Abstract
Background
Bariatric surgery reduces atherosclerotic cardiovascular disease (ASCVD) risk. However, the comparative effect of Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG) on 10-year and lifetime ASCVD risk, as defined by the American College of Cardiology/American Heart Association (ACC/AHA), remains unknown.
Methods
Using the ACC/AHA ASCVD risk estimator, 10-year and lifetime ASCVD risks were calculated before and 1 year after bariatric surgery for patients aged 40–78 who underwent RYGB or SG at an academic medical center in California between 2003 and 2015. Change in risk was calculated by taking the difference between 1-year and baseline risk. Statistical analyses included the Wilcoxon signed rank test, Mann-Whitney U test, Quade’s test, and multiple logistic regression.
Results
There were 536 patients (mean age 52 ± 10 years, 20% male), of whom 438 underwent RYGB and 98 underwent SG. Patients undergoing RYGB were predominately female (82% vs 71%, p = 0.021) and had higher baseline BMIs (44.4 ± 8.4 vs 41.9 ± 8.0, p < 0.001) than patients undergoing SG. Compared with baseline, 10-year and lifetime ASCVD risks were significantly lower 1 year after surgery (aggregate of RYGB and SG, 4.2 ± 6.0% vs. 2.2 ± 3.5%, p < 0.001; 50 ± 11% vs. 39 ± 12%, p < 0.001, respectively). Patients who underwent RYGB had greater reductions in 10-year and lifetime ASCVD risks from baseline to 1 year after surgery than patients who underwent SG (1.7 ± 3.5% vs. 0.8 ± 2.4%, p < 0.001; 11 ± 23% vs. 0 ± 12%, p < 0.001, respectively).
Conclusions
Although RYGB and SG significantly lower 10-year and lifetime cardiovascular disease risks by 1 year after surgery, patients who undergo RYGB may experience greater cardiovascular risk reduction relative to counterparts who undergo SG.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Atherosclerotic cardiovascular disease (ASCVD) is the leading cause of morbidity and mortality in the USA. In 2013, the American Heart Association (AHA) and American College of Cardiology (ACC) released guidelines that aimed to reduce ASCVD risk through evidence-based recommendations [1, 2]. To achieve this goal, the Pooled Cohort Risk Assessment Equation was developed to risk stratify patients who could benefit from cholesterol-lowering therapies [3]. This equation incorporates known ASCVD risk factors to estimate 10-year and lifetime ASCVD risks, defined as coronary death, non-fatal myocardial infarction, or fatal/non-fatal stroke, and it is intended to inform patient-provider discussions around lifestyle modifications and statin initiation. This ASCVD risk estimator is widely used in clinical practice today and has been well-validated against observed ASCVD events in several studies [4, 5].
Obesity is a well-known independent risk factor for ASCVD and is closely related to other traditional ASCVD risk factors, including type 2 diabetes mellitus, hypertension, and dyslipidemia [6]. As its prevalence has risen substantially over the last few decades, obesity has become a target for intervention to reduce ASCVD risk. Bariatric surgery is an effective treatment for morbid obesity [7, 8], and the two most frequently performed procedures are Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG). In 2015, RYGB and SG accounted for 23.1% and 53.8% of all bariatric surgical procedures, respectively [9]. In previous studies, both RYGB and SG have been shown to reduce the prevalence of diabetes [10,11,12], hypertension [13], and dyslipidemia [14]. Although some studies have found that RYGB may have a greater effect on the reduction of these comorbidities [10, 11, 14] and on long-term weight loss [15], this is not a consistent finding [12, 13, 16, 17]. To better understand the impact of bariatric procedures on ASCVD risk, we compared the effect of laparoscopic RYGB and laparoscopic SG on the change in ACC/AHA 10-year and lifetime ASCVD risks from prior to surgery to 1 year after surgery at a single academic medical center.
Methods
Data for this study were obtained from a prospectively maintained database containing clinical information for patients who underwent RYGB or SG at Stanford University Hospital in California between 2003 and 2015. Inclusion criteria included successful completion of surgery with 1 year of data available. Patients were excluded from analysis if they required a re-operation after their initial surgery, had incomplete ASCVD risk data, or had unacceptable values for ASCVD risk calculation as defined in Fig. 1. Data were collected from patients who provided written informed consent, and approval for this study was provided by the Stanford University Institutional Review Board.
