Abstract
Background
The Montpellier bariatric team has recently proposed some technical alternatives to decrease the rate of gastroesophageal reflux disease (GERD) after bariatric surgery and also to offer patients an alternative in case of contraindication to Roux-en-Y gastric bypass (RYGBP): the Nissen-Sleeve (N-Sleeve).
Objectives
We present here the results from a cohort of patients that underwent an operation with this newly designed anti-reflux bariatric procedure N-Sleeve: Nissen valve added to a standard SG.
Methods
Data from a prospective, observational, and monocentric cohort. All consecutive patients presenting to the bariatric surgery department for a laparoscopic sleeve gastrectomy between 2016 and 2018 with GERD were included in the study. The fundus was stapled with a margin from the valve, and the valve was created with tissue at a distance from the greater curvature so as to avoid a double layer stapling of the stomach.
Results
A total of 70 patients were included in the study. Ninety percent of the cohort presented with a hiatal hernia at the time of surgery. No mortality was observed during the follow-up period. Concerning GERD, 76% of all patients had preoperative esophageal syndromes, whereas 21% were asymptomatic with associated esophagitis. Grade A–C esophagitis was present in 99% of the cohort, but no Barrett’s esophagus was present. Fifty-six (80%) patients used PPIs regularly. At 1 year of follow-up, one patient was still symptomatic.
Conclusions
Comparative trials remain necessary between N-Sleeve and standard bariatric procedures to refine the specific indications of each of them and determine the eventual role of the N-Sleeve.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic sleeve gastrectomy (SG) has become one of the most popular bariatric procedures in the world [1,2,3,4]. In France, more than 27,500 SGs were performed in 2014 [5]. This operation consists in removing 70 to 80% of the stomach, sparing the lesser curvature along with the pylorus. Several factors have contributed to its increasing popularity including minimal changes in gastrointestinal anatomy, short operative time, and excellent efficacy in weight reduction [3, 4]. Its standard configuration and simplicity are perhaps the main reasons for its worldwide success along with the long-term weight loss and the absence of significant nutritional deficiencies; reproducibility thus induces popularity.
Additionally, obese patients have a higher risk of developing reflux symptoms compared to the general population. Long-term complications after SG such as gastroesophageal reflux disease (GERD) and weight regain are probably under-evaluated. Currently, for the surgical management of morbidly obese patients presenting with GERD or hiatal hernia, Roux-en-Y gastric bypass (RYGB) is the gold standard procedure [6,7,8]. But it is recognized that GERD can also occur after RYGB [5]. The Montpellier bariatric team has recently proposed some technical alternatives [9] in order to decrease the rate of GERD after bariatric surgery and also to offer patients an alternative in case of contraindication to RYGBP (e.g., if regular endoscopic monitoring is required, lifelong treatment) [10,11,12,13]. We here present the results from a cohort of patients operated at the Andalous Clinic in Casablanca, Morocco, with this newly designed anti-reflux bariatric procedure (Nissen valve added to a standard SG).
Material and Methods
Data from a prospective, observational, and monocentric cohort was collected at the Andalous Clinic in Casablanca (Morocco) by one of the authors. All consecutive patients that presented at the bariatric surgery department for a laparoscopic sleeve gastrectomy between 2016 and 2018 with GERD were included in the study.
GERD was defined by the symptoms or complications that develop due to the reflux of gastric content, according to the Montreal’s definition [14]. The patients included were expected to regularly use proton pump inhibitors (PPIs). Previous bariatric procedures were contraindications for this new approach. The staff surgeon has been performing sleeve gastrectomy since 2007 with an experience of over 1500 cases. Therefore, no learning curve for a standard SG was expected to impact the results of our study. All the patients were individually informed about the experimental purpose of this new technique, and they signed an informed consent form.
