Abstract
Aim
To evaluate the association of moderate-to-intense physical activity with the effects of bariatric surgery on weight loss, level of activities of daily living, dyspnea, and quality of life in sedentary individuals with grade II and III obesity.
Method
Seventy-eight candidates for bariatric surgery were evaluated for anthropometry, dyspnea, quality of life, level of activities of daily living, and physical activity. After surgery, all patients were instructed to perform moderate-to-intense physical activity. All 78 patients were reassessed 6 months after bariatric surgery, and 52 patients were reassessed 3 years after bariatric surgery.
Results
Adherence to physical activity during the postoperative period was 36% at 6 months and 38% at 3 years. Compared with the patients who did not adhere to physical activity, weight loss was higher in the adherent patients at 6 months (29 ± 4% vs. 26 ± 5%; p = 0.01) and 3 years (32 ± 8% vs. 26 ± 6%, p = 0.005). The level of activities of daily living and quality of life also improved in the patients that adhered to physical activity at both 6 months and 3 years after bariatric surgery. However, no difference in dyspnea was observed between the adherent and non-adherent patients. Adherence to physical activity was an independent factor for postoperative weight loss.
Conclusion
Moderate-to-intense physical activity after bariatric surgery increases weight loss, quality of life, and level of activities of daily living, but does not directly influence dyspnea in individuals with morbid obesity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity affects more than 500 million adults and causes 35.8 million disability-adjusted life years worldwide [1]. Obesity is classified according to body mass index (BMI) as grade I, II, and III/morbid with concomitant risks of comorbidities, respectively [2]. In addition, obesity is associated with musculoskeletal [3,4,5] and respiratory disorders [6,7,8,9], which cause serious decreases in functional capacity [10] and quality of life [11].
The treatment for obesity consists primarily of an improvement in eating habits and increased physical activity [12, 13]. However, if the conservative treatments for obesity, including nutritional support, and pharmacologic and endoscopic procedures, are unsuccessful, the next option is surgery [14]. Bariatric surgery is the most effective treatment to control comorbidities [15, 16] and is indicated in individuals with grade III/morbid obesity or grade II obesity associated with a comorbidity [14]. Bariatric surgery aims to reduce weight [16], control comorbidities, and improve quality of life [17,18,19]. However, bariatric surgery per se is not a replacement for improved eating habits and regular participation in physical activities [20, 21].
An increase in physical activity after surgery optimizes weight reduction [22] compared with sedentary behavior. In addition, moderate-to-high-intensity activities are associated with successful obesity treatment by bariatric surgery [23], while sedentary behavior is a strong predictor for insufficient postoperative weight loss [24]. Physical activity reported in previous studies was assessed by a general questionnaire [22], accelerometry 2 to 5 years after surgery [23], or medical records [24]. No studies have focused on more intense activities, such as sports, after bariatric surgery for weight reduction and its association with dyspnea, quality of life, and level of activities of daily living. Therefore, the aim of this study was to evaluate the association of moderate-to-intense physical activity with the effects of bariatric surgery on weight loss, level of activities of daily living, dyspnea, and quality of life in sedentary individuals with morbid obesity.
Methods
Participants
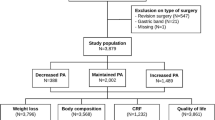
Individuals who did not practice regular physical activity, which was defined as 2 times a week for at least 3 months [25], were followed up at a clinic specializing in the treatment of obesity in Paraná, Brazil. We obtained informed consent from all individuals who agreed to participate in this study. The inclusion criteria were grade III/morbid obesity or grade II obesity associated with a comorbidity [26], preserved cognition, and a capacity to understand questionnaires. The exclusion criteria were the presence of other diseases or physical changes that interfered with the evaluations, canceled surgery, and need for another surgery during the 6-month follow-up period. This study was approved by the Universidade Cidade de São Paulo Ethics Committee (44734015.5.0000.0064).
Experimental Design
Consecutive individuals who had an indication for bariatric surgery were selected according to the eligibility criteria. Anthropometric data, physical activity, level of activities of daily living, dyspnea, and quality of life were assessed by questionnaires. Perioperative data were also collected. All selected individuals underwent bariatric surgery. At 1 month after surgery, all patients were instructed to perform moderate-to-intense physical activity on a regular basis. Patients were reassessed at 6 months and 3 years after surgery. Patients were considered to have adhered to physical activities if they increased their level of postoperative activity compared to their preoperative period; patients were considered non-adherent if they maintained or decreased their level of postoperative activity. Postoperative weight loss relative to the preoperative period (in percentage), level of activities of daily living, dyspnea, quality of life, and weight regain (weight gain after surgery, in relation to the preoperative period) outcomes were compared between the adherent and non-adherent groups.
