Abstract
Introduction
One-anastomosis-mini-gastric bypass (OAGB-MGB) is the second most popular gastric bypass procedure with remarkable weight loss results and comorbidity resolution rates. However, some concerns remain regarding its postoperative complications, including protein-calorie malnutrition (PCM). We hereby report our experience with patients who returned with severe PCM after OAGB-MGB.
Methods
Patients with severe obesity presenting to our referral bariatric center underwent OAGB-MGB surgery using a 200-cm biliopancreatic limb (BPL) by a single surgical team at three university hospitals from March 2014 to February 2016.
Results
From 189 patients undergoing OAGB-MGB, seven patients (3.7%), all female, with a mean age of 46.4 ± 8.2 years and initial body mass index (BMI) of 44.2 ± 4.7 kg/m2, were readmitted for signs of PCM. Lower extremity edema, fatigue, excessive weight loss, hypoalbuminemia, anemia, and pancytopenia were the presenting symptoms and lab findings. Revisional surgery was performed at a mean 19 ± 9.7 months after OAGB-MGB after failure of supportive measures. The mean BMI at the time of revision was 22.5 ± 2.6 kg/m2 with an excess weight loss of 109.2 ± 22.1%. After revisional surgery, one patient developed profound liver failure and expired. Another patient developed severe steatohepatitis but ultimately recovered. In the remaining five, edema and fatigue completely resolved at 1 month and hypoalbuminemia and anemia normalized at 2 months.
Conclusion
A one-fits-all BPL length of 200 cm is increasingly being questioned as it may result in an inadequate absorptive area and PCM in a subset of patients with shorter total bowel lengths, potentially placing them in danger and depriving them of bariatric surgery benefits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mini-gastric bypass (MGB) as first described by Rutledge in 1997 [1] and its variant, one-anastomosis gastric bypass (OAGB) by Carbajo and García-Caballero in 2002 [2], have gained popularity as the second most common gastric bypass technique after Roux-en-Y, owing to shorter operative times, easier technique, and safe surgical profile [3]. Compared to other bariatric options, it has shown excellent weight loss results and resolution of obesity-related comorbidities [3]. Nevertheless, utilization of this method, although slowly increasing in the Middle East and the Asia Pacific regions, has remained limited in many parts of the world mainly due to some concerns of postoperative complications [4].
Protein-calorie malnutrition (PCM) after OAGB-MGB has specifically been a major concern. Although preoperative nutritional status and underlying health problems have been linked to nutritional deficiencies after gastric bypass surgery [5], biliopancreatic limb (BPL) length is suspected to play the major role in postoperative PCM [6,7,8]. This is because BPL length directly determines the alimentary limb length in this loop-configuration bypass procedure. While increasing BPL length may enhance weight loss [9], it decreases the length of functional small intestine, i.e., the alimentary limb/common intestinal channel, and may thus aggravate malabsorption and nutritional deficiencies.
In this prospective case series, we report seven patients who presented with PCM after laparoscopic OAGB-MGB using a BPL length of 200 cm, in line with the Preferred Reporting Of Case Series in Surgery (PROCESS) guidelines [10].
Methods
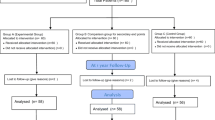
Tehran Obesity Treatment Study (TOTS) is a prospective study of patients with severe obesity referring to our specialized bariatric center to undergo surgery. Details of the study protocol are available elsewhere [11]. One hundred and eighty-nine patients, aged 18–65 years, with body mass index (BMI) ≥ 40 kg/m2 or between 35 and 40 kg/m2 in the presence of medical comorbidities, underwent laparoscopic OAGB-MGB. Surgery was performed by an experienced surgical team at three university hospitals from March 2014 to February 2016. Patients were followed until April 2018. All patients received oral multivitamin-minerals postoperatively: one Pharmaton® capsule daily (Boehringer Ingelheim Inc., Ingelheim am Rhein, Germany, containing 2 mg copper, 10 mg ferrous sulfate, 100 mg folic acid, 1 mcg vitamin B12, vitamins A, B group, C, D, and E, nicotinamide, and biotin) and one Calcicare tablet daily (200 IU vitamin D, 400 mg calcium, 100 mg magnesium, and 4 mg zinc). Patients were followed up postoperatively according to the protocol at 1, 3, 6, 9, 12, and 18 months and yearly thereafter. Anthropometric and biochemical data were routinely collected during each visit. Weight loss was calculated and reported as a change in BMI and percentage of excess weight loss (EWL%), with ideal weight defined as that corresponding to a BMI of 25 kg/m2.