The RYGB technique involved the direct anastomosis of a small gastric pouch to the jejunum allowing food to bypass part of the small intestine and a jejuno-jejunal anastomosis for the flow of exocrine secretions [18]. In SG, a portion of the stomach along its greater curvature was excised, leaving a small gastric remnant for food to travel through to the duodenum [19].
Variables used to calculate ACC/AHA 10-year and lifetime ASCVD risks included age, sex, race (White, African American, or other), total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), systolic blood pressure (SBP), the presence of diabetes, hypertension treatment, and tobacco use. Baseline and 1-year measures of these variables and body mass index (BMI) were collected from the existing database and from a review of individual electronic health records. BMI was calculated by weight (kilograms) divided by height (meters) squared. Classifications of obesity were defined using preoperative BMI as follows: super obesity (BMI ≥ 50 kg/m2), severe obesity (40 kg/m2 ≤ BMI < 50 kg/m2), and morbid obesity (35 kg/m2 ≤ BMI < 40 kg/m2). Because of an institutional requirement for smoking cessation prior to undergoing bariatric surgery, patients were recorded to be non-smokers at both time points. Diabetes was defined as hemoglobin A1c ≥ 6.5% or use of an anti-diabetic medication. Resolution of diabetes was defined as hemoglobin A1c < 6.5% and not taking any diabetes medications 1 year after surgery. Ten-year and lifetime ASCVD risks were estimated at baseline and 1 year after bariatric surgery using the ACC/AHA Pooled Cohort Risk Assessment Equation [3]. The change in ASCVD risk was calculated by taking the difference between 1-year and baseline risks. For valid calculated risk estimation, variables had to be within the following ranges: age 40–79 years (or 40–59 years for lifetime ASCVD estimation), TC 130–320 mg/dL, HDL-C 20–100 mg/dL, and SBP 90–200 mmHg.
Results are expressed as medians with interquartile ranges and count frequencies with percentages unless otherwise specified. Continuous variables were analyzed using Wilcoxon signed rank, Mann-Whitney U, and Quade’s tests, whereas categorical variables were analyzed using the chi-squared test. Logistic regression was used in a sub-group analysis to assess the likelihood of patients achieving a 10-year ASCVD risk < 7.5% 1 year after surgery in the RYGB and SG groups. This metric is clinically relevant, since ACC/AHA guidelines recommend initiation of statin therapy for primary prevention in patients for whom 10-year ASCVD risk ≥ 7.5%. Variables in the logistic regression included preoperative age, sex, BMI, and diabetes. For all statistical analyses, a two-sided p value ≤ 0.05 was considered statistically significant. All analyses were done using SPSS (Version 24.0, IBM Corp., Armonk, NY) and SAS Studio v3.5.
Results
The final analysis included 536 patients, of whom 438 underwent RYGB and 98 underwent SG. The median age was 52 years, 20% were male, and 61% were White. At baseline, 47% had diabetes and 70% took medications for hypertension. Patients undergoing RYGB were more likely to be female (82% vs 71%, p = 0.021), had higher baseline BMIs (44.4 ± 8.4 kg/m2 vs 41.9 ± 8.0 kg/m2, p < 0.001), and greater SBPs (138 ± 28 mmHg vs 132 ± 23 mmHg, p = 0.004) relative to patients undergoing SG. Baseline 10-year and lifetime ASCVD risks were comparable between the two groups (4.2 ± 5.9% for RYGB vs 4.4 ± 6.6% for SG, p = 0.548; 48 ± 11% for RYGB vs 50 ± 12% for SG, p = 0.257, respectively). Table 1 summarizes additional baseline characteristics of the study sample.
After accounting for differences in baseline BMI, sex distribution, and SBP, RYGB still resulted in larger reductions in BMI (− 14.5 ± 5.3 kg/m2 vs − 8.5 ± 4.1 kg/m2, p < 0.001) and TC (− 16 ± 46 mg/dL vs − 8 ± 45 mg/dL, p < 0.001) compared with SG. Patients who underwent RYGB were more likely to experience remission of diabetes relative to patients who underwent SG (80% vs 56%, p < 0.001) 1 year after surgery. In addition, more patients stopped their anti-hypertensives after RYGB than SG (71% vs 49%, p < 0.001). RYGB and SG were associated with similar increases in HDL-C (10 ± 14 mg/dL vs 8 ± 13 mg/dL, p = 0.135) and decreases in SBP (− 10 ± 29 mmHg vs − 3 ± 27 mmHg, p = 0.164).