Assessments
Weight and height were measured according to the National Institute of Health, Heart, Lung, and Blood recommendations [27]. Regular physical activity was measured by the Tegner activity scale, which assesses the level of sports activities [28, 29]; a zero score represents withdrawal from activity due to physical incapacity, a score of 1 to 7 represents sports and/or work activities, and a score of 8 to 10 represents competitive sports activities. The score on the Tegner activity scale is relative to the activities reported, regardless of the weekly frequency or practice time. We considered an individual adherent if they increased their score on the Tegner scale 6 months or 3 years after surgery. We considered an individual non-adherent if they maintained or decreased their score on the Tegner scale 6 months or 3 years after surgery.
The level of activities of daily living was measured by the Human Activity Profile (HAP) [30, 31]. The HAP questionnaire considers current and previous performance of activities of daily living [30]. The HAP questionnaire has 94 items that assess the performance of physical activities arranged by increasing difficulty. Each item has 3 answer options: I still do, I stopped doing, or I never did. The score was given by the Adjusted Activity Score. The number of items answered as “I stopped doing” is subtracted from the highest item answered as “I still do.”
Dyspnea symptoms were measured by the Modified Dyspnea Index (MDI) [32, 33]. The MDI questionnaire assesses an individual’s sensation of shortness of breath in three aspects: work and domestic activities, range of task, and range of effort. The final score ranges from 0 to 12 points; zero means disabling dyspnea and 12 means absence of dyspnea.
Quality of life was measured by the Moorehead–Ardelt Quality of Life Questionnaire II [34, 35] that has six domains: self-esteem, physical activity, social life, working conditions, sexual activity, and eating behavior.
Perioperative Aspects
Patients underwent vertical gastrectomy or gastroplasty with Roux-en-Y gastrointestinal bypass via video laparoscopy. The hospitalization period for all patients was 2 days, and there were no clinical or surgical complications. At 1 month after surgery, all patients were instructed to practice regular moderate-to-intense physical activity for a minimum of 30 min per day/2 times per week. Walking, gymnastics, biking, jogging, running, swimming, hydro-gymnastics, soccer play, bodybuilding, and CrossFit were presented as options. Patients were advised to choose an activity that they felt was pleasant and easily accessible.
Statistical Analysis
Sample calculation was performed for correlation (r = 0.44; p = 0.02) between weight loss and physical activity, with power of 80%, alpha of 5%, and expected sample loss of 15% [23]. Seventy-eight patients were required to respond to the primary aim of the study.
After normality by the Shapiro–Wilk test, the groups were compared using the t or Mann–Whitney, and chi-square tests. A multiple stepwise forward linear regression model was also used. The significance level was 5%. SigmaStat 12.1 software (San Jose, USA) was used.
Results
One hundred consecutive individuals with morbid obesity were selected for this study. Three individuals declined to participate. As a result, 97 individuals were included, but 8 did not respond to any of the postoperative questionnaires, and 11 underwent cholecystectomy during the follow-up period and were, therefore, excluded from the analyses. Seventy-eight patients were evaluated before surgery and 6 months after bariatric surgery, with 52 of these patients reevaluated 3 years after surgery (16 patients were lost to follow-up 3 years after surgery).
The age of the patients ranged from 19 to 62 years, and their BMI ranged from 34.9 to 55.2 kg/m2. Fifty-four patients (69.2%) reported having at least one obesity-associated comorbidity. The most common comorbidities reported were hypertension (55.1%), diabetes mellitus type II (21.7%), dyslipidemia (15.3%), and sleep apnea (11.5%). In addition, 14.1% of patients reported having a musculoskeletal pain condition (Table 1).
The patients’ postoperative weight loss in relation to their preoperative weight was 27 ± 5% through the 6th postoperative month and 29 ± 7% after 3 years. In addition, 38% of patients had weight regain (4 ± 3%) 3 years after surgery relative to their preoperative period. Physical activity, level of activities of daily living, quality of life increased, and dyspnea decreased after surgery (Table 2).
