Abstract
Introduction/Purpose
Bariatric surgery (BS) has emerged as a cornerstone procedure to prevent and treat obesity-related comorbidities. As the Hispanic population continues to grow in the USA, their importance to the healthcare system cannot be understated. We aimed to assess the use of BS and related healthcare outcomes in Hispanics using a national database.
Materials and Methods
Case-control study using the 2010 to 2014 National Inpatient Sample datasets. BS use in Hispanics compared to non-Hispanics was the primary outcome. Secondary outcomes included inpatient mortality, morbidity, resource use, length of hospital stay, hospital costs, and total hospitalization charges. Propensity scores were used to match Hispanic patients with BS with non-Hispanic patients with BS using sex, age, and Charlson Comorbidity Index as covariates. A multivariate model was then used to adjust for additional confounding factors.
Results
From the 105,435 patients who underwent BS, a propensity-matched cohort of 20,440 was created (10,945 Hispanics). Mean (SD) age was 45 (17.2) years, and 73,594 (69.8%) were women. The prevalence of BS in Hispanics was 21/100,000 persons (281/100,000 admissions) compared to 36/100,000 persons (337/100,000 admissions) for non-Hispanics. On multivariate analysis, Hispanics displayed adjusted propensity-matched odds of 0.88 of having BS (P < 0.01). No differences were seen in the surgical approach performed. Hispanics and non-Hispanics had similar mortality, morbidity, hospital length of stay, and costs.
Conclusion
Despite higher obesity rates, the use of BS is lower in Hispanics. For those who underwent BS, no difference in clinical outcomes and minor differences in resource use were observed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hispanics are disproportionately affected by extreme obesity and associated comorbidities [1]. In 2003, Hispanics became the largest ethnic minority in the USA, surpassing African Americans (18.1% vs 13.4% of the total population according to the National Census, respectively) [2, 3]. Furthermore, the Hispanic population continues to grow faster than any other ethnic group in the USA, for which its importance to the healthcare system cannot be understated.
Bariatric surgery (BS) is now a well-established treatment with proven efficacy in weight reduction; improved management of diabetes mellitus, hypertension, and steatohepatitis; and reduced rates of other obesity-related adverse effects, even long-term mortality [4]. Disparities in access to BS have been reported in different ethnic minorities in the USA [5, 6].
There is conflicting evidence on how ethnicity affects BS acceptance, clinical outcomes, adverse effects, healthcare utilization, and economic impact. Most studies suggest decreased BS use and decreased response to treatment in ethnic minorities [7, 8]; however, a study published in 2015 showed no ethnic differences in patients who underwent BS after adjusting for multiple socioeconomic factors [5]. Among those who underwent surgery, comorbidity burden was comparable between all ethnic minorities and white patients [5].
To date, no national study has examined the effect of Hispanic ethnicity in the use of BS, clinical outcomes, and economic implications. For this reason, we aimed to explore the use of BS among Hispanics in the USA, as well as several outcomes (i.e., inpatient mortality, morbidity, resource utilization and inpatient economic burden) using a national database.
Materials and Methods
Study Design and Data Source
We performed a cross-sectional analysis of the National Inpatient Sample (NIS), a database developed and overseen by the Healthcare Cost and Utilization Project (HCUP), which is sponsored by the Agency for Healthcare Research and Quality (AHRQ) under the US Department of Health and Human Services. The NIS is the largest publically available, inpatient, all-payer database in the USA. The examined datasets for the years 2010 to 2014 contain data from January 2010 to December 2014 on more than 35 million inpatient admissions. These admissions are a 20% stratified sample of over 4000 nonfederal acute care hospitals from more than 40 states and are representative of 95% of hospital discharges nationwide [9].
The NIS provides a principal diagnosis, defined as the primary discharge diagnosis, as well as 24 other secondary diagnoses in the dataset. The dataset also includes codes for up to 15 procedures performed during the hospital stay. It allows determining the length of hospital stay, hospitalization costs, and total hospitalization charges [10] and permits calculations of inpatient disease prevalence, which is the relative frequency of a condition coded as a discharge diagnosis.
Patient Population
All patients with International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) procedural code for BS (i.e., 43.89, 44.95, 44.93, 44.69, 44.68, 45.91, 44.93, 45.51, 44.39, 43.7, 44.38, and 44.95) were included in the study. Patients were stratified by different surgery subtypes by associating additional ICD-9-CM codes. Only patients under 18 years of age were excluded.