During the follow-up period, nine patients overall (4.7%) were readmitted with serum albumin levels < 30 g/L in order to receive high-protein parenteral nutrition therapy, all of whom received intensive supportive therapy with more meticulous follow-up visits planned. Included in this report are seven patients who were readmitted for deteriorating PCM and severe hypoalbuminemia unresponsive to conservative therapy, necessitating revisional surgery.
Surgical Technique
A standard five-port laparoscopic technique with the operating table in reverse Trendelenburg position was used for OAGB-MGB. Briefly, a long gastric tube was created using Endo GIA stapler (Endo GIA Auto suture, Covidien, Mansfield, MA, USA) from the incisura angularis to the angle of His over a 36-F bougie. An antecolic loop gastrojejunostomy was performed 200 cm distal to the ligament of Trietz with an Endo GIA stapler and reinforced with continuous sutures. A methylene blue or air test was performed to check for leaks. At the completion of the procedure and at surgeon’s discretion, a white silicone drain (SUPA, Iran) was placed in the proximity of the GJ, which was then removed at the first postoperative visit barring any complications. Revisional procedures included five gastrogastrostomies and two reversals to normal gastrointestinal configuration.
Results
Patients’ baseline characteristics and follow-up changes are summarized in Table 1. All seven patients were female with a mean age of 46.4 ± 8.2 years. The mean preoperative BMI and body weight were 44.2 ± 4.7 kg/m2 and 115.1 ± 13.9 kg, respectively. At the initial presentation, two patients had a significant history for diabetes mellitus and were receiving anti-diabetic agents and two had a history of hypertension controlled by anti-hypertensive medications. Baseline complete blood count and liver function tests were normal in all patients; four cases had high triglycerides (TG), and two had elevated low-density lipoprotein (LDL) levels. None of the patients had protein and/or calorie malnutrition at the baseline evaluation. No significant Fe, Cu, Zn, Ca, P, ferritin, and vitamin D or B12 deficiency was identified at baseline. Preoperative liver ultrasound revealed fatty liver grade I in case #2, grade II in cases #1, #3, #4, and #6, and grade III in case #7. Mean operative time for OAGB-MGB was 110.8 ± 14.2 min [range 90–130]. There were no significant intraoperative events requiring conversions or blood transfusion.
At a mean period of 11.7 ± 4.5 months [range 8–18] after OAGB-MGB, six patients presented with generalized fatigue and lower extremity edema and one patient with excessive weight loss (Table 1). All patients had lost significant weight. Laboratory evaluation revealed hypoalbuminemia in all cases, anemia in three cases, and pancytopenia and high serum liver transaminases in one patient each. Patients were readmitted and received supportive measures including high-protein diet for 1–2 weeks and were discharged with acceptable general condition under close observation. During the follow-up, lower extremity edema persisted and albumin levels continued to decline. Serum liver enzymes rose in six of the seven patients. TG and LDL levels, however, had normalized in two (of four) and one (of two) patients, respectively. Fasting plasma glucose and HbA1c levels reached the normal range in both patients with DM. No significant micronutrient deficiency was identified.
All patients underwent revisional surgeries at a mean period of 19 ± 9.7 months [range 10–36] after OAGB-MGB. The mean BMI at the time of revision was 22.5 ± 2.6 kg/m2 with an excess weight loss of 109.2 ± 22.1%. Alimentary limb length was documented in 5 of the 7 patients. Patient #7 was found to have an alimentary limb of only 108 cm at autopsy (i.e., a total intestinal length of 308 cm), after she developed profound liver failure, severe hypoalbuminemia, and pancytopenia and expired a few days after revisional surgery [12]. Patient #6 developed progressive liver steatosis and anemia, but recovered with intensive supportive measures [13]. Her alimentary limb was approximately 350 cm at revision. Three of the remaining five patients had alimentary limbs of approximately 300 cm. All five regained weight after revision and lower extremity edema and generalized fatigue resolved by the first postoperative month; hypoalbuminemia and anemia normalized nearly 2 months after surgery (data not shown).
