Abstract
Purpose
Bariatric surgery is the most effective treatment for morbid obesity. The present study aimed to assess three bariatric procedures with different mechanisms of actions; sleeve gastrectomy (SG), one-anastomosis gastric bypass (OAGB), and single anastomosis sleeve ileal (SASI) bypass, in terms of efficacy and safety.
Methods
This was a retrospective cohort study on patients with morbid obesity who underwent SG, OAGB, or SASI bypass. The main outcome measures were weight loss and improvement in comorbidities at 6 and 12 months postoperatively, and complications.
Results
A total of 264 patients (186 female) with mean preoperative body mass index (BMI) of 43.6 ± 9.9 kg/m2were included to the study. Significant weight loss was recorded at 6 and 12 months after the three procedures. At 6 and 12 months postoperatively, body weight and BMI were significantly lower after SASI bypass than after SG and OAGB. The %total weight loss (%TWL) and %excess weight loss (%EWL) were significantly higher after SASI bypass than after SG and OAGB. SASI bypass was associated with a significantly higher rate of improvement in DM than SG and OAGB (97.7% vs 71.4% vs 86.7%; p = 0.04) whereas improvement in other comorbidities was similar. The short-term complication rate was similar between the three procedures, yet SASI bypass was followed by higher long-term complication rate.
Conclusion
Based on retrospective review of data, SASI bypass was associated with more reduction in body weight and BMI, higher %TWL and %EWL, better improvement in T2DM, and more long-term nutritional complications than SG and OAGB.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity and type 2 diabetes mellitus (T2DM) have become a major public health problem [1]. Medical treatments usually fail to provide satisfactory results in a considerable number of patients with obesity and T2DM. On the other hand, bariatric surgery has proved to be the most effective treatment for morbid obesity with and without T2DM [2].
Bariatric surgery is traditionally classified into restrictive, malabsorptive, and combined procedures. However, this paradigm needs to be changed as the digestive physiology and the interacting neuroendocrine signals that control hunger and satiety are now better understood. Recent physiologic knowledge can stimulate the design of new bariatric procedures that aim at inducing neuroendocrine changes instead of simple mechanical restriction and /or malabsorption [3].
Santoro et al. have reported long-term data regarding SG with transit bipartition (SG þ TB) [4]. Without exclusions and with a simple surgical procedure, SG þ TB amplifies the nutritive stimulation of the distal gut and simultaneously diminishes the exposure of the proximal bowel to nutrients without completely deactivating the duodenum and jejunum. SASI bypass is a technical modification of SG þ TB that entails a single loop anastomosis instead of a roux en Y anastomosis, thus may potentially be associated with less anastomotic complications and shorter operative time [5].
Sleeve gastrectomy (SG) has gained increasing popularity in the last few years owing to its good outcomes [6]. However, SG can be followed by a number of complications that include staple line leak and bleeding, persistent vomiting, gastroesophageal reflux disease (GERD) and nutritional deficiencies [6, 7]. Furthermore, while SG provides adequate weight loss in patients with BMI < 50 kg/m2, patients with super obesity may have less satisfactory weight loss after SG [8].
One-anastomosis gastric bypass (OAGB) has been assessed in several studies and most of which reported excellent weight loss and improvement in comorbidities after OAGB. Nonetheless, OAGB can be also associated with a number of complications including bile reflux, marginal ulcers, anemia, and nutritional deficiencies [9, 10].
The present study aimed to compare the outcome of three bariatric procedures that employ different mechanisms of weight loss: SG (restrictive mechanism), OAGB (mixed restrictive and malabsorptive mechanism), and the newly introduced SASI bypass (bipartition mechanism). The three procedures were assessed and compared in terms of weight loss, improvement in comorbidities, and complications.
Patients and Methods
Study Design and Setting
Prospective data of patients with morbid obesity who underwent SG, OAGB, or SASI bypass were reviewed. Morbid obesity was defined as BMI > 40 Kg/m2 or > 35 Kg/m2 with at least one associated medical comorbidity.
The study was conducted at Al-Qassimi Hospital in Sharjah, United Arab Emirates in the period of January 2016 to January 2019. Ethical approval for the study was obtained by the principal investigator from the Research Ethics Committee (code: MOHAP/DXB-REC/AAA/No.106/2020).
