Abstract
No data exists concerning the application of a new robotic system with 3-mm instruments (Senhance™, Transenterix, Milano, Italy) in small cavities. Therefore, the aim of this study was to test the system for its performance of intracorporal suturing in small boxes simulating small body cavities. Translucent plastic boxes of decreasing volumes (2519–90 ml) were used. The procedures (two single stitches, each with two consecutive surgical square knots) were performed by a system-experienced and three system-inexperienced surgeons in each box, starting within the largest box, consecutively exchanging the boxes into smaller ones. With this approach, the total amount of procedures performed by each surgeon increased with decreasing volume of boxes being operated in. Outcomes included port placement, time, task completion, internal and external instrument/instrument collisions and instrument/box collisions. The procedures could be performed in all boxes. The operating time decreased gradually in the first three boxes (2519–853 ml), demonstrating a learning curve. The increase of operating time from boxes of 599 ml and lower may be attributed to the increased complexity of the procedure in small cavities as in the smallest box with the dimensions of 2.9 × 6.3 × 4.9 cm. This is also reflected by the parallel increase of internal instrument–instrument collisions. With the introduction of 3-mm instruments in a new robotic surgical system, we were able to perform intracorporal suturing and knot tying in cavities as small as 90 ml. Whether this system is comparable to conventional three-port 3-mm laparoscopic surgery in small cavities—such as in pediatric surgery—has to be evaluated in further studies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In pediatric surgery, many procedures are restricted by the limited working space of the small abdominal and thoracic cavity, encumbering even 3-mm instrument three-port minimally invasive surgery [1]. Robotic surgery may, therefore, be beneficial, especially for complex tasks such as intracorporal suturing. However, the size of the instruments (5 and 8 mm) of the only system currently approved for the use in pediatric surgery (da Vinci™, Intuitive Surgical) limits its application in small children [2,3,4,5,6,7,8].
With a new robotic system (Senhance™, Transenterix) including 3-mm instruments, procedures might probably be executed in smaller children, such as neonates. But no data exist concerning its technical feasibility in small cavities. Therefore, the aim of this study was to test the Senhance™ system for its ability to perform intracorporal suturing in boxes of small volume with the intention to simulate procedures in small pediatric cavities.
Materials and methods
The study was conducted in the operating suite of the University Medical Center Hamburg-Eppendorf (UKE) where an installed system was readily available. The setup consisted of the master console and three separate arms with a 10-mm 3D 0° videoscope and two 3-mm needle drivers. This study was performed in plastic boxes without any patients or animals, thus IRB approval was not needed; the operating surgeons (Bergholz, Boettcher, Gidaro and Verweij) gave informed consent into the study, its evaluation and publication.
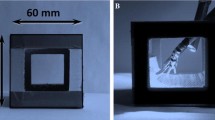
Translucent plastic boxes were used as operative cavities. The boxes were measured and their volume recorded (width × height × length or circular area (calculated from the width) × height in conical boxes). The boxes were screwed onto a wooden plate and the plate fastened on a standard operating table (Maquet, Germany) to keep it in place while tilting the table for better access and triangulation of the instruments. A leather patch was fixed to the wooden plate covering the open boxes to simulate the abdominal wall, which is used by the system to calibrate the fulcrum point for the instruments. The instruments were inserted without ports via stab incisions through the leather covering (Fig. 1).
The procedures were started in the largest box. After completion, the box was exchanged into a smaller one to gradually decrease the volume of the simulated cavity (Table 1). With decreasing size and, therefore, increasing amount of boxes having operated in, the total amount of procedures performed by each surgeon increased.
The procedures (two single stitches, each with two consecutive surgical square knots) were performed by a Senhance™-experienced adult surgeon (S. Gidaro) and three Senhance™-inexperienced pediatric surgeons (R. Bergholz, M. Boettcher and J. Verweij). The sutures were placed on a leather patch with marked spots for the stitches. The leather patch was fastened into each box accordingly. A Vicryl 5-0 suture with a TF-1 needle (Ethicon, Germany) was used. The position of the instruments and the length of the suture were adapted according to the available operative space. Any knot other than a surgical square knot or stitches more than 3 mm outside the marked spots in the leather patch were counted as “inability to perform the procedure”. The time for completion of each stitch and corresponding knots was taken. Every surgeon performed two stitches with corresponding knots per box, therefore, the minimum, maximum, median (if applicable) and mean time per box and surgeon as well as per group (experienced versus inexperienced Senhance™ surgeons) could be calculated.