Definition of Variables
Effect-modifying variables were classified as patient characteristics (i.e., age, sex, ethnicity, insurance status, income in patient zip code) and hospital characteristics (i.e., region, urban location, teaching status, number of beds). According to the US Census Bureau, the USA is divided into four distinct geographic regions: Northeast, South, Midwest, and West. Data from every patient’s vital status at the end of hospitalization, length of hospital stay measured in days, hospital costs, and total hospitalization charges were extracted from the dataset. The Deyo adaptation of the Charlson Comorbidity Index, a validated tool for dataset analysis, was used to control for existing comorbidities [11].
Outcomes
The primary outcome of this study was the general and inpatient prevalence of BS in Hispanic patients when compared to patients of other ethnicities (non-Hispanic). Furthermore, odds of BS use were stratified by all effect-modifying variables (i.e., patient and hospital characteristics). Secondary outcomes were inpatient mortality, morbidity (i.e., shock, multiorgan failure, intensive care unit stay, and total parenteral nutrition [TPN] use), imaging use (i.e., abdominal ultrasound, abdominal computed tomography, and endoscopic retrograde cholangiopancreatography), surgeries performed, length of hospital stay, hospitalization charges, and hospital costs. Hospitalization charges correspond to the financial resources billed by the institution, while hospital costs are the net amount of money invested by the institution in patient care. The HCUP provides cost-to-charge ratios for each admission, which is multiplied by the total charges to obtain costs. Both costs and charges were adjusted for inflation using the Consumer Price Index.
Statistical Analysis
Discharge-level weights published by the HCUP were used to estimate the number of patients undergoing BS. Fisher’s exact test was used to compare proportions and Student’s t test was used to compare means. Propensity score was used to create two matching cohorts in patients who underwent BS: Hispanics and non-Hispanics. Table 1 shows the baseline characteristics of the cohorts before matching, while Table 2 shows the baseline characteristics after matching. A multivariate regression model was created to calculate propensity scores with the following covariates: sex, age, Charlson Comorbidity Index, insurance status, median income in the patient’s zip code, and hospital region, urban location, number of beds, and teaching status. Population estimates were obtained from the National Census Bureau. All statistical analyses were conducted using STATA, Version 13 (StataCorp LLC).
Results
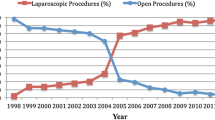
A total of 666,854 patients underwent BS during the study period: 463,464 (69.5%) were white; 98,694 (14.8%), African-American; 92,025 (13.8%), Hispanic; and 12,670 (1.9%), other. A propensity-matched cohort of 20,440 patients was created, of which 10,945 were Hispanics. Mean (SD) patient age was 45 (17.2) years, and 73,594 (69.8%) were women. The prevalence of BS in Hispanics was 21/100,000 persons (281/100,000 admissions) compared to 36/100,000 persons (337/100,000 admissions) for non-Hispanics (Fig. 1) [12].
On multivariate analysis, Hispanics displayed adjusted propensity-matched odds of 0.88 (P < 0.01) of having BS when compared to non-Hispanic, but there was no difference in odds of specific subtype of surgery. All outcomes are displayed in Tables 3 and 4.
Secondary Outcomes
Hispanics undergoing BS did not display different mortality, morbidity, or hospital length of stay compared to non-Hispanics (Tables 3 and 4). Likewise, there was no difference in subtype of BS performed when compared to non-Hispanics. However, on sub-stratification for surgery type, Hispanic patients undergoing RYGB did display increased odds of undergoing CT abdomen and additional adjusted hospital costs, charges, and length of hospital stay compared to non-Hispanics. Hispanic patients who underwent sleeve gastrectomy displayed decreased odds of TPN and multiorgan failure, while having increased odds of undergoing abdominal ultrasound when compared to non-Hispanics (Tables 3 and 4).
Discussion
Our study suggests that Hispanics are less likely to undergo BS in the USA. The NIS is the largest inpatient database available in the country, with representation of 20% of all hospitalizations, stratified by geographic location, thus reducing the chances of selection bias. The creation of propensity-matched cohorts further reduces selection bias. We have adhered to the recommendations on Methodological Standards in Research Using the NIS published by Khera et al. [13].