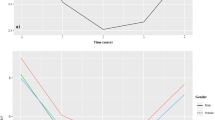
Compared with baseline, 10-year and lifetime ASCVD risks were significantly lower 1 year after bariatric surgery (defined as the aggregate of RYGB and SG, 4.2 ± 6.0% vs. 2.2 ± 3.5%, p < 0.001; 50 ± 11% vs. 39 ± 12%, p < 0.001, respectively). This is illustrated for 10-year ASCVD risk in Fig. 2. Individually, both RYGB and SG led to statistically significant reductions in 10-year ASCVD risk (4.2 ± 5.9% vs. 1.9 ± 3.2%, p < 0.001; 4.4 ± 6.6% vs. 3.2 ± 5.0%, p < 0.001, respectively) and lifetime ASCVD risk (48 ± 11% vs. 39 ± 12%, p < 0.001; 50 ± 12% vs. 39 ± 10%, p < 0.001, respectively). However, after accounting for group differences in BMI reduction and preoperative BMI, sex distribution, and SBP, patients who underwent RYGB had larger reductions in 10-year and lifetime ASCVD risks from baseline to 1 year after surgery than those who underwent SG (1.7 ± 3.5% vs. 0.8 ± 2.4%, p < 0.001; 11 ± 23% vs. 0 ± 12%, p < 0.001, respectively). This is illustrated for 10-year ASCVD risk in Fig. 3.
Median 10-year ASCVD risk at baseline and 1-year after surgery, total and by surgery type. NS, non-significant difference between baseline 10-year ASCVD risk for RYGB and SG. Asterisk symbol indicates significant difference between 10-year ASCVD risk 1 year after RYGB versus SG. ASCVD, atherosclerotic cardiovascular disease; RYGB, Roux-en-Y gastric bypass; SG, sleeve gastrectomy
For patients with a baseline 10-year ASCVD risk ≥ 7.5%, the odds of achieving a 10-year risk < 7.5% were 69% lower for those who underwent SG relative to those who underwent RYGB (adjusted OR for SG = 0.31, 95% CI 0.12–0.85, p = 0.023) after adjusting for preoperative age, BMI, sex distribution, and diabetes (Table 2). The unadjusted odds for achieving this target (OR = 0.24, 95% CI 0.11–0.56, p = 0.001) were similar to the adjusted odds above.
Greater reductions in 10-year ASCVD risk after RYGB compared with SG were observed among female patients (1.5 ± 2.9% vs. 0.5 ± 2.2%, p < 0.001), patients who had severe obesity (1.3 ± 2.6% vs. 0.3 ± 2.0%, p < 0.001) and morbid obesity (1.7 ± 3.9 vs. 1.4 ± 2.7, p = 0.05), and patients who were younger than 60 years of age (1.5 ± 3.1% vs. 0.6 ± 2.3%, p < 0.001). Surprisingly, preoperative diabetes status did not significantly impact the comparative effect as both diabetic and non-diabetic patients experienced greater 10-year ASCVD risk reduction if they underwent RYGB (Table 3).
Postoperative complications occurred in 52 patients—47 who underwent RYGB and 5 SG. For patients who underwent RYGB, complications included clinically significant bleeding requiring a blood transfusion (13), gastrointestinal ulcer (9), wound infection (8), nutritional deficiency (8), arrhythmia (5), pneumonia (5), venous thromboembolism (4), stroke (1), and bowel obstruction/ileus (1). Patients who underwent SG developed venous thromboembolism (3), clinically significant bleeding (1), and nutritional deficiency (1).
Discussion
The purpose of this study was to assess the comparative effectiveness of RYGB and SG on 10-year and lifetime ASCVD risks, as defined by the ACC/AHA Pooled Cohort Risk Assessment Equation, 1 year after surgery. While both RYGB and SG were associated with significant reductions in the 10-year and lifetime risks of ASCVD, RYGB was associated with greater reductions than SG. Greater reductions in risk among patients who underwent RYGB vs. SG were largely driven by patients who were female, had BMIs 35–50 kg/m2, and were younger than 60 years of age, although sub-group analyses should be interpreted cautiously due to small sample sizes. Notably, patients with elevated baseline 10-year ASCVD risk were more likely to achieve a 10-year ASCVD risk < 7.5% 1 year after surgery if they underwent RYGB rather than SG. Postoperative complications were more likely after RYGB than SG, although no patients suffered a postoperative myocardial infarction.