Discussion
OAGB-MGB has become a mainstream bariatric procedure that is gaining popularity in many centers especially in Europe, Asia Pacific, and the Middle East/North Africa region [14, 15]. As a relatively new procedure, however, it should carefully and critically be evaluated in order to improve its outcomes and address its associated potential complications. After establishing the efficacy of this procedure, the focus has now shifted towards the concerns regarding postoperative complications.
Short- and long-term results of this procedure have been published, showing a generally low early and late complication rate of 3% and 10%, respectively [16], compared to the two major bariatric procedures of sleeve gastrectomy and Roux-en-Y gastric bypass [7, 17]. However, in an interesting survey by Dr. Mahawar et al. [18] among surgeons not currently performing OAGB-MGB, increased risk of gastric and esophageal cancer, higher morbidity and mortality risk, and questionable efficacy were their top concerns; none of which, in the opinion of the authors, were supported by evidence. Nevertheless, bile reflux, marginal ulceration, pouch dilation, inadequate weight loss, and, in our case, excessive weight loss and severe nutritional deficiencies have been reported after this procedure [3]. Pending more evidence to better reveal the complete safety profile of this procedure, prompt diagnosis and timely management of complications are key to the patients’ safety.
In the experience of the authors, our patients have successfully lost weight and their comorbidities have improved during the first postoperative year. These favorable changes, however, occurred considerably faster than expected in a small subset of patients, discussed in this report. As comprehensively discussed by Dr. Nimeri [19], a major factor that determines the effect of bariatric surgery including its weight loss results and complication resolution, is the alimentary limb and common channel lengths, i.e., the absorptive area. With a procedure such as MGB with a loop configuration, BPL length directly determines the final alimentary limb length, which will also be the common channel. In this instance, it is the overall length of the small intestine, which could vary between 3 and more than 10 m [20, 21], that determines the final alimentary limb length. Without knowing the total length of small intestine, a fixed BPL of 200 cm, while probably safe in the majority of patients, could potentially lead to severe PCM [13] or even mortality in the case of short total bowel length [12].
A solution could be measuring the total bowel length in all patients, a practice that may lengthen the operative times and harbors the risk of bowel injury, or alternatively, choosing a more conservative BPL length, e.g., 150 cm [6], feared to risk suboptimal weight loss at least in a subset of super-obese patients [8]. In the former case, the experience has been very successful as described by Carbajo et al. in Spain [2], who recommend measuring the small bowel length and leaving at least 250–300 cm of common channel distal to the gastrojejunostomy. The latter case, however, as elaborated by Mahawar et al. [22], is not a simple linear relationship since gastric bypass, either in Roux-en-Y or OAGB-MGB configuration, is beyond just a restrictive and/or malabsorptive procedure. The fear of suboptimal weight loss with BPL of 150 cm may thus not be justified since neuro-hormonal and appetite changes are thought to play the major role in the long-term weight loss. These changes are observed after a combined BPL plus alimentary limb lengths of 150 cm after Roux-en-Y gastric bypass, which would translate into a BPL of 150 cm for OAGB-MGB, with not much added benefit with longer BPL lengths [9]. The relationship between BPL and alimentary limb lengths remains to be further investigated. In particular, the recent discussion around bypassing a “percentage” of intestine is promising and may lead to an answer to the “individual’s” optimal BPL length.
During the 2-year follow-up in our study, 9 of 189 patients (4.7%) returned with PCM after OAGB-MGB, and 7 (3.7%) required revisional surgery after failing to respond to intensive parenteral supplementation. Although this incidence was comparable to the revision rate of 2.69% reported by Lee et al. [23] (similarly, most commonly due to malnutrition), it was tenfold higher than the average rate of 0.37% reported by Mahawar et al. in a survey involving more than 47,000 cases [6]. In the opinion of the authors, and most importantly, a fixed BPL length of 200 cm, not considering the variability in total bowel lengths could account for this higher rate. In addition, there is a tendency by both surgeons and patients in our setting to favor revision because of insurance coverage issues associated with repeated hospitalizations for parenteral nutrition, lack of a structured patient support system, and accessibility issues, which could lead to late presentations and unfortunate consequences. Among these, the importance of sufficient psychosocial support, both at family and community levels, cannot be overemphasized. In an emerging setting like ours where social support structures are still in development, family support may serve as the only source of encouragement for the patients. Not surprisingly, all of our reported patients were facing family issues, which rendered them feeling helpless and vulnerable in their fight against obesity. Social media support and patient advocacy groups could partially offer such support.