Our findings parallel the published literature, showing that ethnic disparities are not only present in obesity and obesity-related comorbidities but also in access to effective treatments for obesity. Greater than two-thirds of patients undergoing BS were from the southern and western regions of the USA, which reflect the higher rates of observed obesity in those locations [14]. Our findings are in exact concordance to this geographic distribution observed in other studies, as more than two-thirds of the patient population undergoing BS was from the southern and western regions of the USA. In addition, the majority of patients in both study cohorts underwent BS at urban teaching hospitals with large hospital volume. Although there were statistical differences between the cohorts in terms of hospital characteristics, it is the author’s opinion that these are not clinically significant.
The higher incidence of obesity in Hispanics can be explained by genetics, diet, amount of physical activity, psychosocial factors, and income [1, 7]. Some risk factors are present as early as the preschool years. Access to BS, however, is determined by sociocultural factors (e.g., self-perceived obesity, health literacy), healthcare access (e.g., geography, insurance status, language barriers, and socioeconomic status), and even psychosocial stress. Although there were no differences between the Hispanic and non-Hispanic cohorts after matching in terms of insurance coverage, the cohorts did differ in the pre-matching setting. Proportionately, more Hispanics were on Medicaid coverage and less so on Medicare when compared to non-Hispanics. Overall, the cohort of Hispanics was composed of proportionately more patients with low median income, which may evidence another factor contributing to the disparity. A telephone survey showed that Hispanics are more willing to consider BS than non-Hispanic after adjustment for body mass index (BMI) and sociodemographics. Strategies to increase the use of BS in Hispanics should be multidisciplinary and include awareness campaigns, education, and improved access to BS centers.
A “Hispanic Obesity Paradox” has been reported in the literature and suggests that despite having higher rates of obesity, Hispanics display an average of two additional years in life expectancy compared to white patients [15, 16]. This study could not evaluate this factor, as the only outcomes it examines are the ones during the index admission for bariatric surgery. Therefore, a study examining long-term outcomes in Hispanic patients who underwent BS would be warranted to appropriately address this issue.
There is debate on the impact of ethnicity in clinical outcomes following BS. Some reports show decreased reduction on metabolic syndrome and less improvement in lipid profile in Hispanics [17, 18]. Another study shows no difference in percent of excess weight loss or perioperative mortality among Hispanics compared to non-Hispanics [19]. Current analysis reveals that, despite lower use of BS, clinical outcomes (i.e., mortality and complications) and healthcare use were similar between our study groups. Increased research spending, awareness, and access to treatment in Hispanics are proposed to combat the alarming obesity epidemic and prevent increasing disparities [7].
Our study has limitations inherent to retrospective research. The ICD-9-CM code for BS has not been validated but is clearly identified in hospital coding. No stratification was made between indications for BS (e.g., BMI or BMI with adverse effects). Despite our matching efforts and statistical approach, stratification and sampling bias cannot be totally prevented in any analysis of administrative data [13]. Khera et al. [13] have raised concerns of performing NIS analysis in data collected after 2011 due to a frame shift on the hospital pool that share data with HCUP. We have accounted for these changes by assigning new weights to patients on a year-by-year basis, which is a valid methodology recommended by HCUP [13]. Lastly, inpatient medication use or outpatient costs incurred by BS could not be estimated.
Conclusion
Despite higher obesity rates seen in Hispanics, their use of BS is lower in a national sample. This finding suggests ethnic disparities in access to BS. For those who underwent BS, no difference in inpatient mortality, morbidity, or resource use was observed, further illustrating that the factors affecting BS use in Hispanics are probably related to healthcare access, personal beliefs, socioeconomics, or other cultural factors rather than biologic differences and clinical variables. Further studies are needed to identify the specific factors that compose these disparities, measure their impact, and trace the best strategies to assess them.
References
KYZ F, Leeds MJ, Ufelle AC. Epidemiology of obesity in the Hispanic adult population in the United States. Fam Community Health. 2017;40(4):291–7. https://doi.org/10.1097/FCH.0000000000000160.
U.S. Department of Commerce EaSA. Population profile of the United States: dynamic version. Living, working, and growing in the USA: U.S. Census Bureau; 2003. Available from: https://www.census.gov/population/pop-profile/dynamic/profiledynamic.pdf. Accessed Feb 27 2019.
Clemetson L. Hispanics now largest minority, census shows. The New York Times. 2003; 1/22/2003:A00001.