All procedures were video-recorded for later blinded analysis. Outcome parameters were: completion of the task (yes, no), operating time (s), amount of internal instrument–instrument collisions (n), amount of external instrument–instrument collisions (n), amount of instrument–box collisions (n) and distance between the instruments (in cm, ΔLC: distance of the instrument to camera, ΔRC and ΔLR, respectively).
The operating time was plotted against the decreasing volume of the boxes on the X-axis. This allows for displaying two results: first, the operating time can be compared to the decreasing volume of the boxes (simulated cavities) and second, as the amount of procedures per surgeon increased as more (and smaller) boxes were operated in, the operating time can be understood as a learning curve for each surgeon confounded by the decreasing volume of the boxes. The Mann–Whitney U test was used to test for differences in skewed data.
Results
Internal instrument/instrument and instrument/box collisions increased within smaller boxes but did not impede the completion of the procedures in any of the boxes (Table 2). For instrument triangulation in the smallest box, the distance between the instruments could be reduced to 2.5 cm (camera to left and right instrument) and 3.8 cm (instrument to instrument, Table 3).
Figure 2a displays the mean operating time per group (experienced versus inexperienced Senhance™ surgeons) in relation to decreasing box volume. The operating time decreases gradually in the first three boxes. An increase was seen starting at a volume of 598 ml and smaller. This effect was more pronounced in the inexperienced surgeons than in the experienced surgeon and also apparent when displaying the best operating time (minimum operating time, Fig. 2b). The box plots of the operating time in the largest and smallest box did not show a significant difference in either group (p = 0.337 Senhance-inexperienced surgeons, p = 0.121 Senhance-experienced surgeon) or when analysing all surgeons collectively (p = 0.248, Fig. 2c, d).
a Mean operating time in seconds (single stitch with two consecutive intracorporal square knots) in the boxes grouped according to the Senhance experience oft the surgeons. b Minimum operating time in seconds according to a. c Box plot of the operating time grouped into Senhance-experienced and inexperienced surgeons between the largest and smallest box. Note that n = 2 in the Senhance-experienced group (one surgeon, two stitches with consecutive knots each) with, therefore, decreased statistical power. d Box pot of the operating time of all surgeons between the largest and smallest box
Discussion
Our results demonstrate that intracorporal suturing and knot tying are feasible in operative cavities as small as 90 ml by applying the Senhance™ system with a 10-mm 0° 3D laparoscope and two 3-mm instruments. The encountered instrument/instrument and instrument/box collisions in smaller boxes did not prevent the surgeons from completing the procedures in all settings. This is also confirmed by the operating time, which did not differ significantly between the biggest and smallest box (Fig. 2c, d). These results are in contrast to data on the only system currently approved for children, which demonstrates significant instrument/instrument or instrument/box collisions within cubes measuring 4.0 and 4.5 cm (64 ml and 91 ml, respectively) preventing surgeons from performing the procedures. With difficulty, suturing procedures could be performed in cubes of 5 and 6 cm size (125 and 216 ml) [5].
The advantage of this system in smaller cavities appears to be related to the use of smaller instruments which could be inserted directly without ports; they can, therefore, be placed closer together. The minimal horizontal area of 6.3 × 4.9 cm in the smallest box led to positioning of the instruments with a distance as short as 2.5 cm in this study [4, 9]. The small instrument distance may also be attributed to the configuration of the robotic arms outside the patient. Their range of motion is reduced when they are placed close to each other and the risk of external instrument/instrument collision increases. The Senhance applies three separate arms, each mounted on its own robotic slave console, providing a flexible 360° range of placement.
We encountered a learning curve, demonstrated by a decrease in operating time of the surgeons in the first six procedures [from box 1 (2519 ml) to box 3 (853 ml) times two procedures per box]. The learning curve in this study is in context to previously described short learning curves with the same system [10, 11]. The increase of operating time from boxes of 599 ml and lower, counteracting the learning curve, may be due to the increased complexity of the procedure in small cavities as knot tying became more demanding. This is also reflected by the increase of internal instrument–instrument collisions. Similar effects of multiphasic learning curves have been described for robotic adult surgery in rectal cancer with the da Vinci system [12].