Six months after surgery, 36% of patients (28 patients) adhered to regular moderate-to-intense physical activity; the majority (54%) of these patients reported that they performed both aerobic activity and exercises for muscle strengthening 2–3 times per week. Compared to the patients who were non-adherent to postoperative moderate-to-intense physical activity, the adherent patients had greater weight loss (29 ± 4% vs. 26 ± 5%; p = 0.01), increased level of activities of daily living (16 ± 13 pts vs. 9 ± 13 pts; p = 0.03), and increased quality of life (1.36 ± 1.02 vs. 0.91 ± 0.89; p = 0.04).
Three years after surgery, 38% of patients adhered to regular moderate-to-intense physical activity. Compared to the patients who were non-adherent to moderate-to-intense physical activity, the adherent patients had greater weight loss (32 ± 8% vs. 26 ± 6%; p = 0.005), increased level of activities of daily living (23 ± 12 pts vs. 9 ± 2 pts; p < 0.0001), and increased quality of life (1.13 ± 1.0 vs. 0.51 ± 0.99; p = 0.03). We observed no differences in dyspnea for any of the reassessment periods (Table 3).
A comparison of patient activities at 6 months and 3 years after bariatric surgery showed an increase over time in bathing without help (4 vs. 16; p = 0.04), dancing (8 vs. 17; p = 0.04), shoveling (3 vs. 8; p = 0.04), and climbing 50 steps without stopping (27 vs. 40; p = 0.01).
The multiple linear regression model showed that both adherence to regular moderate-to-intense physical activity and age were independent factors associated with weight loss 6 months after surgery. The level of activities of daily living and type of surgery were not associated with weight loss. However, at 3 years after surgery, only adherence to regular moderate-to-intense physical activity was an independent factor associated with weight loss (Table 4).
After the follow-up period, weight loss was associated with an adherence to regular physical activity (odds ratio 1.12, 95% confidence interval 1.02–1.24), and weight regain was not associated with adherence to regular physical activity.
Discussion
This study demonstrates that bariatric surgery and its consequential weight loss improve an individual’s level of activities of daily living, dyspnea, and quality of life; in addition, moderate-to-intense regular physical activity intensifies these benefits. Adherence to regular moderate-to-intense physical activity during the postoperative period is an independent factor that positively influences an individual’s ability to reach the goals of bariatric surgery. Our results are consistent with previous studies that reported an intensified weight loss through physical activity [22, 23, 36]. However, these previous studies evaluated physical activity in a generalized way [22, 23, 36]. Our study detected this association by the use of an evaluation instrument that was focused on moderate-to-intense activities. We also observed an association of age with percentage of weight loss, probably due to the more prevalent concern with health in older adults compared to younger adults. Most individuals in our study were between the ages of 30 and 50 years and had comorbidities, and the stimulus for weight loss and improved health may have been higher in this age group than in younger adults.
Although weight loss induced by the increased energy expenditure of physical activity is lower than that induced by a decreased caloric intake [37,38,39,40], our study reinforces the hypothesis that an adherence to physical activity associated with dietary restriction methods, such as bariatric surgery, will optimize percentage reduction of body weight and provide health benefits. However, the postoperative weight regain we observed in some patients was not associated with physical activity, and this result was contrary to some previous studies. Amundsen et al. showed a lower level of physical activity in subjects with suboptimal weight loss (weight loss < 50%) or significant postoperative weight regain (total gain of weight > 15% compared to preoperative) 6 months to 2 years after surgery [41]. Another study showed an association of moderate-to-vigorous physical activity with better reduction and maintenance of weight 2 to 16 years after surgery [42]. However, there is still no consensus on the types of physical activity that are most effective in preventing postoperative weight regain.
As expected, observed weight loss was significant in the first 6 months after bariatric surgery and was retained for up to 3 years after surgery. The success of the obesity treatment was evidenced by improvements in the quality of life and increases in the level of activities of daily living evaluated by the HAP. The HAP includes activities that range from basic personal care to those with a significant expenditure of energy [31]. Thus, an increase in the HAP score indicates a change in lifestyle to more substantial activities of daily living and more intense physical activities, which were previously limited by morbid obesity. Previous studies have shown that an increase in postoperative sedentary activities, such as maintaining a seated position, is associated with a higher risk of comorbidities and mortality [43,44,45]. Therefore, the observed behavioral changes in our patients may have improved or reversed the effects of postoperative sedentary behavior on their general health status and quality of life. In addition, our patients carried out some activities that were preoperatively abandoned due to an incapacity or were never performed, and this should have positively affected their quality of life.
