Abstract
Evidence supporting the safe use of the single-port (SP) robot for partial nephrectomy is scarce. The purpose of this study was to compare perioperative outcomes for patients undergoing robotic assisted SP vs multi-port (MP) partial nephrectomy (PN) in a time-matched cohort. All patients with clinically localized renal masses who underwent robotic PN from January 2019 to March 2020 were evaluated. Patients were stratified according to SP vs MP approach. Postoperative analgesia was administered in accordance with department-wide opioid stewardship protocol and outpatient opioid use was tracked. Total of 78 patients underwent robotic PN with 26 patients in the SP cohort. The majority of renal masses had low-complexity (53, 67.9%) R.E.N.A.L. nephrometry scores, without a significant difference between the two cohorts (p = 0.19). A retroperitoneal approach was performed in 16 (20.5%) patients overall, though more commonly via the SP robotic approach (13 vs 3, p < 0.001). Mean operative time for SP cases was 183.9 ± 63.5 min vs 208.6 ± 65.0 min in the MP cohort (p = 0.12). Rate of conversion to radical nephrectomy was 3.8% vs 9.6% for SP vs MP cases, respectively, (p = 0.37). The majority of patients were discharged on postoperative day one (67.9%) irrespective of operative approach (p = 0.60). There were no differences in inpatient milligram morphine equivalents administered (MME, p = 0.08) or outpatient postoperative MME prescribed (p = 0.21) between the two cohorts. In this retrospective single-institution study, SP robotic approach offers similar short-term perioperative outcomes to MP platforms for minimally invasive, nephron-sparing surgery. Using the SP system was not associated with a reduction in postoperative opioid analgesic requirements.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The American Cancer Society predicts an estimated 73,750 new cases of renal cell carcinoma (RCC) in the United States in 2020 [1]. The majority of newly discovered renal masses are clinically T1; thus, amenable to nephron-sparing extirpative approaches to preserve renal function [2, 3]. Since up to 20% of small renal masses are benign and open partial nephrectomy carries significant morbidity, the American Urological Association and European Association of Urology support a minimally invasive conventional laparoscopic or robot-assisted laparoscopic approach to minimize blood loss, perioperative pain, length of stay, and long-term convalescence [3, 4].
The da Vinci single-port (SP) robotic platform (Intuitive Surgical, Sunnyvale, CA) gained US Food and Drug Administration approval for urologic surgery in 2018 and permits true single-incision robotic surgery through a 2.5 cm, multichannel trocar [5, 6]. While several series have demonstrated comparable safety and oncologic efficacy between the SP and multi-port (MP) approach for radical prostatectomy, evidence in support of using this platform for nephron-sparing surgery is scarce [5,6,7,8,9,10,11,12]. Given the prevalence of intra- and perioperative complications reported for minimally invasive, nephron-sparing surgery, evaluation of the safety and efficacy of the SP robotic system for this procedure is of paramount importance [13,14,15].
The purpose of this study was to evaluate safety and postoperative opioid analgesic requirements in a contemporary cohort of adults undergoing partial nephrectomy (PN) for clinically localized renal masses comparing SP and MP robotic platforms.
Methods
Patient accrual and study design
All patients with clinically localized renal masses who underwent robotic PN from January 2019 to March 2020 at our institution were eligible for inclusion in this retrospective cohort comparison study. Preoperative demographic and clinical information, mass characteristics, postoperative course, and post-hospitalization opioid medication use were obtained via chart review under Institutional Review Board approval. Estimated blood loss (EBL) was stratified by greater or less than 500 mL to avoid challenges interpreting mean EBL which, can be skewed by select cases with blood loss drastically greater or less than the norm [16].
Preoperative cross-sectional imaging and radiology reports were used to calculate the R.E.N.A.L. (radius, endophytic/exophytic, nearness, anterior/posterior, location) nephrometry score [17]. Patients underwent either a MP (da Vinci Xi or Si, Intuitive Surgical, Sunnyvale, CA), or SP PN based on operating room availability. A transperitoneal (TP) or retroperitoneal (RP) approach was utilized based on tumor location, size, and surgeon preference. All MP PNs were performed by one of five fellowship-trained urologic oncologists with extensive multi-port robotic platform training and clinical experience. Two of those five urologic oncologists performed all SP procedures, and they preferentially utilized this platform if it was available. Both urologic oncologists have utilized the SP platform for minimally invasive procedures since it was first made available at our institution in 2019. Complications were recorded using the Clavien–Dindo classification system [18]. Final surgical pathology was reported according to 2016 World Health Organization/International Society of Urological Pathology classification [19]. Surgical margin positivity was not compared due to the controversial prognostic implications of this finding and the operative heterogeneity of enucleation and wedge resections across both cohorts [20, 21].
