T (1995) Hydroxyurea for patients with essential thrombocythemia and a high risk of thrombosis. N Engl J Med 332:1132–1136
Landolfi R, Marchioli R, Kutti J, Gisslinger H, Tognoni G, Patrono C, Barbui T (2004) Efficacy and safety of low-dose aspirin in polycythemia vera. N Engl J Med 350:114–124
Marchioli R, Finazzi G, Landolfi R, Kutti J, Gisslinger H, Patrono C, Marilus R, Villegas A, Tognoni G, Barbui T (2005) Vascular and neoplastic risk in a large cohort of patients with polycythemia vera. J Clin Oncol 23:2224–2232
Harrison CN, Campbell PJ, Buck G, Wheatley K, East CL, Bareford D, Wilkins BS, van der Walt JD, Reilly JT, Grigg AP, Revell P, Woodcock BE, Green AR (2005) Hydroxyurea compared with anagrelide in high-risk essential thrombocythemia. N Engl J Med 353:33–45
De Stefano V, Za T, Rossi E, Vannucchi AM, Ruggeri M, Elli E, Mico C, Tieghi A, Cacciola RR, Santoro C, Gerli G, Vianelli N, Guglielmelli P, Pieri L, Scognamiglio F, Rodeghiero F, Pogliani EM, Finazzi G, Gugliotta L, Marchioli R, Leone G, Barbui T (2008) Recurrent thrombosis in patients with polycythemia vera and essential thrombocythemia: incidence, risk factors, and effect of treatments. Haematologica 93:372–380
Kiladjian JJ, Cervantes F, Leebeek FW, Marzac C, Cassinat B, Chevret S, Cazals-Hatem D, Plessier A, Garcia-Pagan JC, Murad SD, Raffa S, Janssen HL, Gardin C, Cereja S, Tonetti C, Giraudier S, Condat B, Casadevall N, Fenaux P, Valla DC (2008) The impact of JAK2 and MPL mutations on diagnosis and prognosis of splanchnic vein thrombosis: a report on 241 cases. Blood 111:4922–4929
Cervantes F, Passamonti F, Barosi G (2008) Life expectancy and prognostic factors in the classic BCR/ABL-negative myeloproliferative disorders. Leukemia 22:905–914
Finazzi G, Barbui T (2005) Risk-adapted therapy in essential thrombocythemia and polycythemia vera. Blood Rev 19:243–252
Marchetti M, Falanga A (2008) Leukocytosis, JAK2V617F mutation, and hemostasis in myeloproliferative disorders. Pathophysiol Haemost Thromb 36:148–159
Di Nisio M, Barbui T, Di Gennaro L, Borrelli G, Finazzi G, Landolfi R, Leone G, Marfisi R, Porreca E, Ruggeri M, Rutjes AW, Tognoni G, Vannucchi AM, Marchioli R (2007) The haematocrit and platelet target in polycythemia vera. Br J Haematol 136:249–259
Pearson TC, Wetherley-Mein G (1978) Vascular occlusive episodes and venous haematocrit in primary proliferative polycythaemia. Lancet 2:1219–1222
Tefferi A, Gangat N, Wolanskyj AP (2006) Management of extreme thrombocytosis in otherwise low-risk essential thrombocythemia; does number matter? Blood 108:2493–2494
Barbui T, Carobbio A, Rambaldi A, Finazzi G (2009) Perspectives on thrombosis in essential thrombocythemia and polycythemia vera: is leukocytosis a causative factor? Blood 114:759–763
Antonioli E, Guglielmelli P, Pancrazzi A, Bogani C, Verrucci M, Ponziani V, Longo G, Bosi A, Vannucchi AM (2005) Clinical implications of the JAK2 V617F mutation in essential thrombocythemia. Leukemia 19:1847–1849
Antonioli E, Guglielmelli P, Poli G, Bogani C, Pancrazzi A, Longo G, Ponziani V, Tozzi L, Pieri L, Santini V, Bosi A, Vannucchi AM (2008) Influence of JAK2V617F allele burden on phenotype in essential thrombocythemia. Haematologica 93:41–48
Wolanskyj AP, Lasho TL, Schwager SM, McClure RF, Wadleigh M, Lee SJ, Gilliland DG, Tefferi A (2005) JAK2 mutation in essential thrombocythaemia: clinical associations and long-term prognostic relevance. Br J Haematol 131:208–213
Vannucchi AM, Antonioli E, Guglielmelli P, Rambaldi A, Barosi G, Marchioli R, Marfisi RM, Finazzi G, Guerini V, Fabris F, Randi ML, De Stefano V, Caberlon S, Tafuri A, Ruggeri M, Specchia G, Liso V, Rossi E, Pogliani E, Gugliotta L, Bosi A, Barbui T (2007) Clinical profile of homozygous JAK2V617F mutation in patients with polycythemia vera or essential thrombocythemia. Blood 110:840–846
Vannucchi AM, Antonioli E, Guglielmelli P, Longo G, Pancrazzi A, Ponziani V, Bogani C, Ferrini PR, Rambaldi A, Guerini V, Bosi A, Barbui T (2007) Prospective identification of high-risk polycythemia vera patients based on JAK2(V617F) allele burden. Leukemia 21:1952–1959