Arterburn DE, Olsen MK, Smith VA, et al. Association between bariatric surgery and long-term survival. JAMA. 2015;313(1):62–70. https://doi.org/10.1001/jama.2014.16968.
Stanford FC, Jones DB, Schneider BE, et al. Patient race and the likelihood of undergoing bariatric surgery among patients seeking surgery. Surg Endosc. 2015;29(9):2794–9. https://doi.org/10.1007/s00464-014-4014-8.
Wee CC, Huskey KW, Bolcic-Jankovic D, et al. Sex, race, and consideration of bariatric surgery among primary care patients with moderate to severe obesity. J Gen Intern Med. 2014;29(1):68–75. https://doi.org/10.1007/s11606-013-2603-1.
Byrd AS, Toth AT, Stanford FC. Racial disparities in obesity treatment. Curr Obes Rep. 2018;7(2):130–8. https://doi.org/10.1007/s13679-018-0301-3.
Sudan R, Winegar D, Thomas S, et al. Influence of ethnicity on the efficacy and utilization of bariatric surgery in the USA. J Gastrointest Surg. 2014;18(1):130–6. https://doi.org/10.1007/s11605-013-2368-1.
Khera R, Krumholz HM. With great power comes great responsibility: big data research from the National Inpatient Sample. Circ Cardiovasc Qual Outcomes. 2017;10(7):e003846. https://doi.org/10.1161/CIRCOUTCOMES.117.003846.
HCUP Databases. Healthcare cost and utilization project—overview of the National (Nationwide) Inpatient Sample (NIS) Agency for Healthcare Research and Quality. Rockville, MD. 2016.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–9.
Kroner PT, Koop A, Stewart M, et al. 792—Hispanic ethnicity is associated with decreased odds of bariatric surgery: a nationwide analysis. Gastroenterology. 2018;154(6, Supplement 1):S-1358–S-9. https://doi.org/10.1016/S0016-5085(18)34444-5.
Khera R, Angraal S, Couch T, et al. Adherence to methodological standards in research using the National Inpatient Sample. JAMA. 2017;318(20):2011–8. https://doi.org/10.1001/jama.2017.17653.
Le A, Judd SE, Allison DB, et al. The geographic distribution of obesity in the US and the potential regional differences in misreporting of obesity. Obesity (Silver Spring). 2014;22(1):300–6. https://doi.org/10.1002/oby.20451.
Istfan N, Anderson WA, Apovian C, et al. Racial differences in weight loss, hemoglobin A1C, and blood lipid profiles after Roux-en-Y gastric bypass surgery. Surg Obes Relat Dis. 2016;12(7):1329–36. https://doi.org/10.1016/j.soard.2015.12.028.
Coleman KJ, Huang YC, Koebnick C, et al. Metabolic syndrome is less likely to resolve in Hispanics and non-Hispanic blacks after bariatric surgery. Ann Surg. 2014;259(2):279–85. https://doi.org/10.1097/SLA.0000000000000258.
Dominguez K, Penman-Aguilar A, Chang MH, et al. Vital signs: leading causes of death, prevalence of diseases and risk factors, and use of health services among Hispanics in the United States: 2009-2013. MMWR Morb Mortal Wkly Rep. 2015;64(17):469–78.
Hainer V, Aldhoon-Hainerová I. Obesity paradox does exist. Diabetes Care. 2013;36(Suppl 2):S276–81. https://doi.org/10.2337/dcS13-2023.
Elli EF, Gonzalez-Heredia R, Patel N, et al. Bariatric surgery outcomes in ethnic minorities. Surgery. 2016;160(3):805–12. https://doi.org/10.1016/j.surg.2016.02.023.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflict of interests.
Ethics Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. For this type of study, formal consent was not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Portions of this manuscript have been published in abstract form: Kroner PT, Koop A, Stewart M, Lukens F. 792—Hispanic ethnicity is associated with decreased odds of bariatric surgery: a nationwide analysis. Gastroenterology. 2018;154(6, Supplement 1):S-1358-S-9.
Rights and permissions
About this article
Cite this article
Kröner Florit, P.T., Corral Hurtado, J.E., Wijarnpreecha, K. et al. Bariatric Surgery, Clinical Outcomes, and Healthcare Burden in Hispanics in the USA. OBES SURG 29, 3646–3652 (2019). https://doi.org/10.1007/s11695-019-04047-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-04047-4