Surgical approach
For patients who underwent SP PN, the transperitoneal approach was performed by positioning patients in the modified flank position. A 3 cm midline incision above the umbilicus was made to accommodate a GelPort MINI (Applied Medical, Rancho Santa Margarita, CA), which in turn allowed for SP trocar and 12 mm AirSeal assistant port (ConMed Corp., Utica, NY) placement through a single incision. For anatomically challenging cases, a separate incision was made inferior to the xyphoid process or in the ipsilateral lower quadrant to accommodate an 8 or 12 mm AirSeal assistant port. The retroperitoneal approach was performed in a full flank position. The 3 cm horizontal incision for the GelPort MINI was made medial to the tip of the 12th rib. A separate assistant port was placed medially in line with the umbilicus after the retroperitoneal working space was bluntly developed if needed (Fig. 1).
Port configuration for SP robotic retroperitoneal (a) and transperitoneal (b) partial nephrectomy. The retroperitoneal approach is conducted in a formal flank position and the transperitoneal approach is achieved in a modified flank position. Both SP approaches utilize a 3 cm single incision to accommodate the robotic arm and AirSeal port. A separate 1 cm incision for an AirSeal assistant port for challenging cases is possible
The transperitoneal MP PN was performed in the modified flank position in the traditional manner by placing three 8 mm trocars and an 8 mm (Xi) or 12 mm (Si) camera port linearly along the midclavicular line on the ipsilateral side of the tumor. The AirSeal assistant port was placed superior to the umbilicus. For the retroperitoneal MP approach, patients were placed in formal flank position. Retroperitoneal access was achieved by making a 1–1.5 cm incision two fingerbreadths below the midpoint between the 11th and 12th ribs. A Spacemaker balloon (Medtronic, Minneapolis, MN) was used to develop the retroperitoneal working space. The initial incision served as the camera port and three additional 8 mm working ports were placed in line with the camera port and the umbilicus. An additional 12 mm AirSeal port was placed inferior to the camera port.
All patients received 5000 u heparin and antibiotics preoperatively. Hilar exposure was performed in all cases but decision to clamp the renal artery and/or vein prior to tumor extirpation and renorrhaphy was made based on surgeon preference. The two surgeons performing SP as well as some MP PNs favored ‘off-clamp’ tumor extirpation whereas the other three surgeons performing MP-only PN’s performed hilar clamping routinely. The two SP surgeons have 7- and 9-year post-fellowship operative experience, one MP surgeon has 13-year experience and the other two MP surgeons each have greater than 1-year post-fellowship operating experience. The decision to leave a perinephric drain postoperatively was based on surgeon preference and case complexity. All patients were continued on prophylactic heparin or enoxaparin while admitted.
Postoperative opioid management
Baseline opioid use was defined as filling an opioid narcotic prescription within 3 months of surgery according to the Alabama Prescription Drug Monitoring Program (AL-PDMP), which reports opioid prescriptions nationwide. Postoperative analgesia was managed in accordance with department-wide opioid conservation efforts: unless contraindicated, all patients receive scheduled acetaminophen. A low (5 mg) and moderate dose (10 mg) oral opioid narcotic (oxycodone or hydrocodone) were available. For patients with persistent intolerable pain, non-narcotic analgesics such as muscle relaxers (i.e., methocarbamol) and/or neuralgesics (i.e., gabapentin) were administered prior to any additional oral or intravenous opioids. Inpatient analgesic administration was dictated by self-reported pain severity from 0 to 10. Mild pain (1–3) was managed by oral acetaminophen, moderate pain (4–6) with a 5 mg oral opioid, severe pain (7–10) with a 10 mg oral opioid and persistent or breakthrough pain with muscle relaxers, neuralgesics or intravenous opioids as a last resort. Upon discharge, all patients are instructed to take alternating doses of acetaminophen and ibuprofen prior opioid use. Patients are prescribed no more than 8 5 mg oxycodone or 14 5/325 mg oxycodone/acetaminophen tablets (if ibuprofen is medically contraindicated) following surgery. Additional measures such as transverse abdominis plane blocks were not routinely used.