Overall, these findings were attributable to greater ASCVD risk factor reduction in the RYGB group. Compared with SG, RYGB not only caused a larger reduction in TC, but also resulted in greater remission of diabetes and decreased utilization of anti-hypertensives. Patients who underwent RYGB also experienced more weight loss than those who underwent SG, although the group differences in ASCVD risk reduction were persistent after accounting for this finding. As previously described, RYGB may have a greater effect on weight loss and metabolic syndrome remission due to bypass of the proximal small intestine leading to decreased nutrient contact with the duodenum and proximal jejunum. This is thought to prevent secretion of an unidentified “anti-incretin,” a signal that otherwise promotes insulin resistance [20].
The results of this study demonstrate a 54% and 30% relative reduction in 10-year ASCVD risk after RYGB and SG, respectively, and are comparable with results from prior studies that have examined the effect of bariatric surgery on the Framingham risk score [21], which estimates the 10-year risk of myocardial infarction, coronary death, and adverse cardiovascular events. For example, Torquati et al. [22] estimated that RYGB led to a reduction in 10-year cardiovascular risk, as defined by the Framingham risk score, from 5.4 to 2.7% (50% relative risk reduction) 1 year after surgery. Similarly, two large prospective cohort studies [23, 24] found that the incidence of myocardial infarction and coronary death over an average of 7–10 years was reduced by ~ 50% after RYGB compared with medical management. While cardiovascular risk after SG has not been well studied, a prospective cohort study of 140 Spanish patients by Benaiges et al. [25] found that 10-year cardiovascular risk, as measured by the Framingham risk score, decreased from 5.6 to 3.4% (equivalent to a 39% relative risk reduction) 1 year after SG.
To our knowledge, this study is first to quantify changes in ASCVD risk for bariatric patients in a way that can be used to inform clinical decisions and patient-provider discussions in current practice. Since the 2013 ACC/AHA cholesterol guideline [1] recommended use of the Pooled Cohort Equation to estimate 10-year and lifetime ASCVD risks, it has become integrated into clinical practice as a quantitative way to effectively risk stratify patients when determining statin eligibility. Currently, patients with 10-year ASCVD risk ≥ 7.5% are considered eligible for statin therapy. No previous studies have analyzed the impact of bariatric surgery—specifically, RYGB and SG—on ACC/AHA 10-year and lifetime ASCVD risks. Understanding the impact of these common procedures on a clinically relevant risk assessment tool and in a high-risk population is important for understanding the role of bariatric surgery in the prevention and treatment of ASCVD. Our results demonstrate that RYGB may be more effective than SG in reducing overall ASCVD risk, particularly in lower risk sub-groups.
There are several limitations to the present study. First, patients were recorded to be non-smokers prior to and following bariatric surgery based on institutional requirements. Although patients were asked preoperatively and during follow-up to confirm smoking cessation and were deemed non-operative candidates if they were suspected to have continued smoking, it is possible that some patients continued smoking without provider knowledge. Second, due to the observational study design, it is possible that the observed differences in ASCVD risk reduction following RYGB and SG may be due to residual confounding not accounted for by our analyses, and it is not possible to ascertain causality. Third, a significant proportion of patients were excluded for values outside the range of ASCVD risk estimation, which limits the external validity of our findings. Fourth, this study only includes follow-up data for 1 year after bariatric surgery. In the future, it will be important to conduct similar investigations using longer term outcomes.
Conclusion
RYGB and SG are both associated with significantly lower 10-year and lifetime cardiovascular disease risk 1 year after surgery, but patients undergoing RYGB experienced greater cardiovascular risk reduction than those undergoing SG. Randomized controlled trials are needed to evaluate the comparative effect of different bariatric procedures on ASCVD risk and events.
References
Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2889–934.
Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013;63:2960–84.
Goff DC, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk. Circulation. 2013;63:2935–59.
Muntner P, Colantonio LD, Cushman M, et al. Validation of the atherosclerotic cardiovascular disease pooled cohort risk equations. JAMA. 2014;311(14):1406–15.
Loprinzi PD, Addoh O. Predictive validity of the American College of Cardiology/American Heart Association pooled cohort equations in predicting all-cause and cardiovascular disease-specific mortality in a National Prospective Cohort Study of adults in the United States. Mayo Clin Proc. 2016;91(6):763–9.