Our patients’ behavioral changes had no impact on dyspnea, which decreased independently from adherence to postoperative physical activity; weight loss was the predominant factor that impacted dyspnea. These findings reinforce the results of previous studies that reported surgery for obesity was effective at improving respiratory function due to decreased body fat, reducing dyspnea [46,47,48], and increasing the ability to perform activities of daily living [49].
Quality of life is multifactorial and involves many aspects, such as physical and mental function, that generally improve in obese individuals after surgery [50,51,52,53]. A previous study showed that quality of life increased significantly after an intervention program with counseling, increasing increase the level of physical activity prior to surgery, even when assessed by the non-specific The Medical Outcomes Study Short Form-36 health survey (SF-36) [54]; in addition, this previous study showed that an increase in moderate-to-intense physical activity during the preoperative period evaluated by an accelerometer was independently associated with improvements in physical function, body pain, general health status, and physical component in the SF-36. Our study complements these results by showing that the positive effect of physical activity on quality of life continues even with behavioral changes after surgery. These positive effects observed in our study were evidenced in both short and longer follow-up periods. In addition, our study used a specific instrument for this population that combined the aspects of other more general questionnaires [22, 54, 55] with eating behavior, which is the main focus of bariatric surgery.
A previous randomized clinical trial evaluated the effects of a 12-week moderate-intensity aerobic training program on the quality of life of obese subjects undergoing bariatric surgery [55]. Participants in the training program had better quality of life outcomes compared to the control group. Our study emphasizes the association of quality of life with the practice of sports, which reinforces the results of this previous clinical trial.
The main limitation of this study is that we lost some patients to follow-up 3 years after surgery. However, we believe that the reassessment of 67% of patients is sufficient to reflect the results between 6 months and 3 years of bariatric surgery, which were maintained over time. Other limitation is the information about adherence to physical activity had been measured by self-reporting which can bias the results. In addition, the Tegner activity scale could be adapted for the surgical population to include the frequency and time of performance of each activity included for scoring.
Our results show that postoperative moderate-to-intense physical activity is associated with postoperative weight loss and increases in the level of activities of daily living and quality of life, without a decrease in dyspnea greater than that caused by postoperative weight loss. Individuals with morbid obesity who are candidates for bariatric surgery should be advised to optimize their treatment outcomes with adherence to regular moderate-to-intense physical activity during the postoperative period.
References
World Health Organization. The Organization; c 2016 [cited 2016 Dec 1]. Global Health Observatory data; [about 4 screens]. Available from: http://www.who.int/gho/ncd/risk_factors/obesity_text/en/. Accessed 16 Sept 2018.
Nguyen NT, Magno CP, Lane KT, et al. Association of hypertension, diabetes, dyslipidemia, and metabolic syndrome with obesity: findings from the National Health and Nutrition Examination Survey, 1999 to 2004. J Am Coll Surg. 2008;207(6):928–34.
Seaman DR. Body mass index and musculoskeletal pain: is there a connection? Chiropr Man Therap. 2013;21(15):1–9.
DeMarco MA, Maynard JW, Huizinga MM, et al. Obesity and younger age at gout onset in a community-based cohort. Arthritis Care Res (Hoboken). 2011;63(8):1108–14.
Spector TD, Hart DJ, Doyle DV. Incidence and progression of osteoarthritis in women with unilateral knee disease in the general population: the effect of obesity. Ann Rheum Dis. 1994;53:565–8.
Olson AL, Zwillich C. The obesity hypoventilation syndrome. Am J Med. 2005;118(9):948–56.
Davies RJO, Stradling JR. The relationship between neck circumference, radiographic pharyngeal anatomy, and the obstructive sleep apneoa syndrome. Eur Respir J. 1990;3:509–14.
Manuel AR, Hart N, Stradling JR. Correlates of obesity-related chronic ventilatory failure. BMJ Open Respir Res. 2016;3(1):e000110.
Gibson GJ. Obesity, respiratory function and breathlessness. Thorax. 2000;55(1):S41–4.
Pataky Z, Armand S, Muller-Pinget S, et al. Effects of obesity on functional capacity. Obesity (Silver Spring). 2014;22(1):56–62.
Hassan MK, Joshi AV, Madhavan SS, et al. Obesity and health-related quality of life: a cross-sectional analysis of the US population. Int J Obes. 2003;27(10):1227–32.