The AL-PDMP was reviewed to identify opioid prescriptions filled postoperatively. Additional opioid prescriptions were defined as any additional opioid prescription filled within 3 months of surgery. Milligram morphine equivalents (MMEs) were calculated for all inpatient and outpatient opioid use for standardization [22, 23].
Statistical analysis
Statistical analysis was performed using Stata SE v12.1 software (College Station, TX, USA). Group categorical and continuous variables were compared using χ2 and t tests, respectively. Fischer exact modifications were made for the χ2 test in situations where frequency of a categorical variable necessitated adjustment. A p value less than 0.05 was considered statistically significant.
Results
From January 2019 to March 2020, 78 patients underwent robotic PN. Among these, 26 (33.3%) were performed using the SP platform. No significant differences in average age, BMI, gender, ECOG performance status, or history of prior abdominal surgery between the two cohorts were observed. Baseline opioid use was present in 24 (30.8%) of all patients, and this was not significantly different between the two cohorts. Additional preoperative information is summarized in Table 1.
The majority of all renal masses were cT1a (52, 66.7%) without a laterality predominance (p = 0.34). Most masses were low- (53, 67.9%) or moderate-risk (23, 29.5%) for perioperative complications according to R.E.N.A.L. nephrometry score calculations. These factors did not significantly differ when stratified by SP vs MP approach (Table 2). No significant difference in mean tumor size between the SP and MP cohorts was observed (3.5 ± 1.3 cm vs 3.3 ± 1.6 cm, respectively, p = 0.55). A greater proportion of SP cases involved posterior or mid-axis tumors compared to MP cases (20, 76.9% vs 33, 63.5%) but this was not statistically significant (p = 0.48).
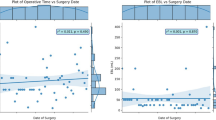
Significantly more SP cases were performed ‘off-clamp’ (24/26 or 92%) whereas hilar clamping was utilized for 32/52 (61.5%) of the MP cohort (p < 0.001). A retroperitoneal approach was performed in 13 (50%) and 3 (5.8%) SP and MP cases, respectively (p < 0.001). Mean operative time for all patients was 190 min. No significant difference were observed when stratified by SP vs MP approach (183.9 ± 63.5 min vs 208.6 ± 65.0 min, p = 0.12). A separate AirSeal port was utilized in 16 (61.5%) SP cases. Using a separate assistant port did not impact mean SP case operative time (p = 0.73).
While occurring at a higher relative incidence in the SP cohort, episodes of EBL > 500 mL did not significantly differ between the SP (8, 30.8%) and MP cohorts (8, 15.4%, p = 0.11). Transfusion requirement was overall higher in the SP cohort (3/26 vs 1/52) but not statistically significant (p = 0.07). Subgroup analysis revealed incidence of EBL > 500 mL did not significantly differ in the setting of hilar clamping (p = 0.98) or according to transperitoneal vs retroperitoneal approach (p = 0.62). Significant EBL did not significantly differ when stratified by use of a separate assistant port in the SP cohort (p = 0.95). Six patients required conversion to radical nephrectomy in the entire study, with no significant difference between the SP and MP cohorts (1 vs 5, p = 0.37).
There were six observed complications in the entire cohort: two Clavien–Dindo II complications, three Clavien–Dindo III and one Clavien–Dindo IV. The three Clavien–Dindo III complications were postoperatively discovered collecting system injuries necessitating ureteral stent placement (two SP, one MP, p = 0.21). The Clavien–Dindo IV complication in the MP cohort was a postoperative cerebrovascular accident. The overall incidence of complications did not differ between the two cohorts (p = 1.0). Additional intraoperative information is outlined in Table 3.
Most patients were discharged on postoperative day one (53, 67.9%), and overall length of stay did not significantly differ between the two cohorts (p = 0.60). Mean postoperative inpatient MME was not significantly different between the SP and MP cohorts although there was a trend towards lower MME administration in the SP arm (63.1 vs 95.8 MME, p = 0.08).
Nearly all patients were prescribed an opioid pain medication at discharge (73, 93.6%), and 62 (79.5%) filled their prescription. Ten opioid pills were prescribed on average, and this did not significantly differ between SP and MP cohorts (p = 0.17, Table 3). There were a significantly higher number of MP patients who received a non-narcotic analgesic prescription (24, 46.2%) compared to SP patients (6, 23.1%, p = 0.041). Operative time, EBL, complication occurrence, conversion to radical nephrectomy and length of stay were not significantly associated with being prescribed a non-narcotic analgesic prescription on univariate analyses.