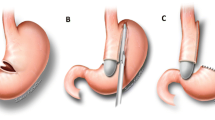
Surgical Technique (Fig. 1)
All operations were performed under general anesthesia and by laparoscopic approach using the French technique (the surgeon standing between the patient’s legs). Each procedure required 5 ports. Pneumoperitoneum was induced by inserting a Veress needle into the left hypochondrium and maintained at a pressure of 12 mmHg. The first step of the N-Sleeve technique was the dissection and reduction of a hiatal hernia if present. An extension of at least 5 cm of abdominal esophagus was achieved, and all the anterior and the posterior esophageal hiatal space was cleared. Then the greater curvature of the stomach was dissected from the short gastric vessels and gastro colic ligament as long as 6 cm from the pylorus using an impedance coagulator Ultracision® (Ethicon Endo-surgery, Johnson-Johnson Inc. 2010, USA). A careful dissection was performed at the level of the gastric fundus, in order to keep an appropriate distance from the gastric wall and to avoid any possible thermal injury to this important part, which would be used for the creation of the valve. The valve remains vascularized as in the standard Nisse technique. The hiatal orifice was closed by 2 or 3 nonabsorbable sutures of Ethibond® 2.0 suture (Johnson-Johnson Inc., USA), and a 37F calibration tube was introduced to the stomach. A short Nissen valve of 2–3 cm was created using Ethibond® 3.0 suture (Johnson-Johnson Inc., USA). This valve is created with the purpose of diminishing the reflux. A fixation suture was passed between the valve and the right pillar. Dissection of the rest of the greater curvature continued until 6 cm from the pylorus. A laparoscopic linear stapler was introduced into the peritoneal cavity and was positioned so that it divided the stomach parallel to the calibration tube along the lesser curvature. The instrument was fired and reloaded, and the procedure was repeated. A maximum of 8 cartridges were used to staple the antrum, the body, and the fundus of the stomach. The fundus was stapled leaving a margin from the valve, and the valve was created using tissue at a distance from the greater curvature so as to avoid a double layer stapling of the stomach. For patients who presented with a high risk of bleeding (hypertension, need for high anticoagulation treatment), a buttressing material Seamguard (W.L. Gore & Associates, Flastaff, AZ) was used. The final aspect is an appropriate Nissen valve combined with a sleeved stomach (Fig. 1).
All patients received perioperative deep vein thrombosis prophylaxis using low molecular weight heparin and intermittent pneumatic leg compression during the operation. Patients were allowed to drink on postoperative day 1, and PPIs were stopped after surgery. Patients were regularly followed up at 1, 6, and 12 months after discharge. Recorded characteristics included age, gender, weight, height, body mass index (BMI), comorbidities, and ASA classification; these are summarized in Table 1.
GERD symptoms, complications, and treatments were evaluated through the consultation that was applied before and at the end of the first year of follow-up. GERD was considered under control according to compound criteria of symptoms relief without PPI and absence of esophagitis at the 1-year follow-up upper endoscopy.
Operative time, length of stay, complications, and reoperation data were also collected. Weight loss over the first year was measured using changes in BMI, excess weight loss (with the calculation of ideal body weight based on a BMI of 25 kg/m2) and total body weight loss. Demographic and clinical data, complications, and reoperations were recorded prospectively using a standardized database. [15]
Results
A total of 70 patients were included in the study. The study cohort comprised a majority of females (80%) with a mean age of 42 years and a mean BMI of 40 kg/m2. Major comorbidities were sleep apnea, arthrosis, and high blood pressure with no ASA III patients. Ninety percent of the cohort presented with a hiatal hernia at the time of surgery. No mortality was observed during the follow-up period.
However, three major complications were detected. One conversion to an open surgery was needed intra-operatively due to an uncontrolled bleeding with no postoperative adverse events (Table 2). One patient presented with a late stenosis and was readmitted for endoscopic dilatation. A third patient developed a generalized peritonitis secondary to a gastric fistula on postoperative day 7, treated by a peritoneal lavage of the abdominal cavity. An upper endoscopy was performed with evidence of a fistula on the gastric longitudinal staple line and a distal gastric tube stenosis. A double pigtail was implanted. At 3 months, the fistula persisted, and a conversion to a RYGB was performed on a new gastric pouch after the resection of the valve, the gastric tube, and the fistula. The postoperative period was uneventful, and the follow-up revealed no abnormalities including GERD [16].