Selection Criteria
Adult patients of all genders with age less than 65 years with morbid obesity who underwent SG, OAGB, or SASI bypass during the study period were included. All patients included matched the MOHAP guidelines for bariatric surgery. Only patients who completed 12 months of follow-up after surgery were included to the study.
We excluded patients with previous bariatric surgery, major psychiatric disorders, patients unwilling to comply with the dietary regimen after surgery, and patients with ASA III and higher.
Preoperative Assessment and Preparation
Detailed history was taken from every patient with regard to dietary habits, medical comorbidities, and previous investigations and treatments for morbid obesity. Then, general and abdominal examination was performed. Patients’ weight and height were recorded and BMI was calculated. All patients were investigated with abdominal ultrasonography, ECG, chest x-ray, and esophagogastroduodenoscopy before surgery.
Thromboembolic prophylaxis entailed good hydration, wearing an elastic compression stocking before and after the procedure, and subcutaneous injection of low-molecular weight heparin (Enoxaparin, 40 I.U) 12 h before the operation. Informed written consents were taken from the patients after explanation of the nature and possible harms and benefits of each procedure with explanation of the novel, experimental nature of the SASI bypass.
Procedure Selection
The selection of the procedure for each patient was based on shared decision-making between the patient and a multidisciplinary team that included the operating surgeon, obesity physician, dietitian, psychologist, and anesthetist. Factors that were considered when taking the decision on the type of surgery to be performed were baseline BMI, presence of T2DM, presence of GERD, eating behavior, and personal preference of each patient.
During the shared-decision making meetings, patients were asked about their expectations and main concerns then the benefits and drawbacks of each procedure were explained to them. Patients with super obesity were informed that SG may confer suboptimal results in comparison with bypass procedures. Patients with diabetes mellitus were informed that OAGB and SASI bypass confer better remission or improvement in DM than SG as reported in the literature. Patients with GERD were informed about the refluxogenic nature of SG and the literature results denoting good improvement in reflux after OAGB and SASI.
All patients who underwent SASI bypass were informed about the experimental nature of the procedure and that only short-term outcome data are available. The patients were shown schematic illustration of the procedure with emphasis on its potential benefits and complications in the available literature.
Surgery
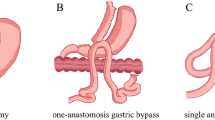
All procedures were performed under general anesthesia in the French position by expert bariatric surgeons. Two grams of the third generation cephalosporines were administered on induction as prophylactic antibiotics. The three procedures entailed different mechanisms of action as shown in Fig. 1.
Sleeve Gastrectomy
After creation of pneumoperitoneum, a 10-mm visual trocar was inserted. Then, under direct vision, a 5-mm trocar was placed under the xiphoid process for introduction of the liver retractor and two additional 12-mm trocars were placed at the right and left midclavicular lines.
Using harmonic ace scalpel™ (Ethicon Endo-Surgery; J & J Medical Ltd., Cincinnati, OH, USA), dissection of the greater curvature of the stomach was started 5–6 cm away from the pylorus and was continued up to the cardio-esophageal junction. Afterwards, a 36-Fr orogastric tube was inserted into the stomach and the stomach was resected using a linear stapler starting 5 cm away from the pylorus, proceeding up to the angle of Hiss. Hemostasis of the staple line was confirmed and if bleeding points were detected, reinforcement of the staple line was done by either oversewing with absorbable suture or placement of clips.
OAGB
The lesser curvature was dissected off the lesser omentum at the level of the crow’s foot using harmonic ace scalpel™. The gastric pouch was created by resecting the stomach transversely then vertically using a linear stapler, guided by the insertion of a 36-Fr intragastric calibration tube.
A gastrotomy was made using the harmonic scalpel at the lowermost point of the gastric pouch, anterior to the staple line. As the greater omentum and transverse colon were retracted cranially, the duodenojejunal junction was identified at the ligament of Treitz and 170 cm of the proximal jejunum was measured downwards. Then, an enterotomy was made in the jejunum at this point using the harmonic scalpel.