Mean overall perioperative opioid use (inpatient + prescribed) was 207.7MME, and while lower in the SP cohort (149.0 vs 235.0MME) this was not statistically significant (p = 0.20). There was a nonsignificant but lower mean MME prescribed postoperatively in the SP cohort (60.1 vs 85.7 MME p = 0.21), and fewer SP patients required an additional opioid (11.5% vs 21.2%, p = 0.24, Table 3). Total perioperative MME did not significantly differ between the SP and MP cohorts when further stratified according to gender, transperitoneal or retroperitoneal approach (p > 0.05 for all subgroups). Use of an assistant port was not significantly associated with total perioperative MME requirements for SP cases (p = 0.25).
Final surgical pathology revealed RCC in 71/78 cases. Clear cell RCC (ccRCC) and papillary RCC (papRCC) were among the most common RCC subtypes (44, 62.0% and 16, 22.5%, respectively). A total of 45 (63.4%) tumors were pT1a, 13 (18.3%) were pT1b, and 11 (15.5%) were pT3a. Regional node dissections were not performed in accordance with society guidelines and thus were pNX in all cases. The incidence of benign vs malignant neoplasms, various RCC subtypes as well as pT-stage did not significantly differ between the SP and MP cohorts (Table 2).
Discussion
Single-site robotic assisted partial nephrectomy was first described by Kaouk et al. in 2009 using a multichannel gelport to accommodate a MP robot [24]. While safe and efficacious for small exophytic tumors in several multi-institutional series, trocar setup and hilar control can be challenging [12, 24,25,26]. Early evidence suggest the SP platform is safe for radical prostatectomy, but only few studies have evaluated perioperative outcomes for partial nephrectomy. Our initial experience demonstrated feasibility of performing an off-clamp SP PN and radical nephrectomy [10]. Na et al. recently described 14 patients undergoing either SP or MP PN, and no significant complications were observed perioperatively [8,9,10,11]. To our knowledge, the present 78 patient study is the largest comparing SP vs MP PN and the largest retroperitoneal SP PN cohort reported to date.
Using the da Vinci SP platform to perform a PN via a transperitoneal and retroperitoneal approach appears safe and well tolerated in the present study. The incidence of conversion to radical nephrectomy and postoperative complications were overall low and did not differ significantly between the two cohorts. While the higher incidence of EBL > 500 mL and rate of blood transfusion in the SP cohort is worth noting, these differences were not statistically significant and may reflect ‘on-’ vs ‘off-clamp’ preferences, patient and/or perioperative factors not tracked in this study.
Though not statistically significant, the SP robotic system yielded a lower mean operative time despite our surgeons having vastly greater experience with the Si and Xi platforms. This is likely multifactorial and may reflect fewer required port sites for the SP platform, ease of docking and potentially lowered learning curve for experienced robotic surgeons. This shorter operative time may be especially advantageous for a retroperitoneal approach using the SP robot given the challenges associated with developing an adequate working space to accommodate multiple ports required for MP platforms [26,27,28]. This could be evidenced by the significantly higher rate of retroperitoneal PN performed in the SP cohort compared to the MP cohort in our study series.
In 2016, there were more than 2 million Americans with an opioid use disorder. Narcotic prescriptions as short as 6 days are associated with an increased risk of opioid dependence [29]. Resultantly, postoperative pain minimization and opioid stewardship have become increasingly important goals. Vigneswaran et al. recently evaluated 163 men who underwent SP or MP radical prostatectomy. Postoperative pain scores were significantly lower in the SP arm; however, no differences in total inpatient MME were observed [5]. While we similarly did not observe a significant decline in perioperative MME, mean total opioid administration (149.0 vs 235.0 MME, p = 0.20) and percent of patients requiring an additional opioid were insignificantly lower in the SP cohort (Table 3). This may be spurious or could reflect lower postoperative pain. Alternatively, recently implemented opioid stewardship efforts may have a greater impact on perioperative MME requirements than incisional size. While a significantly higher proportion of patients in the MP arm received a non-narcotic analgesic prescription, this discrepancy may not reflect patients’ true home medication regimens as all patients received written instructions to take acetaminophen and ibuprofen.