Consequently, this experience has encouraged the authors to implement an individualized approach for patients choosing to undergo OAGB-MGB, which may include incorporating a shorter BPL length of 160 cm, measuring the total bowel length to make sure at least 350–400 cm of alimentary limb is present when a 200-cm BPL length is being considered (for patients with super-obesity), as well as administering a stricter clinical and laboratory follow-up for patients at risk. Moreover, more emphasis is put on the support these patients need with multiple visits and consultations with active inclusion of their families. Nevertheless, in the case of PCM and failed supportive measures, an earlier revisional surgery is discussed with our patients. Our upcoming comparison of two BPL lengths in OAGB-MGB patients with calculation of bypassed intestine percentage and future comparative trials may further clarify the optimal approach to minimize postoperative complications while maximizing metabolic benefits.
Conclusion
OAGB-MGB with a fixed BPL length of 200 cm for all patients may contribute to preventable and unnecessary cases of PCM requiring revisional surgery. Nevertheless, OAGB-MGB continues to prove as a safe and effective procedure and the decision on the BPL length is the one best tailored to individual patient’s characteristics to ensure maximum efficacy and safety. A consensus remains to be reached on such approach, which would render OAGB-MGB a more popular procedure among surgeons and patients likewise.
References
Rutledge R. The mini-gastric bypass: experience with the first 1,274 cases. Obes Surg. 2001;11(3):276–80. https://doi.org/10.1381/096089201321336584.
Carbajo MA, Luque-de-Leon E, Jimenez JM, et al. Laparoscopic one-anastomosis gastric bypass: technique, results, and long-term follow-up in 1200 patients. Obes Surg. 2017;27(5):1153–67. https://doi.org/10.1007/s11695-016-2428-1.
Georgiadou D, Sergentanis TN, Nixon A, et al. Efficacy and safety of laparoscopic mini-gastric bypass. A systematic review. Surg Obes Relat Dis. 2014;10(5):984–91. https://doi.org/10.1016/j.soard.2014.02.009.
Musella M, Susa A, Manno E, et al. Complications following the mini/one anastomosis gastric bypass (MGB/OAGB): a multi-institutional survey on 2678 patients with a mid-term (5 years) follow-up. Obes Surg. 2017;27(11):2956–67. https://doi.org/10.1007/s11695-017-2726-2.
Schlottmann F, Nayyar A, Herbella FAM, et al. Preoperative evaluation in bariatric surgery. J Laparoendosc Adv Surg Tech A. 2018;28(8):925–9. https://doi.org/10.1089/lap.2018.0391.
Mahawar KK, Parmar C, Carr WRJ, et al. Impact of biliopancreatic limb length on severe protein-calorie malnutrition requiring revisional surgery after one anastomosis (mini) gastric bypass. J Minim Access Surg. 2018;14(1):37–43. https://doi.org/10.4103/jmas.JMAS_198_16.
Jammu GS, Sharma R. A 7-year clinical audit of 1107 cases comparing sleeve gastrectomy, Roux-En-Y gastric bypass, and mini-gastric bypass, to determine an effective and safe bariatric and metabolic procedure. Obes Surg. 2016;26(5):926–32. https://doi.org/10.1007/s11695-015-1869-2.
Ahuja A, Tantia O, Goyal G, et al. MGB-OAGB: effect of biliopancreatic limb length on nutritional deficiency, weight loss, and comorbidity resolution. Obes Surg. 2018;28(11):3439–45. https://doi.org/10.1007/s11695-018-3405-7.
Mahawar KK, Kumar P, Parmar C, et al. Small bowel limb lengths and Roux-en-Y gastric bypass: a systematic review. Obes Surg. 2016;26(3):660–71. https://doi.org/10.1007/s11695-016-2050-2.