A stapled antecolic isoperistaltic loop gastrojejunostomy was created. We ascertained that the calibration tube was introduced easily from the gastric pouch into the alimentary limb of the anastomosis. The anastomotic rent was closed by a single layer of PDS 2/0. The integrity of the staple line was tested by intragastric injection of methylene blue.
SASI Bypass
SASI bypass is a newly introduced, experimental procedure that entails SG with a single gastroileal anastomosis. Upon completion of SG and creation of the gastric pouch as aforementioned, the patient’s position was changed to the Trendelenburg position. The entire length of the small bowel was measured and three meters of the ileum were counted starting from the ileocecal junction. Using a 45-mm linear stapler, an antecolic, isoperistaltic, side-to-side anastomosis between the gastric antrum, 5 cm away from the pylorus, and the ileum was created. The size of the anastomosis was about 3 cm and the afferent limb length was at least 2 m. The anterior wall of the gastroenterostomy was closed with polyglactin or barbed 2/0 running sutures.
Follow-Up
Patients were discharged at the third postoperative day and follow-up was scheduled at the outpatient clinic once every week during the first month after the surgery then every month for 3 months, then every 3 months for 1 year, then on a yearly basis.
Dietary and Nutritional Adjustment
Low-caloric, the protein-rich liquid diet was started for 1 month after surgery, and then, other dietary elements were introduced under the supervision of a specialist dietitian.
A multivitamin supplement was prescribed for all patients in the three groups and included a daily oral supplementation of 18 mg of iron, 400 mcg of folic acid, 800 IUs of vitamin D, and 500 mcg of vitamin B12 in addition to calcium, selenium, copper, and zinc. Moreover, protein supplementation was provided for all patients in the first 6 months.
Patients were subjected to work-up for assessment of the nutritional status at 6 and 12 months after surgery. The work-up included serum hemoglobin, total serum protein, serum albumin, vitamin B12, and vitamin D levels. In select patients, vitamin B1, B6, iron, and copper were assessed when needed.
Study Outcomes
The primary outcomes were weight loss and improvement in comorbidities at 12 months after each procedure. Weight loss was assessed by the %total weight loss (TWL), % excess weight loss (EWL), and % excess BMI loss (EBMIL).
-
%TWL was calculated as [(preoperative weight- weight on follow-up)/preoperative weight] × 100.
-
%EWL was calculated as [(preoperative weight- weight on follow-up)/ (preoperative weight − ideal weight)] × 100
-
%EBMIL was calculated as [(preoperative BMI- BMI on follow-up)/ (preoperative BMI − 25)] × 100
Remission of T2DM was defined as a fasting plasma glucose level < 110 mg/dL or HbA1C level < 42 mmol/mol without hypoglycemic medication at 12 months after surgery. Improvement in T2DM was defined as a reduction of at least 25% in the fasting plasma glucose level and of at least 1% in the HbA1c level with hypoglycemic drug treatment [11].
Improvement in other comorbidities was considered if the disease was controlled after surgery without any medications in line with the standardized outcomes reporting in metabolic and bariatric surgery devised by the ASMBS [11]. The improvement in GERD was assessed with a symptom questionnaire and was confirmed with esophagogastroduodenoscopy. Endoscopic grading of reflux esophagitis was done using the Los Angeles classification [12] (Appendix Table 7). Secondary outcomes included postoperative complications, hospital stay, readmission, and nutritional status.
Data Collected
Preoperative data included age, gender, initial weight, initial BMI, and comorbidities. Operative data included operative time and intraoperative complications. Postoperative data included hospital stay, early postoperative complications, %TWL, %EBMIL, and improvement in complications. Long-term complications occurring after 1 month after surgery such as vomiting, reflux, stricture, intestinal obstruction, hypoalbuminemia, anemia and protein, and vitamin B12 deficiency were also collected. Complications were graded using the Clavien-Dindo classification.
Sample Size and Statistical Analysis
Based on the primary outcome of the study (%TWL at 12 months) and in light of previous literature [13, 14] that reported this parameter after each procedure, the sample size was calculated using online software (https://clincalc.com/stats/samplesize.aspx). The reported average %TWL at 12 months after SG was 34% ± 8.4 versus 38 ± 8.4% after OAGB and 28% ± 13.4 after SASI bypass; therefore, a minimum sample size of 210 patients was required to have a study power of 90% with a significance level set at 5%.