Our study has several acknowledged limitations. This was a retrospective, single-institution study. Selection bias influencing the use of SP vs MP platform as well as a transperitoneal vs retroperitoneal approach may have occurred. Operative time and EBL were derived from anesthetic records and other perioperative documents which are subject to error. While this represents the largest SP PN cohort to date, this is an admittedly small sample size lacking long-term oncologic follow-up and renal function monitoring. Intraoperative details such as the need to convert to radical nephrectomy and postoperative outcome including narcotic use may also reflect individual provider experience and counseling not captured in the present study.
Future studies with a larger and thus optimally powered sample size may further stratify patients according to transperitoneal and retroperitoneal approaches and better elucidate explanations for EBL discrepancies observed. Future studies may also assess the incidence of placing a second assistant port as well as any varying perioperative factors such as EBL and operative time as they may relate to the decision to perform ‘on- ’ vs ‘off-clamp’ extirpation. While introduction of a bulldog clamp without a dedicated 12 mm assistant port is feasible, it can be challenging and thus less desirable [12, 30]. Subsequent studies with long-term oncologic follow-up may also compare any prognostic implications of margin positivity in SP vs MP patient cohorts, as this finding on final surgical pathology remains controversial [31].
While postoperative opioid analgesia was only provided if patients met aforementioned criteria, objective 0–10 pain scores were not tracked for statistical analysis as the timing of acquisition as well as the temporal relationship to analgesic administration was not standardized. Similarly, surveying patients following discharge to quantify the number of opioid doses consumed may be an optimal modality to compare pain. Due to the large geographic area served by our institution, postoperative complications may have been addressed by other hospitals and thus not captured.
Conclusion
In this retrospective cohort study, the da Vinci SP platform offers similar perioperative and immediate postoperative outcomes to MP platforms for minimally invasive nephron-sparing surgery. When compared to traditional multi-port platforms, the SP platform did not appear to significantly reduce postoperative opioid analgesic requirements.
Data availability
Available upon request.
Code availability
Not applicable.
References
Siegel RL, Miller KD, Jemal A (2020) Cancer statistics, 2020. CA Cancer J Clin 70:7–30
Sc C, Br L (2016) Campbell-Walsh urology, ch 57: malignant renal tumors, 11th edn. Elsevier, Philidelphia, PA
Campbell S, Uzzo RG, Allaf ME et al (2017) Renal mass and localized renal cancer: AUA guideline. J Urol 198:520–529
Ljungberg B, Albiges L, Abu-Ghanem Y et al (2019) European association of urology guidelines on renal cell carcinoma: the 2019 update. Eur Urol 75:799–810
Vigneswaran HT, Schwarzman LS, Francavilla S et al (2020) A comparison of perioperative outcomes between single-port and multiport robot-assisted laparoscopic prostatectomy. Eur Urol 77:671
Bertolo R, Garisto J, Gettman M et al (2018) Novel system for robotic single-port surgery: feasibility and state of the art in urology. Eur Urol Focus 4:669–673
Saidian A, Fang AM, Hakim O et al (2020) Perioperative outcomes of single vs multi-port robotic assisted radical prostatectomy: a single institutional experience. J Urol 204:490–495
Saidian A, Fang AM, Hakim O et al (2020) Perioperative outcomes between single-port and multi-port robotic assisted radical prostatectomy: a single institutional experience. J Urol. https://doi.org/10.1097/JU0000000000000811
Kaouk J, Aminsharifi A, Sawczyn G et al (2020) Single-port robotic urological surgery using purpose-built single-port surgical system: single-institutional experience with the first 100 cases. Urology 140:77
Fang AM, Saidian A, Magi-Galluzzi C et al (2020) Single-port robotic partial and radical nephrectomies for renal cortical tumors: initial clinical experience. J Robot Surg 14:773
Na JC, Lee HH, Yoon YE et al (2020) True single-site partial nephrectomy using the SP surgical system: feasibility, comparison with the Xi single-site platform, and step-by-step procedure guide. J Endourol 34:169–174
Kaouk J, Garisto J, Eltemamy M et al (2019) Pure single-site robot-assisted partial nephrectomy using the SP surgical system: initial clinical experience. Urology 124:282–285