It might be a matter of debate, that our setup did not include wristed instruments, as they are held to be one of the main advantages of robotic surgery [13]. But our study was conducted to test the general feasibility of the Senhance system in small cavities. Interestingly, as we were able to demonstrate that 3-mm instruments appear to provide access to and maneuverability in small cavities, our results are in contrast to a current study on the da Vinci system, comparing tasks with 5-mm and 8-mm instruments in a box with the dimensions of 6 × 6 × 6 cm (216 ml). The authors concluded that 8-mm robotic instruments are safer and more efficient tools for robotic surgery in small workspaces. Although 5-mm instruments should theoretically be more appropriate for use with pediatric patients, [their] study has shown conversely that they can be less effective due to a space-consuming effect [6]. This effect can be explained by the technically reduced joint angulation kinematics of the 5-mm compared to the 8-mm instruments in this system. In our study, we applied 3-mm non-articulating instruments, therefore, eliminating a probable confounding effect of wristed instruments.
As a potential interference, our setup required a 10-mm laparoscope for 3D vision. Of course, a 10-mm camera is cumbersome in pediatric newborn surgery. A 5-mm or 3-mm laparoscope can be applied instead, but would result in the loss of 3D visualization. Nevertheless, we hypothesize that advances in optical technics will lead to a size reduction of 3D laparoscopes down to 5 mm in the near future.
Due to its restriction in small cavities, current robotic surgery is performed in older children and adults, although it has been successfully applied in children with less than 10 kg body weight [14,15,16]. In a recent meta-analysis, the average age of pediatric patients was 7.8 years and the average weight 24.2 kg indicating its reduced feasibility in smaller children [4]. In contrast, robotic pediatric surgery may develop its full potential in complex procedures in small children and neonates, such as congenital diaphragmatic hernia repair, Kasai portoenterostomy, choledochal cyst excision, esophageal atresia repair or lung resections for CPAM [17]. Thus, a robotic system is required which is in small cavities equivalent applicable to laparoscopic or thoracoscopic surgery. For thoracoscopic esophageal atresia repair, the distance between instruments can be as short as 2.3 cm and 2.9 cm for camera to left and right and 4.7 cm for left to right instrument distance [18]. This distance was also realized in our study. Nevertheless, it appears to be a matter of debate how far the working space of 90 ml in our smallest box is similar to the working space in newborns and infants. For correction of esophageal atresia, the system has to be used inside the right hemithorax of newborns. Chapman et al. estimated the volume of the right lung by echo planar imaging within ranges from 74 to 114 ml in an infant with a body weight of 4 kg [19]. Therefore, our smallest box of 90 ml volume appears to be representative for a neonatal hemithorax.
Conclusion
Access to small body cavities, especially in small infants and neonates, is difficult with current robotic systems when providing 8–5 mm diameter instruments. With the introduction of 3-mm instruments into the Senhance system, we were able to perform intracorporal suturing and knot tying in cavities as small as 90 ml—simulating a neonatal hemithorax. Whether this system is comparable to or advantageous over conventional three port laparoscopic pediatric surgery is not known. Therefore, studies comparing the Senhance to experienced laparoscopic surgeons using standard 3-mm instruments have to be performed in small cavities to obtain reliable data.
References
Lacher M, Kuebler JF, Dingemann J, Ure BM (2014) Minimal invasive surgery in the newborn: current status and evidence. Semin Pediatr Surg 23:249–256. https://doi.org/10.1053/j.sempedsurg.2014.09.004
Spinoit A-F, Nguyen H, Subramaniam R (2017) Role of robotics in children: a brave new world! Eur Urol Focus 3:172–180. https://doi.org/10.1016/j.euf.2017.08.011
Cave J, Clarke S (2018) Paediatric robotic surgery. Ann R Coll Surg Engl 100:18–21. https://doi.org/10.1308/rcsann.supp2.18
van Haasteren G, Levine S, Hayes W (2009) Pediatric robotic surgery: early assessment. Pediatrics 124:1642–1649. https://doi.org/10.1542/peds.2008-3822