Data were analyzed using SPSS® version 23.0 (IBM® corp, Chicago, USA). Unless stated otherwise, all data were expressed as the mean ± standard deviation (SD) or as numbers and proportions. Descriptive and inferential statistical analyses were performed using both parametric and non-parametric procedures as appropriate. Comparisons of categorical/ordinal variables were performed using Fisher exact test or Chi-Square test for trends. Continuous variables were compared using one-way ANOVA test. All tests were two-tailed and the results with p < 0.05 were considered statistically significant.
Results
Patients’ Characteristics
A total of 264 patients were included to the present study. Patients were 186 (70.4%) female and 78 (29.6%) male with a mean age of 35.2 ± 10.9 years. The mean baseline weight was 113.3 ± 52 kg and the mean preoperative BMI was 43.6 ± 9.9 kg/m2. Forty-one (15.5%) patients had super obesity (BMI > 50 kg/m2).
Regarding obesity-related comorbidities, 85 (32.2%) patients had T2DM, 64 (24.2%) had hypertension, 34 (12.9%) had hyperlipidemia, 38 (14.4%) had GERD, eight (3%) had obstructive sleep apnea, five (1.9%) had depression, and five (1.9%) had polycystic ovary syndrome (PCOS). Preoperative endoscopy revealed GERD in 38 (14.4%) patients, 27 were of endoscopic grade B and 11 of grade C. Twelve (4.5%) patients had an associated hiatus hernia.
Table 1 illustrates the baseline characteristics and demographics of the three groups. Patients who underwent SG were significantly younger (p < 0.0001), more patients with T2DM and hypertension underwent SASI bypass (p < 0.0001), and more patients with GERD underwent OAGB (p < 0.0001). Otherwise, the three groups were comparable in regards sex distribution, baseline weight, BMI, percent of super obesity, and other comorbidities.
Weight Loss
Significant weight loss was recorded at 6 and 12 months after the three procedures as revealed by a significant decrease in weight and BMI compared to baseline values and a significant increase in %TWL, %EWL, and %EBMIL.
At 6 months postoperatively, body weight and BMI were significantly lower after SASI bypass than after SG and OAGB (p = 0.01 & 0.04). The %TWL, %EWL, and %EBMIL were significantly higher after SASI bypass than after SG and OAGB (p = 0.0001, < 0.0001, 0.02).
Similarly, at 12 months postoperatively, body weight and BMI were significantly lower after SASI bypass than after SG and OAGB (p < 0.0001). The %TWL and %EWL were significantly higher after SASI bypass than after SG and OAGB (p < 0.0001 each) whereas the %EBMIL was comparable among the three groups (p = 0.059) (Table 2).
Improvement in Comorbidities
At 12 months postoperatively, SASI bypass was followed by a significantly higher rate of remission or improvement in T2DM compared to SG and OAGB (97.7% vs 71.4% vs 86.7%; p = 0.04). The three procedures were associated with similar improvement in hypertension (p = 0.35), hyperlipidemia (p = 0.6), sleep apnea (p = 0.99), and GERD (p = 0.72) (Table 3). All patients with preoperative GERD answered the symptom questionnaire and had follow-up endoscopy after surgery. The improvement in GERD after the three procedures in terms of clinical and endoscopic findings is shown in Table 4.
Complications and Readmissions
All complications recorded in this study were of grade II–III on the Clavien-Dindo classification. Short-term complications occurred in one patient after OAGB in the form of pouch gangrene and perforation and in three patients after SASI bypass in the form of bleeding and obstruction whereas no short-term complications were recorded after SG. SASI bypass had the highest rate of short-term complications; however, the difference between the three procedures was not statistically significant (0 vs 1 vs 4% in SG, OAGB, SASI bypass respectively, p = 0.07).
Long-term complications involved hypoalbuminemia in two patients who underwent SG, nine patients who underwent OAGB, and nine patients who had SASI bypass. Two patients developed peripheral neuropathy after SASI bypass due to vitamin deficiency. There was a significant difference between the three procedures in terms of long-term complications (2% vs 9.8% vs 14.9%, p = 0.005).