Khene ZE, Peyronnet B, Bernhard JC et al (2019) A preoperative nomogram to predict major complications after robot assisted partial nephrectomy (UroCCR-57 study). Urol Oncol 37(577):e1–e7
Bradshaw AW, Autorino R, Simone G et al (2020) Robotic partial nephrectomy versus minimally invasive radical nephrectomy for clinical T2a renal mass: a propensity score matched comparison from the ROSULA (robotic surgery for large renal mass) collaborative group. BJU Int 126:114
Bjurlin MA, Taneja SS (2001) Complications of urologic surgery: prevention and management, Ch. 34 complications of laparoscopic/robotic nephrectomy and partial nephrectomy, 4th edn. Elsevier, Philadelphia, PA
Rais-Bahrami S, George AK, Herati AS et al (2012) Off-clamp versus complete hilar control laparoscopic partial nephrectomy: comparison by clinical stage. BJU Int 109:1376–1381
Kutikov A, Uzzo RG (2009) The R.E.N.A.L. nephrometry score: a comprehensive standardized system for quantitating renal tumor size, location and depth. J Urol 182:844–853
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Moch H, Cubilla AL, Humphrey PA et al (2016) The 2016 WHO classification of tumours of the urinary system and male genital organs-part a: renal, penile, and testicular tumours. Eur Urol 70:93–105
Laganosky DD, Filson CP, Master VA (2017) Surgical margins in nephron-sparing surgery for renal cell carcinoma. Curr Urol Rep 18:8
Wang L, Hughes I, Snarskis C et al (2017) Tumor enucleation specimens of small renal tumors more frequently have a positive surgical margin than partial nephrectomy specimens, but this is not associated with local tumor recurrence. Virchows Arch 470:55–61
Motov S. MD Calc: Morphine milligram equivalents (MME) calculator. www.MDCalc.com
Dunn KM, Saunders KW, Rutter CM et al (2010) Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med 152:85–92
Kaouk JH, Goel RK (2009) Single-port laparoscopic and robotic partial nephrectomy. Eur Urol 55:1163–1169
Springer C, Greco F, Autorino R et al (2014) Analysis of oncological outcomes and renal function after laparoendoscopic single-site (LESS) partial nephrectomy: a multi-institutional outcome analysis. BJU Int 113:266–274
Greco F, Autorino R, Rha KH et al (2013) Laparoendoscopic single-site partial nephrectomy: a multi-institutional outcome analysis. Eur Urol 64:314–322
Pavan N, Derweesh I, Hampton LJ et al (2018) Retroperitoneal robotic partial nephrectomy: systematic review and cumulative analysis of comparative outcomes. J Endourol 32:591–596
Ghani KR, Porter J, Menon M et al (2014) Robotic retroperitoneal partial nephrectomy: a step-by-step guide. BJU Int 114:311–313
Zhu W, Chernew ME, Sherry TB et al (2019) Initial opioid prescriptions among U.S. commercially insured patients, 2012–2017. N Engl J Med 380:1043–1052
Shumaker L, Rais-Bahrami S, Nix J (2020) Renal hilar clamping with a standard robotic bulldog clamp using the single port da Vinci robot. Urology 145:297
Stewart GD, Oades G (2015) Frozen section during partial nephrectomy: an unreliable test that changes nothing? BJU Int 116:836–837
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
ZAG: conceptualization, data curation, formal analysis, investigation, methodology, resources, validation, visualization, writing—original draft, and writing—review and editing. ZRB: conceptualization, data curation, investigation, resources, and writing—review and editing. AMF: conceptualization, data curation, investigation, resources, and writing—review and editing. AS: conceptualization, data curation, investigation, resources, and writing—review and editing. CM-G: data curation, investigation, resources, and writing—review and editing. JWN: data curation, funding acquisition, supervision, validation, visualization, and writing—review and editing. SR-B: conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, resources, software, supervision, validation, visualization, writing—original draft, and writing—review and editing.
Corresponding author
Ethics declarations
Conflict of interest
Jeffrey W. Nix and Soroush Rais-Bahrami serve as consultants to Philips/InVivo Corp and Intuitive Surgical. Soroush Rais-Bahrami also serves as a consultant to Blue Earth Diagnostics, Genomic Health Inc, and Bayer Healthcare.
Consent for publication
All the authors approve of the submission of this manuscript for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Glaser, Z.A., Burns, Z.R., Fang, A.M. et al. Single- versus multi-port robotic partial nephrectomy: a comparative analysis of perioperative outcomes and analgesic requirements. J Robotic Surg 16, 695–703 (2022). https://doi.org/10.1007/s11701-021-01271-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-021-01271-y