Thakre AA, Bailly Y, Sun LW, Van Meer F, Yeung CK (2008) Is smaller workspace a limitation for robot performance in laparoscopy? J Urol 179:1138–1142. https://doi.org/10.1016/j.juro.2007.10.091(discussion 1142–1143)
Ballouhey Q, Clermidi P, Cros J, Grosos C, Rosa-Arsène C, Bahans C, Caire F, Longis B, Compagnon R, Fourcade L (2018) Comparison of 8 and 5 mm robotic instruments in small cavities : 5 or 8 mm robotic instruments for small cavities? Surg Endosc 32:1027–1034. https://doi.org/10.1007/s00464-017-5781-9
Baek M, Silay MS, Au JK, Huang GO, Elizondo RA, Puttmann KT, Janzen NK, Seth A, Roth DR, Koh CJ (2018) Does the use of 5 mm instruments affect the outcomes of robot-assisted laparoscopic pyeloplasty in smaller working spaces? A comparative analysis of infants and older children. J Pediatr Urol. https://doi.org/10.1016/j.jpurol.2018.06.010
Finkelstein JB, Levy AC, Silva MV, Murray L, Delaney C, Casale P (2015) How to decide which infant can have robotic surgery? Just do the math. J Pediatr Urol 11:170.e1–170.e4. https://doi.org/10.1016/j.jpurol.2014.11.020
Anderberg M, Kockum CC, Arnbjornsson E (2009) Morgagni hernia repair in a small child using da Vinci robotic instruments—a case report. Eur J Pediatr Surg 19:110–112. https://doi.org/10.1055/s-2008-1038500
Rossitto C, Gueli Alletti S, Fanfani F, Fagotti A, Costantini B, Gallotta V, Selvaggi L, Monterossi G, Restaino S, Gidaro S, Scambia G (2016) Learning a new robotic surgical device: telelap Alf X in gynaecological surgery. Int J Med Robot Comput Assist Surg MRCAS 12:490–495. https://doi.org/10.1002/rcs.1672
Hutchins AR, Manson RJ, Lerebours R, Farjat AE, Cox ML, Mann BP, Zani S (2018) Objective assessment of the early stages of the learning curve for the Senhance surgical robotic system. J Surg Educ. https://doi.org/10.1016/j.jsurg.2018.06.026
Sng KK, Hara M, Shin J-W, Yoo B-E, Yang K-S, Kim S-H (2013) The multiphasic learning curve for robot-assisted rectal surgery. Surg Endosc 27:3297–3307. https://doi.org/10.1007/s00464-013-2909-4
George EI, Brand TC, LaPorta A, Marescaux J, Satava RM (2018) Origins of robotic surgery: from skepticism to standard of care. JSLS. https://doi.org/10.4293/jsls.2018.00039
Hollands CM, Dixey LN (2002) Applications of robotic surgery in pediatric patients. Surg Laparosc Endosc Percutan Tech 12:71–76
Meehan JJ, Sandler A (2008) Pediatric robotic surgery: a single-institutional review of the first 100 consecutive cases. Surg Endosc 22:177–182. https://doi.org/10.1007/s00464-007-9418-2
Kawal T, Srinivasan AK, Shrivastava D, Chu DI, Van Batavia J, Weiss D, Long C, Shukla AR (2018) Pediatric robotic-assisted laparoscopic pyeloplasty: does age matter? J Pediatr Urol. https://doi.org/10.1016/j.jpurol.2018.04.023
Krauss A, Neumuth T, Wachowiak R, Donaubauer B, Korb W, Burgert O, Muensterer OJ (2012) Laparoscopic versus robot-assisted Nissen fundoplication in an infant pig model. Pediatr Surg Int 28:357–362. https://doi.org/10.1007/s00383-011-3045-7
Jackson HT, Kane TD (2014) Advances in minimally invasive surgery in pediatric patients. Adv Pediatr 61:149–195. https://doi.org/10.1016/j.yapd.2014.03.011
Chapman B, O’Callaghan C, Coxon R, Glover P, Jaroszkiewicz G, Howseman A, Mansfield P, Small P, Milner AD, Coupland RE (1990) Estimation of lung volume in infants by echo planar imaging and total body plethysmography. Arch Dis Child 65:168–170
Acknowledgements
The authors thank Fred Brueckner, Wouter Donders, Sara Lazzaretti, Raul Blanco Sanchez and Anastasios Karamanidis for technical and logistic support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Robert Bergholz is a stockholder of TITAN Medical (a competing robotic system (SPORT) under development), Transenterix and a medical consultant of Transenterix. Sanne Botden, Wim Van Gemert, Stefaan Tytgat and Stefano Gidaro are medical consultants of Transenterix. Transenterix provided the robotic system placed at the UKE Medical Center Hamburg-Eppendorf for study purposes but no other further material. Transenterix covered travel expenses for Sanne Botden, Wim Van Gemert, Stefaan Tytgat and Robert Bergholz for an introductory meeting in Milano, Italy. Johannes Verweij, Michael Boettcher, Heiko Ehlert and Konrad Reinshagen have nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bergholz, R., Botden, S., Verweij, J. et al. Evaluation of a new robotic-assisted laparoscopic surgical system for procedures in small cavities. J Robotic Surg 14, 191–197 (2020). https://doi.org/10.1007/s11701-019-00961-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-019-00961-y