The nine patients who developed hypoalbuminemia after SASI bypass had bypass of a median of 53.8% of small bowel (range, 45.4–60%) whereas patients who did not experience hypoalbuminemia after SASI bypass had bypass of a median of 50% of small bowel (range, 40–57%).
Overall, the readmission rates were similar after the three procedures (1% vs 2.2% vs 4%, p = 0.45). Causes of readmission comprised abdominal pain, fever, acute pancreatitis, and need for pouch revision after OAGB (Table 5). A summary of the outcome of the three procedures is shown in Fig. 2.
Changes in the Nutritional Status
All patients in the three groups were available for assessment of the nutritional status at 12 months postoperatively since the study included only patients who completed this period of follow-up. All procedures were followed by a significant decrease in serum protein levels at 12 months postoperatively, yet it was within the normal laboratory range (6–8 g%). There were no significant differences between the three procedures in terms of preoperative and postoperative total protein levels.
The three procedures uniformly reduced the serum protein levels; however, the serum albumin levels showed an insignificant decrease after OAGB and SASI bypass whereas they showed a non-significant increase after SG.
All procedures were followed by a significant increase in vitamin B12 levels on follow-up. The baseline and postoperative vitamin B12 levels were significantly higher after SASI bypass than after OAGB and SG (Table 6).
Discussion
The present study assessed the outcome of three bariatric procedures that employ three different mechanisms of action. SG relies on the principle of mechanical restriction of the gastric capacity with relevant changes in satiety hormones and ghrelin [15]. OAGB employs the principle of restriction plus diversion similar to the classical RYGB yet with a single instead of double anastomosis. SASI bypass follows the principle of bipartition as devised by Santoro et al. [4] when they introduced the original transit bipartition and SG.
Each procedure has its own advantages and shortcomings. While SG is considered the simplest procedure in terms of technical aspects, it usually provides better results in patients with BMI less than 50 kg/m2 and weight regain after SG is a possible sequel with an incidence up to 75% at 6 years [16]. OAGB provides superior weight loss and improvement in T2DM compared to SG, yet is associated with bile reflux and nutritional deficits. In addition, digestive tract exclusions may cause atrophy of the mucosa, with bacterial proliferation that leads to bacterial translocation to the portal system [17]. On the other hand, SASI bypass confers excellent improvement in T2DM which is why it was originally introduced as a metabolic procedure. However, since SASI bypass has been recently introduced, it may be considered as an investigational, rather than a fully established and thoroughly assessed procedure.
Although most baseline characteristics of the patients in the three groups were similar, some significant differences were present and may reflect the way each procedure was chosen for the patients. Patients who underwent SG were younger than patients who underwent OAGB or SASI bypass. Younger patients maybe more prone to weight regain after surgery as they have longer follow-up, and since weight regain after SG can be more easily managed with re-sleeve or conversion to bypass surgery, this may explain the prevalence of SG in younger patients. More patients with T2DM underwent SASI bypass perhaps because the procedure was mainly introduced as a metabolic surgery for T2DM and several studies [6, 13, 18] reported excellent improvement in T2DM after SASI that was greater than 90%.
Only 5% of patients with GERD chose to have SG since the procedure tends to be associated with a considerable risk of developing GERD postoperatively. The majority (76%) of patients with GERD chose to have OAGB since it has been reported in the literature [19] to be followed by a significant improvement in GERD symptoms, comparable to its improvement after RYGB.
A comparable proportion of patients with super obesity underwent sleeve gastrectomy and SASI bypass (13% vs 12%), yet a higher proportion (21%) underwent OAGB; however, this difference was not statistically significant. Since the procedure selection was based on shared-decision making with the patients, more patients with BMI > 50 kg/m2 chose to have OAGB since it attains better results in larger BMI, comparable to the original RYGB [20].