Agha RA, Borrelli MR, Farwana R, et al. The PROCESS 2018 statement: Updating Consensus Preferred Reporting Of CasE Series in Surgery (PROCESS) guidelines. Int J Surg. 2018;60:279–82. https://doi.org/10.1016/j.ijsu.2018.10.031.
Barzin M, Hosseinpanah F, Motamedi MA, et al. Bariatric surgery for morbid obesity: Tehran Obesity Treatment Study (TOTS) rationale and study design. JMIR Res Protoc. 2016;5(1):e8. https://doi.org/10.2196/resprot.5214.
Motamedi MAK, Barzin M, Ebrahimi M, et al. Severe fatal protein malnutrition and liver failure in a morbidly obese patient after mini-gastric bypass surgery: case report. Int J Surg Case Rep. 2017;33:71–4. https://doi.org/10.1016/j.ijscr.2017.02.033.
Motamedi MAK, Rakhshani N, Khalaj A, et al. Biopsy-proven progressive fatty liver disease nine months post mini-gastric bypass surgery: a case study. Int J Surg Case Rep. 2017;39:168–71. https://doi.org/10.1016/j.ijscr.2017.07.062.
Mahawar KK, Himpens J, Shikora SA, et al. The first consensus statement on one anastomosis/mini-gastric bypass (OAGB/MGB) using a modified Delphi approach. Obes Surg. 2018;28(2):303–12. https://doi.org/10.1007/s11695-017-3070-2.
Nimeri A, Al Hadad M, Khoursheed M, et al. The peri-operative bariatric surgery care in the Middle East Region. Obes Surg. 2017;27(6):1543–7. https://doi.org/10.1007/s11695-016-2503-7.
Bruzzi M, Rau C, Voron T, et al. Single anastomosis or mini-gastric bypass: long-term results and quality of life after a 5-year follow-up. Surg Obes Relat Dis. 2015;11(2):321–6. https://doi.org/10.1016/j.soard.2014.09.004.
Lee WJ, Ser KH, Lee YC, et al. Laparoscopic Roux-en-Y vs. mini-gastric bypass for the treatment of morbid obesity: a 10-year experience. Obes Surg. 2012;22(12):1827–34. https://doi.org/10.1007/s11695-012-0726-9.
Mahawar KK, Borg CM, Kular KS, et al. Understanding objections to one anastomosis (mini) gastric bypass: a survey of 417 surgeons not performing this procedure. Obes Surg. 2017;27(9):2222–8. https://doi.org/10.1007/s11695-017-2663-0.
Nimeri A. Making sense of gastric/intestinal bypass surgeries: forget the name and remember the degree of restriction and malabsorption the surgeries provide. Surg Obes Relat Dis. 2017;13(4):716–9. https://doi.org/10.1016/j.soard.2017.01.001.
Hess DS. Limb measurements in duodenal switch. Obes Surg. 2003;13(6):966. https://doi.org/10.1381/096089203322618885.
Tacchino RM. Bowel length: measurement, predictors, and impact on bariatric and metabolic surgery. Surg Obes Relat Dis. 2015;11(2):328–34. https://doi.org/10.1016/j.soard.2014.09.016.
Mahawar KK. Gastric bypass is not a “restrictive and Malabsorptive” procedure. Obes Surg. 2016;26(9):2225–6. https://doi.org/10.1007/s11695-016-2270-5.
Lee WJ, Lee YC, Ser KH, et al. Revisional surgery for laparoscopic mini-gastric bypass. Surg Obes Relat Dis. 2011;7(4):486–91. https://doi.org/10.1016/j.soard.2010.10.012.
Acknowledgments
The author would like to thank Dr. M. Hassan K. Motamedi for his language edit of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This study was approved by the institutional review board (no. IR.SBMU.ENDOCRINE.REC 1397.0592018-05-08). Informed consent was obtained from all individual participants included in the study. All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Khalaj, A., Kalantar Motamedi, M.A., Mousapour, P. et al. Protein-Calorie Malnutrition Requiring Revisional Surgery after One-Anastomosis-Mini-Gastric Bypass (OAGB-MGB): Case Series from the Tehran Obesity Treatment Study (TOTS). OBES SURG 29, 1714–1720 (2019). https://doi.org/10.1007/s11695-019-03741-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03741-7