Concerning GERD, 76% of all patients had preoperative esophageal syndromes, whereas 21% were asymptomatic with associated esophagitis. Grade A–C esophagitis was present in 99% of the cohort, but no Barrett’s esophagus was present. Fifty-six (80%) patients used PPIs regularly.
At 1 year of follow-up, one patient was still symptomatic (1%). There were persistent cases of esophagitis but in reduced proportions (Table 3), and 5 (7%) patients were still regularly using PPIs. Weight loss results are presented in Table 4.
Discussion
GERD is the main mechanism underlying the transformation of the esophageal squamous mucosa into metaplastic columnar mucosa [17], a predominant factor in the physiopathology of gastroesophageal junction cancer. Indeed, the incidence rate of malignant transformation of BE has been evaluated at between 0.6 and 0.7% per year in two large meta-analyses [18, 19]. In addition to the functional impairment it implies, the malignant potential of GERD emphasizes the importance of this medical condition.
The association between obesity and GERD is well known, and obese patients have an increased risk of developing reflux symptoms compared to the general population [19, 20]. Moreover, GERD is present in the vast majority of patients seeking a bariatric procedure [21]. Developing the most appropriate surgical procedure to simultaneously address these two issues is thus of primary importance. While it has been argued that SG might decrease GERD because of the reduction in intra-abdominal pressure, gastric acid production, gastric volume, and increased gastric emptying [22, 23], it now seems evident from the literature that the true weakness of this procedure is the long-term occurrence of GERD [24]. Genco et al. first published alarming systematic endoscopy results of 17.2% of 110 patients with Barrett’s esophagus after SG at a median follow-up of 58 months [25]. Sebastianelli et al. reported a 76% prevalence of GERD symptoms at 5 years follow-up after SG in a cohort of ninety patients [26]. Many mechanisms have been claimed to be responsible for the increased rate of GERD observed after SG, such as the disruption of anatomical anti-reflux mechanisms after surgery, decreased gastric compliance, increased intragastric pressure, localized stricture, or angulation of the gastric tube at the junction between the body and the antrum of the stomach, the gastric twist, the final shape of the sleeve (funnel shape), the persistence of a significant part of the gastric fundus, and the presence of a hiatal hernia. It should be highlighted that this association between SG and GERD is under intense debate, but recent studies point toward a strong correlation in the long term.
An alternative and more consensual approach is the realization of a RYGB [6,7,8] in the setting of GERD associated to morbid obesity. Indeed, the latter works as an anti-reflux procedure because the Roux-en-Y loop anatomy avoids bile reflux, and the small, gastric pouch based in the lesser curvature that excludes the acid-secreting gastric fundus limits the production of hydrochloric acid that may come in contact with the esophagus.
There is currently no consensus on the treatment of obesity associated with GERD. SG in this setting is put into question with a tendency toward contraindication. The RYGB is the recommended procedure but is losing popularity due to the technicity it requires, slowing its generalization in the common setting. Thus, there is a room for improvement.
The N-Sleeve proposes a technical change to the standard SG, which attempts to preserve the ease and reproducibility of this procedure. Reflux control in our series was obtained after surgery. The rate of symptom control rose to 99% at 1 year post operation, which is quite a promising result considering that the operative time and hospital stay were not increased. However, there were cases of persistent esophagitis but in reduced proportions and persistent use of PPI (7%) at 1 year of follow-up. One patient presented with preoperative bleeding which was successfully managed by being converted to open and another upper staple line fistula which was managed using delayed conversion to RYGB [16], and two patients presented with delayed stenosis treated by endoscopic dilatation. There was no mortality. The early series from Montpelier experienced an increased rate of leak that was not evidenced in our series (1%). Indeed, the series of Pr Nocca’s team allowed us to be very selective on our indications.
Furthermore, in our series, excess weight loss was 69 ± 20% which can be paralleled to the weight loss results of a standard SG. Indeed, leaving a small part of gastric fundus including the esophagus could eventually compromise the bariatric effect of this technique, but the results of this cohort seem to contradict this theory, at least at the 1-year follow-up.
The hormonal mechanism is not yet clear. The decrease in ghrelin levels after RYGB is also significant, suggesting that it is not necessarily the resection of the pouch that will lead to the decrease in ghrelin. The fundus left for the valve is very small and especially not functional (like the RYGB). Moreover, there is also a minor secretion of ghrelin in the antro-pyloric region.