Jacob JJ, Isaac R. Behavioral therapy for management of obesity. Indian J Endocrinol Metab. 2012;16(1):28–32.
Klem ML, Wing RR, McGuire MT, et al. A descriptive study of individuals successful at long-term maintenance of substantial weight loss. Am J Clin Nutr. 1997;66(2):239–46.
National Institutes of Health. Gastrointestinal surgery for severe obesity: NIH Consensus Development Conference Statement. Am J Clinl Nutr. 1992;55:S615–9.
Gloy VL, Briel M, Bhatt DL, et al. Bariatric surgery versus non-surgical treatment for obesity: a systematic review and meta-analysis of randomised controlled trials. BMJl. 2013;347:f5934.
Kissler HJ, Settmacher U. Bariatric surgery to treat obesity. Semin Nephrol. 2013;33(1):75–89.
Julia C, Ciangura C, Capuron L, et al. Quality of life after Roux-en-Y gastric bypass and changes in body mass index and obesity-related comorbidities. Diabetes Metab. 2013;39(2):148–54.
Peterli R, Borbely Y, Kern B, et al. Early results of the Swiss Multicentre Bypass or Sleeve Study (SM-BOSS): a prospective randomized trial comparing laparoscopic sleeve gastrectomy and Roux-en-Y gastric bypass. Ann Surg. 2013;258(5):690–4.
Reynolds CL, Byrne SM, Hamdorf JM. Treatment success: investigating clinically significant change in quality of life following bariatric surgery. Obes Surg. 2017;27(7):1842–8.
Freire RH, Borges MC, Alvarez-Leite JI, et al. Food quality, physical activity, and nutritional follow-up as determinant of weight regain after Roux-en-Y gastric bypass. Nutrition. 2012;28(1):53–8.
McMahon MM, Sarr MG, Clark MM, et al. Clinical management after bariatric surgery: value of a multidisciplinary approach. Mayo Clin Proc. 2006;81(10 Suppl):S34–45.
Bond DS, Phelan S, Wolfe LG, et al. Becoming physically active after bariatric surgery is associated with improved weight loss and health-related quality of life. Obesity (Silver Spring). 2009;17(1):78–83.
Josbeno DA, Kalarchian M, Sparto PJ, et al. Physical activity and physical function in individuals post-bariatric surgery. Obes Surg. 2011;21(8):1243–9.
Hatoum IJ, Stein HK, Merrifield BF, et al. Capacity for physical activity predicts weight loss after Roux-en-Y gastric bypass. Obesity (Silver Spring). 2009;17(1):92–9.
World Health Organization. Global recommendations on physical activity for health. Geneva: World Health Organization; 2010.
Farrell TM, Haggerty SP, Overby DW, et al. Clinical application of laparoscopic bariatric surgery: an evidence-based review. Surgl Endosc. 2009;23(5):930–49.
National Institutes of Healt. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults -The Evidence Report. Obes Res. 1998;6(Suppl 2):S51–209.
Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–9.
Briggs KK, Lysholm J, Tegner Y, et al. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med. 2009;37(5):890–7.
Fix AJ, Daughton D. Human activity profile: professional manual. Psychological Assessment Resources: Nebraska; 1988.
Souza DC, Wegner F, Costa LCM, et al. Measurement properties of the Human Activity Profile questionnaire in hospitalized patients. Braz J Phys Ther. 2017;21(3):153–8.
Stoller JK, Ferranti R, Feinstein AR. Further specification and evaluation of a new clinical index for dyspnea. Am Rev Respir Dis. 1986;134(6):1129–34.
Miura CTP, Gallani M, Domingues GBL, et al. Adaptação cultural e análise da confiabilidade do instrumento Modified Dyspnea Índex para a cultura brasileira. Rev Latino-Am Enfermagem. 2010;18(5):1–11. Brazilian
Moorehead MK, Ardelt-Gattinger E, Lechner H, et al. The validation of the Moorehead-Ardelt quality of life questionnaire II. Obes Surg. 2003;13(5):684–92.
Maciel J, Infante P, Ribeiro S, et al. Translation, adaptation and validation of a Portuguese version of the Moorehead-Ardelt Quality of Life Questionnaire II. Obes Surg. 2014;24(11):1940–6.
Livhits M, Mercado C, Yermilov I, et al. Exercise following bariatric surgery: systematic review. Obes Surg. 2010;20(5):657–65.