The three procedures achieved significant weight loss with incremental increase in %TWL, %EWL, and %EBMIL on follow-up. However, the reduction in BMI and increase in %TWL and %EWL at 12 months postoperatively was more significant after SASI bypass compared to SG and OAGB. It has been assumed that the ideal bariatric procedure should induce weight loss through function restriction and modulation of the neuroendocrine control of hunger and satiety, as the SASI bypass does, rather than mechanical restriction and malabsorption. This has been defined as the digestive adaptation technique as inducted by Santoro and colleagues [3].
Weight loss after bipartition procedures is not only caused by restriction of the gastric volume or decreased nutrient absorption, but it is mainly produced by the neuroendocrine response generated by the early reception of nutrients in the distal bowel, stimulating the secretion of satietogenic distal gut hormone, reducing the activity of the proximal bowel, and inducing a hypothalamic- mediated satiety sensation [21]. However, to date, there is no human study that assessed the hormonal changes after the SASI bypass. Since there is a portion of food that passes through the duodenum into the normal pathway, the subsequent effects of this phenomenon on the enteric hormones need to be investigated in future prospective studies.
This exact neuroendocrine response is the key mechanism that explains the superlative remission or improvement in T2DM after SASI bypass as previously discussed [5]. This was reproduced in the present study as the SASI bypass was associated with a significantly higher rate of improvement in T2DM than OAGB and SG. The rate of improvement was 97%, within the range (89–100%) reported in the literature on SASI procedure [6, 13, 18, 22, 23]. On the other hand, all three procedures were followed by comparable rates of improvement in hypertension and hyperlipidemia. Although the SASI bypass was followed by a higher improvement in GERD than OAGB and SG, this difference was not statistically significant, probably because of the small number of patients with GERD in the study.
The short-term, procedure-related complication rates were statistically comparable among the three procedures. Nonetheless, the difference between the three procedures, although not statistically significant, can be clinically significant, and such a difference may be more prominent with a larger number of patients.
The SASI bypass was followed by a significantly higher long-term complication rate that mainly involved nutritional deficiencies. Overall, most complications recorded in the study were of minor to moderate grade and there were only two major complications in the form of obstruction after SASI bypass and pouch gangrene and rupture after OAGB, which may imply the good safety profile of the three procedures.
The patient who developed pouch gangrene after OAGB was a male patient with super obesity and history of cigarette smoking. The patient presented postoperatively with tachycardia and dyspnea; abdominal CT was free apart from mild pleural effusion. On laparoscopic assessment, the lower one-third of the pouch was gangrenous. Excision of the gangrenous part of the pouch and undo of the anastomosis was performed. Then, using linear stapler, a side-to-side anastomosis between the residual gastric pouch and the remaining stomach was done. The patient was discharged home in a good condition and did not experience further problems on follow-up.
Most complications after the SASI bypass were protein and vitamin deficiencies. It is worthy to note that hypoalbuminemia occurred after the three procedures, yet at variable rates. The incidence of hypoalbuminemia requiring correction was lower after SG (2%) in comparison with OAGB (10%) and SASI (12%), which can be reasonable since SG does not entail any form of diversion, exclusion, or malabsorption. This was demonstrated by assessment of the change in the nutritional status after the three procedures as patients who underwent SG had higher serum albumin levels than those who underwent OAGB or SASI bypass. Nonetheless, the decrease in serum albumin levels at 12 months after the three procedures was non-significant. Overall, the total protein and albumin levels were within the normal laboratory range after the three procedures.
Patients who developed hypoalbuminemia were treated with protein supplementation and high-protein diet. Patients with serum albumin < 2.5 g% were given intravenous albumin infusion for 1 week, in addition to the high protein diet and protein supplementation. Strict follow-up with focused patient education was employed for 3 months to improve patient compliance. Reasons for hypoalbuminemia varied among the three groups. In the OAGB and SASI groups, the bypass of a portion of the small bowel with inadequate absorption of dietary proteins was the main cause. As reported in a literature review [24], the median rate of hypoalbuminemia after SG was 4%; however, its exact cause is not clear and maybe attributed to dietary restrictions related to the size of the gastric pouch. In most cases, lack of patient compliance with the dietary and supplementation instructions may be the main reason for hypoalbuminemia.