Jensen MD, Ryan DH, Apovian CM, et al. AHA/ACC/TOS guideline for the management of overweight and obesity in adults. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. 2014. 2013;129(25 suppl 2):S102–S38.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
DeMaria EJ. Bariatric surgery for morbid obesity. N Engl J Med. 2007;356(21):2176–83.
Ponce J, DeMaria EJ, Nguyen NT, et al. American Society for Metabolic and Bariatric Surgery estimation of bariatric surgery procedures in 2015 and surgeon workforce in the United States. Surg Obes Relat Dis. 2016;12(9):1637–9.
Li J-F, Lai D-D, Ni B, et al. Comparison of laparoscopic Roux-en-Y gastric bypass with laparoscopic sleeve gastrectomy for morbid obesity or type 2 diabetes mellitus: a meta-analysis of randomized controlled trials. Can J Surg. 2013;56(6):E158–E64.
Yska J, van Roon EN, de Boer A, et al. Remission of type 2 diabetes mellitus in patients after different types of bariatric surgery: a population-based cohort study in the United Kingdom. JAMA Surg. 2015;150(12):1126–33.
Cho J-M, Kim HJ, Menzo EL, et al. Effect of sleeve gastrectomy on type 2 diabetes as an alternative treatment modality to Roux-en-Y gastric bypass: systemic review and meta-analysis. Surg Obes Relat Dis. 2015;11(6):1273–80.
Nassour I, Almandoz JP, Adams-Huet B, et al. Metabolic syndrome remission after Roux-en-Y gastric bypass or sleeve gastrectomy. Diabetes Metab Syndr Obes. 2017;10:393–402.
Spivak H, Sakran N, Dicker D, et al. Different effects of bariatric surgical procedures on dyslipidemia: a registry-based analysis. Surg Obes Relat Dis. 2017;13(7):1189–94.
Maciejewski ML, Arterburn DE, Van Scoyoc L, et al. Bariatric surgery and long-term durability of weight loss. JAMA Surg. 2016;151(11):1046–55.
Peterli R, Wölnerhanssen B, Peters T, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-y gastric bypass on weight loss in patients with morbid obesity: the sm-boss randomized clinical trial. JAMA. 2018;319(3):255–65.
Salminen P, Helmiö M, Ovaska J, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-y gastric bypass on weight loss at 5 years among patients with morbid obesity: the sleevepass randomized clinical trial. JAMA. 2018;319(3):241–54.
Olbers T, Lönroth H, Fagevik-Olsén M, et al. Laparoscopic gastric bypass: development of technique, respiratory function, and long-term outcome. Obes Surg. 2003;13(3):364–70.
Rosenthal RJ. International sleeve gastrectomy expert panel consensus statement: best practice guidelines based on experience of >12,000 cases. Surg Obes Relat Dis. 2012;8(1):8–19.
Pok E-H, Lee W-J. Gastrointestinal metabolic surgery for the treatment of type 2 diabetes mellitus. World J Gastroenterol: WJG. 2014;20(39):14315–28.
Wilson PWF, D’Agostino RB, Levy D, et al. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837–47.
Torquati A, Wright K, Melvin W, et al. Effect of gastric bypass operation on Framingham and actual risk of cardiovascular events in class II to III obesity. J Am Coll Surg. 2007;204(5):776–82.
Sjöström L, Narbro K, Sjöström CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357(8):741–52.
Adams TD, Gress RE, Smith SC, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357(8):753–61.
Benaiges D, Goday A, Ramon JM, et al. Laparoscopic sleeve gastrectomy and laparoscopic gastric bypass are equally effective for reduction of cardiovascular risk in severely obese patients at one year of follow-up. Surg Obes Relat Dis. 2011;7(5):575–80.
Author information
Authors and Affiliations
Contributions
V.R. performed data analysis and wrote the manuscript. L.G. assisted with data analysis and reviewed the manuscript. D.M. contributed to the research design and revised the manuscript. J.M. provided the data and critical review of the manuscript. J.M. and D.M. conceived of study. All authors agree with the contents of this manuscript.
Corresponding author
Ethics declarations
Data were collected from patients who provided written informed consent, and approval for this study was provided by the Stanford University Institutional Review Board.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Raygor, V., Garcia, L., Maron, D.J. et al. The Comparative Effect of Roux-en-Y Gastric Bypass and Sleeve Gastrectomy on 10-Year and Lifetime Atherosclerotic Cardiovascular Disease Risk. OBES SURG 29, 3111–3117 (2019). https://doi.org/10.1007/s11695-019-03948-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03948-8