Other bariatric teams tackled the combined issue of GERD and morbid obesity via different approaches; some new modifications have been proposed to the standard SG such as a Collis-Nissen procedure by Silva [11] or a cardiopexy with ligamentum teres [13] with promising results. The rationale of the N-Sleeve procedure resides in the combination of the two most popular and common procedures addressing both GERD and obesity, thus preserving their simplicity and reproducibility.
In our study, GERD was defined by the symptoms or complications that develop due to the reflux of gastric content, according to the Montreal’s definition. However, EGD is not a sensitive marker for pathologic GERD. Grade A and B esophagitis can often be seen in the setting of normal GERD. There is also a portion of the population that will suffer from hypersensitivity or functional heartburn that will not have true reflux, in the absence of any objective evaluation for GERD – pH impedance, 24-h pH catheter test, or Bravo pH tests.
If results of N-Sleeve with longer follow-up and larger number of patients remain as good as those presented in this series and in Nocca et al. [9], N-Sleeve could become a new standard in treating morbid obesity with the onset of GERD. There is thus an urgent need to evaluate this procedure in a randomized controlled trial; the question of the control group remains: Should we consider RYGB the standard procedure?
Finally, our preliminary results stop us from drawing any conclusion on the efficacy of N-Sleeve on GERD. The only affirmation possible is that N-Sleeve is feasible in morbidly obese patients that present with GERD with a safety that is comparable to current bariatric procedures. These primary results of 1 year showed that there was no difference in terms of EWL results when compared to standard SG. However, a year is too short a period of time, even to establish GERD control rate, as GERD onset could occur later on [27]. Besides, long-term results, at least at 5 years, are very important to monitor potential fundus dilation to understand how effective the procedure is on weight loss in the long term when part of the fundus is left in place.
Conclusion
Comparative trials remain necessary between N-Sleeve and standard bariatric procedures (SG and RYGB) to refine the specific indications of each of them and determine the eventual place of N-Sleeve.
References
Dupree CE, Blair K, Steele SR, et al. Laparoscopic sleeve gastrectomy in patients with preexisting gastroesophageal reflux disease: a national analysis. JAMA Surg. 2014; https://doi.org/10.1001/jamasurg.2013.4323.
Hutter MM, Schirmer BD, Jones DB, et al. First report from the American College of Surgeons bariatric surgery center network: laparoscopic sleeve gastrectomy has morbidity and effectiveness positioned between the band and the bypass. Ann Surg. 2011;254(3):410–20. https://doi.org/10.1097/SLA.0b013e31822c9dac. discussion 420–2
Deitel M, Crosby RD, Gagner M. The First International Consensus Summit for Sleeve Gastrectomy (SG), New York City, October 25–27, 2007. Obes Surg. 2008;18(5):487–96. https://doi.org/10.1007/s11695-0089471-5.
Fischer L, Hildebrandt C, Bruckner T, et al. Excessive weight loss after sleeve gastrectomy: a systematic review. Obes Surg. 2012;22(5):721–31. https://doi.org/10.1007/s11695-012-0616-1.
Schaaf C, Iannelli A, Gugenheim J. État actuel de la chirurgie bariatrique en France. E-mémoires de L’Académie Nation de Chir. 2015;14(2):104–7.
Varella JE, Hinojosa MW, Nguyen NT. Laparoscopic fundoplication compared with laparoscopic gastric bypass in morbidly obese patients with gastroesophageal reflux disease. Surg Obes Relat Dis. 2009;5(2):139–43.
Prachand VN, ALverdy JC. Gastroesophageal reflux disease and severe obesity: fundoplication or bariatric surgery? Wourld J Gastroenterol. 2010;16(30):3757–61.
Katz P, Gerson L, Vela M. Diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol. 2013;108:308–2.