Two patients with type II DM developed peripheral neuropathy after SASI bypass due to deficiency of vitamin B1 (Thiamin). This complication, although not frequently common, is possible after the SASI bypass because a part of the small bowel is being bypassed, thus may be associated with poor absorption of vitamin B that predisposes to peripheral neuropathy, especially in diabetic patients. The patients showed complete recovery after daily supplementation with 100 mg of vitamin B1 (intravenous infusion for 3 days then oral supplementation for 2 months). Although thiamine is typically included in the multivitamin supplement prescribed to the patients, its amount is fairly small; thus, additional supplementation of vitamin B1 may be indicated in some patients.
The present study is limited by its retrospective, non-randomized, single-center nature. Although the lack of randomization resulted in some imbalance in the baseline characteristics among the three procedure, this may actually reflect the real-life practice and how bariatric surgery is being tailored to fit every patient’s needs and expectations. The outcome assessed in this study is short-term and longer follow-up is needed. Other nutritional parameters such as calcium, iron, zinc, and vitamin B6 were not regularly assessed after the procedures.
Conclusions
SASI bypass is a feasible procedure that was associated with more reduction in body weight and BMI, higher %TWL and %EWL, better improvement in T2DM, and more long-term nutritional complications than SG and OAGB. These conclusions should be interpreted with caution owing to the retrospective, single-center nature of the study and the small numbers included to each group. Multicenter prospective studies comparing the three procedures are required to ascertain these preliminary conclusions. Careful selection of the bariatric procedure in accordance with each patient’s condition and expectations is crucial in order to achieve the best possible results.
References
Chen L, Magliano DJ, Zimmet PZ. The worldwide epidemiology of type 2 diabetes mellitus--present and future perspectives. Nat Rev Endocrinol. 2011;8(4):228–36. https://doi.org/10.1038/nrendo.2011.183.
Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366(17):1567–76. https://doi.org/10.1056/NEJMoa1200225.
Santoro S, Velhote MC, Malzoni CE, et al. Preliminary results from digestive adaptation: a new surgical proposal for treating obesity, based on physiology and evolution. Sao Paulo Med J. 2006;124(4):192–7. https://doi.org/10.1590/s1516-31802006000400004.
Santoro S, Castro LC, Velhote MC, et al. Sleeve gastrectomy with transit bipartition: a potent intervention for metabolic syndrome and obesity. Ann Surg. 2012;256(1):104–10. https://doi.org/10.1097/SLA.0b013e31825370c0.
Mahdy T, Al Wahedi A, Schou C. Efficacy of single anastomosis sleeve ileal (SASI) bypass for type-2 diabetic morbid obese patients: gastric bipartition, a novel metabolic surgery procedure: a retrospective cohort study. Int J Surg. 2016;34:28–34. https://doi.org/10.1016/j.ijsu.2016.08.018.
Emile SH, Elfeki H, Elalfy K, et al. Laparoscopic sleeve gastrectomy then and now: an updated systematic review of the progress and short-term outcomes over the last 5 years. Surg Laparosc Endosc Percutan Tech. 2017;27(5):307–17. https://doi.org/10.1097/SLE.0000000000000418.
Elbanna H, Ghnnam W, Negm A, et al. Impact of preoperative body mass index on the final outcome after laparoscopic sleeve gastrectomy for morbid obesity. Ulus Cerrahi Derg. 2016;32(4):238–43. https://doi.org/10.5152/UCD.2016.3275.
Emile SH. Gastroesophageal reflux disease after sleeve gastrectomy: the need to predict its onset and prevent its consequences. Obes Surg. 2019;29(8):2625–6. https://doi.org/10.1007/s11695-019-03955-9.
Rutledge R, Walsh TR. Continued excellent results with the mini-gastric bypass: six-year study in 2,410 patients. Obes Surg. 2005;15(9):1304–8. https://doi.org/10.1381/096089205774512663.
Mahawar KK, Kumar P, Carr WR, et al. Current status of mini-gastric bypass. J Minim Access Surg. 2016;12(4):305–10. https://doi.org/10.4103/0972-9941.181352.
Brethauer SA, Kim J, E Chaar M, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Obes Surg. 2015;25(4):587–606. https://doi.org/10.1007/s11695-015-1645-3.