Foster-Schubert KE, Alfano CM, Duggan CR, et al. Effect of diet and exercise, alone or combined, on weight and body composition in overweight-to-obese post-menopausal women. Obesity (Silver Spring). 2012;20(8):1628–38.
Garrow JS, Summerbell CD. Meta-analysis: effect of exercise, with or without dieting, on the body composition of overweight subjects. Eur J Clin Nutr. 1995;49(1):1–10.
Batsis JA, Gill LE, Masutani RK, et al. Weight loss interventions in older adults with obesity: a systematic review of randomized controlled trials since 2005. J Am Geriatr Soc. 2017;65(2):257–68.
Johns DJ, Hartmann-Boyce J, Jebb SA, et al. Behavioural Weight Management Review G. Diet or exercise interventions vs combined behavioral weight management programs: a systematic review and meta-analysis of direct comparisons. J Acad Nutr Diet. 2014;114(10):1557–68.
Amundsen T, Strømmen M, Martins C. Suboptimal weight loss and weight regain after gastric bypass surgery—postoperative status of energy intake, eating behavior, physical activity, and psychometrics. Obes Surg. 2017;27(5):1316–23.
Herman KM, Carver TE, Christou NV, et al. Keeping the weight off: physical activity, sitting time, and weight loss maintenance in bariatric surgery patients 2 to 16 years postsurgery. Obes Surg. 2014;24(7):1064–72.
Katzmarzyk PT, Lee M. Sedentary behaviour and life expectancy in the USA: a cause-deleted life table analysis. BMJ Open. 2012;2(4):e000828.
Ford ES, Caspersen CJ. Sedentary behaviour and cardiovascular disease: a review of prospective studies. Int J Epidemiol. 2012;41(5):1338–53.
Edwardson CL, Gorely T, Davies MJ, et al. Association of sedentary behaviour with metabolic syndrome: a meta-analysis. PLoS One. 2012;7(4):e34916.
El-Gamal H, Khayat A, Shikora S, et al. Relationship of dyspnea to respiratory drive and pulmonary function tests in obese patients before and after weight loss. Chest. 2005;128(6):3870–4.
Boissiere L, Perotin-Collard JM, Bertin E, et al. Improvement of dyspnea after bariatric surgery is associated with increased expiratory reserve volume: a prospective follow-up study of 45 patients. PLoS One. 2017;12(9):e0185058.
Refsum HE, Holter PH, Lovig T, et al. Pulmonary function and energy expenditure after marked weight loss in obese women: observations before and one year after gastric banding. Int J Obes. 1990;14(2):175–83.
Parameswaran K, Todd DC, Soth M. Altered respiratory physiology in obesity. Can Respir J. 2006;13(4):203–10.
Batsis JA, Lopez-Jimenez F, Collazo-Clavell ML, et al. Quality of life after bariatric surgery: a population-based cohort study. Am J Med. 2009;122(11):1055.e1–1055.e10.
Dixon JB, Dixon ME, O'Brien PE. Quality of life after lap-band placement: influence of time, weight loss, and comorbidities. Obes Res. 2001;9(11):713–21.
Dymek MP, Le Grange D, Neven K, et al. Quality of life after gastric bypass surgery: a cross-sectional study. Obes Res. 2002;10(11):1135–42.
Major P, Matlok M, Pedziwiatr M, et al. Quality of life after bariatric surgery. Obes Surg. 2015;25(9):1703–10.
Bond DS, Thomas JG, King WC, et al. Exercise improves quality of life in bariatric surgery candidates: results from the Bari-Active trial. Obesity (Silver Spring). 2015;23(3):536–42.
Shah M, Snell PG, Rao S, et al. High-volume exercise program in obese bariatric surgery patients: a randomized, controlled trial. Obesity (Silver Spring). 2011;19(9):1826–34.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
The study was approved by the Universidade Cidade de São Paulo Ethics Committee (44734015.5.0000.0064).
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fontana, A.D., Lopes, A.D. & Lunardi, A.C. Bariatric Surgery Associated with Practice of Moderate to Intense Physical Activity Related to Weight Loss, Activity Level in Daily Life, Dyspnea, and Quality of Life of Sedentary Individuals with Morbid Obesity: a Prospective Longitudinal Study. OBES SURG 29, 2442–2448 (2019). https://doi.org/10.1007/s11695-019-03859-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03859-8