David Nocca MD, PhD, El Mehdi Skalli MD, Eric Boulay MD, Marius Nedelcu MD, Jean Michel Fabre MD, PhD, Marcelo Loureiro MD, PhD, The Nissen Sleeve (N-Sleeve) operation: preliminary results of a pilot study, Surg Obes Relat Dis, https://doi.org/10.1016/j.soard.2016.02.010
Daes J, Jimenez ME, Said N, et al. Laparoscopic sleeve gastrectomy: symptoms of gastroesophageal reflux can be reduced by changes in surgical technique. Obes Surg. 2012;22(12):1874–9. 7
Da Silva LE, Alves MM, El-Ajouz TK, et al. Laparoscopic Sleeve-Collis-Nissen gastroplasty: a safe alternative for morbidly obese patients with gastroesophageal reflux disease. Obes Surg. 2014;25(7):1217–22.
Soricelli E, Casella G, Rizzello M, et al. Initial experience with laparoscopic crural closure in the management of hiatal hernia in obese patients undergoing sleeve gastrectomy. Obes Surg. 2010;20:1149–53.
Gálvez-Valdovino R, Cruz Vigo JL, Marín Santillán E, et al. Cardiopexy with ligament teres in patients with hiatal hernia and previous sleeve gastrectomy: an alternative treatment for gastroesophageal reflux disease. Obes Surg. 2015;25(8):1539–43.
Vakil M, Van Zanten SV, Kahrilas P, et al. Global consensus group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101(8):1900–20.
Brethauer SA, Kim J, el Chaar M, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Surg Obes Relat Dis. 2015;11(3):489–506.
Ben Amor I, Debs T, Petrucciani N, et al. Chronic fistula post laparoscopic Nissen sleeve gastrectomy: conversion to Roux-en-Y gastric bypass. Obes Surg. 2019;29:3414–5. https://doi.org/10.1007/s11695-019-04080-3.
Spechler SJ, Souza RF. Barrett’s esophagus. N Engl J Med. 2014;371(9):836–45.
Steevens J, Schouten LJ, Driessen ALC, et al. A prospective cohort study on overweight, smoking, alcohol consumption, and risk of Barrett’s esophagus. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol. 2011;20(2): 345–58. 25.
Gatenby P, Ramus J, Caygill C, et al. Routinely diagnosed low grade dysplasia in Barrett’s oesophagus: a population-based study of natural history. Histopathology. 2009;54(7):814–9.
Tutuian R. Obesity and GERD: pathophysiology and effect of bariatric surgery. Curr Gastroenterol Rep. 2011;13:205–12.
Braghetto I, Csendes A. Prevalence of Barret’s esophagus in bariatric patients undergoing sleeve gastrectomy. Obes Surg. 2015;26(4):710–4.
Anand G, Katz PO. Gastroesophageal reflux disease and obesity. Rev Gastroenterol Disord. 2008;8(4):233–9.
Sharma A, Aggarwal S, Ahuja V, et al. Evaluation of gastroesophageal reflux before and after sleeve gastrectomy using symptom scoring, scintigraphy, and endoscopy. Surg Obes Relat Dis. 2014;10(4):600–5.
Rebecchi F, Allaix ME, Giaccone C, et al. Gastroesophageal reflux disease and laparoscopic sleeve gastrectomy: a physiopathologic evaluation. Ann Surg. 2014;260(5):909–14.
Peterli R, Wölnerhanssen BK, Peters T, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity: the SM-BOSS randomized clinical trial. JAMA. 2018;319(3):255–65.
Genco A, Soricelli E, Casella G, et al. Gastroesophageal reflux disease and Barrett’s esophagus after laparoscopic sleeve gastrectomy: a possible, underestimated long-term complication. Surg Obes Relat Dis. 2017;13(4):568–74.
Sebastianelli L, Benois M, Iannelli A, et al. Systematic endoscopy 5 years after sleeve gastrectomy results in a high rate of Barrett’s esophagus: results of a multicenter study. Obes Surg. 2019;29(5):1462–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Statement of Human and Animal Rights and Informed Consent
“Informed consent was obtained from all individual participants included in the study.”
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Amor, I.B., Casanova, V., Vanbiervliet, G. et al. The Nissen-Sleeve (N-Sleeve): Results of a Cohort Study. OBES SURG 30, 3267–3272 (2020). https://doi.org/10.1007/s11695-020-04469-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04469-5