Armstrong D, Bennett JR, Blum AL, et al. The endoscopic assessment of esophagitis: a progress report on observer agreement. Gastroenterology. 1996;111(1):85–92. https://doi.org/10.1053/gast.1996.v111.pm8698230.
Mahdy T, Emile SH, Madyan A, et al. Evaluation of the efficacy of Single Anastomosis Sleeve Ileal (SASI) bypass for patients with morbid obesity: a multicenter study. Obes Surg. 2020;30(3):837–45. https://doi.org/10.1007/s11695-019-04296-3.
Kansou G, Lechaux D, Delarue J, et al. Laparoscopic sleeve gastrectomy versus laparoscopic mini gastric bypass: one year outcomes. Int J Surg. 2016;33 Pt A:18–22. https://doi.org/10.1016/j.ijsu.2016.07.051.
Itlaybah A, Elbanna H, Emile S, et al. Correlation between the number of ghrelin-secreting cells in the gastric fundus and excess weight loss after sleeve gastrectomy. Obes Surg. 2019;29(1):76–83. https://doi.org/10.1007/s11695-018-3498-z.
Lauti M, Kularatna M, Hill AG, et al. Weight regain following sleeve gastrectomy-a systematic review. Obes Surg. 2016;26(6):1326–34. https://doi.org/10.1007/s11695-016-2152-x.
Castillo J, Fabrega E, Escalante CF, et al. Liver transplantation in a case of steatohepatitis and subacute hepatic failure after biliopancreatic diversion for morbid obesity. Obes Surg. 2001;11(5):640e642.
Madyan A, Emile SH, Abdel-Razik MA, et al. Laparoscopic single anastomosis sleeve ileal (SASI) bypass for patients with morbid obesity: technical description and short-term outcomes. Surg Laparosc Endosc Percutan Tech. 2020;30(2):e13–7. https://doi.org/10.1097/SLE.0000000000000763.
Fahmy MH, Sarhan MD, Salman MA, et al. Gastro-esophageal reflux disease after laparoscopic mini-gastric bypass and Roux-en-Y gastric bypass: is there a difference? Bariatr Surg Pract Patient Care. 2018;13:109–14. https://doi.org/10.1089/bari.2018.0018.
Magouliotis DE, Tasiopoulou VS, Tzovaras G. One anastomosis gastric bypass versus Roux-en-Y gastric bypass for morbid obesity: a meta-analysis. Clin Obes. 2018;8(3):159–69. https://doi.org/10.1111/cob.12246.
Lustig RH. The neuroendocrinology of obesity. Endocrinol Metab ClinNorth Am. 2001;30(3):765e785.
Kermansaravi M, Kabir A, Pazouki A. 1-year follow-up of single anastomosis sleeve ileal (SASI) bypass in morbid obese patients: efficacy and concerns. Obes Surg. 2020;30:4286–92. https://doi.org/10.1007/s11695-020-04781-0.
Abouzeid MM, Helmy MM, Abdulaziz MM, et al. Single anastomosis sleeve ileal bypass (SASI) for management of obese patients with type 2 diabetes. Life Sci J. 2019;16(11):112–20.
Emile SH, Elfeki H. Nutritional deficiency after sleeve gastrectomy: a comprehensive literature review. EMJ Gastroenterol. 2017;6(1):99–105.
Author information
Authors and Affiliations
Contributions
Tarek Mahdy designed the study and participated in data collection and revision of the manuscript. Sameh Emile contributed to data interpretation and analysis, writing, and critical revision of the manuscript. Waleed Gado, Carl Schou, and Abdulwahid Alwahidi contributed to data interpretation and review of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethical approval for the study was obtained from the Research Ethics Committee.
Informed Consent
Informed consent does not apply as for this type of study formal consent is not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Mahdy, T., Gado, W., Alwahidi, A. et al. Sleeve Gastrectomy, One-Anastomosis Gastric Bypass (OAGB), and Single Anastomosis Sleeve Ileal (SASI) Bypass in Treatment of Morbid Obesity: a Retrospective Cohort Study. OBES SURG 31, 1579–1589 (2021). https://doi.org/10.1007/s11695-020-05159-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-05159-y