Vannucchi AM, Antonioli E, Guglielmelli P, Pardanani A, Tefferi A (2008) Clinical correlates of JAK2V617F presence or allele burden in myeloproliferative neoplasms: a critical reappraisal. Leukemia 22:1299–1307
Ziakas PD (2008) Effect of JAK2 V617F on thrombotic risk in patients with essential thrombocythemia: measuring the uncertain. Haematologica 93:1412–1414
Dahabreh IJ, Zoi K, Giannouli S, Zoi C, Loukopoulos D, Voulgarelis M (2008) Is JAK2 V617F mutation more than a diagnostic index? A meta-analysis of clinical outcomes in essential thrombocythemia. Leuk Res 33:67–73
Lussana F, Caberlon S, Pagani C, Kamphuisen PW, Buller HR, Cattaneo M (2009) Association of V617F Jak2 mutation with the risk of thrombosis among patients with essential thrombocythaemia or idiopathic myelofibrosis: A systematic review. Thromb Res Mar 17 (epub ahead of print)
De Stefano V, Fiorini A, Rossi E, Za T, Farina G, Chiusolo P, Sica S, Leone G (2007) Incidence of the JAK2 V617F mutation among patients with splanchnic or cerebral venous thrombosis and without overt chronic myeloproliferative disorders. J Thromb Haemost 5:708–714
Dentali F, Squizzato A, Brivio L, Appio L, Campiotti L, Crowther M, Grandi AM, Ageno W (2009) JAK2V617F mutation for the early diagnosis of Ph- myeloproliferative neoplasms in patients with venous thromboembolism: a meta-analysis. Blood 113:5617–5623
Passamonti F, Rumi E, Pietra D, Della Porta MG, Boveri E, Pascutto C, Vanelli L, Arcaini L, Burcheri S, Malcovati L, Lazzarino M, Cazzola M (2006) Relation between JAK2 (V617F) mutation status, granulocyte activation, and constitutive mobilization of CD34 + cells into peripheral blood in myeloproliferative disorders. Blood 107:3676–3682
Falanga A, Marchetti M, Evangelista V, Vignoli A, Licini M, Balicco M, Manarini S, Finazzi G, Cerletti C, Barbui T (2000) Polymorphonuclear leukocyte activation and hemostasis in patients with essential thrombocythemia and polycythemia vera. Blood 96:4261–4266
Falanga A, Marchetti M, Vignoli A, Balducci D, Russo L, Guerini V, Barbui T (2007) V617F JAK-2 mutation in patients with essential thrombocythemia: relation to platelet, granulocyte, and plasma hemostatic and inflammatory molecules. Exp Hematol 35:702–711
Marchetti M, Castoldi E, Spronk HM, van Oerle R, Balducci D, Barbui T, Rosing J, Ten Cate H, Falanga A (2008) Thrombin generation and activated protein C resistance in patients with essential thrombocythemia and polycythemia vera. Blood 112:4061–4068
De Stefano V, Za T, Rossi E, Fiorini A, Ciminello A, Luzzi C, Chiusolo P, Sica S, Leone G (2009) Influence of the JAK2 V617F mutation and inherited thrombophilia on the thrombotic risk among patients with essential thrombocythemia. Haematologica 94:733–737
Kiladjian JJ, Cassinat B, Chevret S, Turlure P, Cambier N, Roussel M, Bellucci S, Grandchamp B, Chomienne C, Fenaux P (2008) Pegylated interferon-alfa-2a induces complete hematological and molecular responses with low toxicity in polycythemia vera. Blood 112:3065–3072
Barbui T, Finazzi G (2006) Myeloproliferative disease in pregnancy and other management issues. In: Hematology. American Society of Hematology Education Program, pp 246–252
Pardanani A (2008) JAK2 inhibitor therapy in myeloproliferative disorders: rationale, preclinical studies and ongoing clinical trials. Leukemia 22:23–30
Acknowledgments
This work was supported by Institutional Funds from University of Florence (ex-60%) and Istituto Toscano Tumori. The author apologizes to many eminent colleagues whose work in the field can not be cited because of space limitations.
Conflict of interest statement
The authors declare that they have no conflict of interest related to the publication of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vannucchi, A.M. Insights into the pathogenesis and management of thrombosis in polycythemia vera and essential thrombocythemia. Intern Emerg Med 5, 177–184 (2010). https://doi.org/10.1007/s11739-009-0319-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-009-0319-3