Abstract
Introduction
Although several studies have compared totally robot-assisted gastric bypass (RA-GB) to laparoscopic gastric bypass (L-GB), the clinical benefit of the robotic approach remains unclear.
Materials and Methods
We compared perioperative outcomes of 82 consecutive patients undergoing RA-GB between 2013 and 2016 to 169 consecutive patients having undergone L-GB between 2009 and 2016. Secondary endpoints included duration of hospitalization, readmission rate, weight loss at 1 year, and the learning curve of RA-GB, assessed by operation times and complication rates.
Results
There were no statistically significant differences between groups concerning age (43.5 ± 11.2 vs. 42.2 ± 12.4 years), body mass index (42.4 ± 5.0 vs. 43.6 ± 7.2 kg/m2), or comorbidities. The rate of revision surgery was higher in L-GB group without reaching statistical significance. No statistically significant difference was observed for duration of operation (134 ± 35 vs. 135 ± 37 min), readmission rate at 90 days (4.9% vs. 8.9%), or percentage of excess weight loss at 1 year (RA-GB vs. L-GB) (76.8% ± 20.5 vs. 73.1% ± 23.5). There were fewer statistically significant complications overall in RA-GB (9.8% vs. 21.9%, p = 0.019). Median duration of hospital stay was shorter for RA-GB (3 vs. 4 days, p < 0.0001). The mean duration of operation for RA-GB decreased from 153 min in 2014 to 122 min in 2016; p = 0.004.
Conclusion
In our experience, the robotic approach for gastric bypass was associated with fewer postoperative complications compared to traditional laparoscopic gastric bypass. Cost increment associated with RA-GB remains an important drawback that hampers its widespread.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Morbid obesity is a major public health problem. According to the WHO, it affected 650 million people worldwide in 2016 [1]. Gastric bypass is the standard technique to obtain prolonged weight loss [2, 3]. First introduced by Masson in 1969 [4], and modified by Griffen in 1977 (Roux-en-Y reconstruction) [5], it is a combined restrictive and malabsorption procedure.
Laparoscopy is presently the preferred surgical approach [6], as it allows for reduced postoperative pain and improves postoperative recovery [7]. Laparoscopic gastric bypass surgery remains a difficult procedure, with poor work ergonomics for the surgeon [8]. Robotic may overcome some limitations of laparoscopic methods and improve outcomes. Currently, several publications have compared laparoscopic to robotic bariatric surgery with inconclusive results [9,10,11,12,13,14,15,16,17,18,19,20,21,22].
As we believed that short- and medium-term surgical results of robot-assisted laparoscopic gastric bypass (RA-GB) would be comparable to laparoscopic gastric bypass, this cohort study aimed to compare the postoperative course of patients who underwent RA-GB to a historical cohort of patients having undergone laparoscopic gastric bypass (L-GB).The secondary goal was to evaluate the learning curve of the robotic approach based on duration of intervention and complication rate during the study period.
Materials and Methods
After having received approval from the ethics committee of the Diaconesses Croix Saint-Simon hospital group (Paris, France), we analyzed the outcomes of all adult patients who underwent a gastric bypass between 2009 and 2016 in our institution. The inclusion criteria complied with the guidelines of the French Health Authority regarding surgical treatment of obesity [23]. All patients had a Body Mass Index (BMI) ≥ 40 kg/m2 or a BMI ≥ 35 kg/m2 in association with at least one of the following comorbidities: hypertension, diabetes, sleep apnea, osteoarticular disorders, and nonalcoholic steatohepatitis. Patient consent was obtained prior to performing the surgical intervention.
A multidisciplinary team comprising nutritionist, endocrinologist, psychologist, and surgeon had monitored the patients for at least 6 months prior to surgical treatment.
Patient Data
Among the 251 patients who underwent bypass surgery between 2009 and 2016, 169 underwent L-GB and starting in 2013, 82 patients underwent RA-GB. Demographic characteristics, and perioperative and postoperative variables were collected retrospectively for L-GB, but prospectively for RA-GB. The percentage of excess weight loss was calculated based on the guidelines published by Deitel and Greenstein [24].
The main assessment criterion for our study was the rate of postoperative complications at 30 days, as evaluated by the Dindo-Clavien classification [25]. All patients who had a complication grade 1 or higher were included in the complication rate. Complications were deemed severe when the grade was 3 or greater.
The secondary criteria were the duration of the hospitalization, the rate of readmission, the weight loss at 1 year, and the learning curve based on duration of operation and complication rates. The complication rate was calculated using the overall number of complications divided by the number of procedures for each year under scrutiny. We compared the duration of interventions in the first year to the last year of the RA-GB cohort at different steps of the operation (total duration, docking duration, duration of gastrojejunal anastomosis, jejunojejunal anastomosis). A non-exhaustive medical economic analysis was made to compare the two approaches.
Surgical Technique
The type of procedure (robotic or laparoscopic) depended on surgeon’s discretion. Briefly, after the acquisition of the robot by our institution, three surgeons (AV, NG, OO) started to perform all gastric bypass using the robotic platform, whereas two surgeons (see acknowledgment) did not take part in any robotic surgery. Robotic procedures were always performed by two senior surgeons, and a single surgeon (AV) was present in all robotic procedures. Supplementary file 1 shows the number of each procedure by year.
Laparoscopy gastric bypass was performed according to a standard technique [26] (Antecolic and antegastric Roux-en-Y limb of 150 cm). We performed the gastrojejunal and jejunojejunal anastomoses with an endo-GIA™ 60-mm stapler; the entry holes for the stapler were closed with a continuous suture of Vicryl® 2-0. All interventions were performed by experienced surgeons in laparoscopic and bariatric surgery.
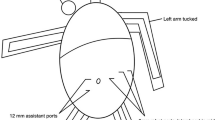
The robot-assisted gastric bypass was performed according to the technique described by Germain [27]. We used the da Vinci® system from Intuitive Surgical Inc. (Sunnyvale, USA) with four robotic arms. The gastric pouch was created by the assistant surgeon with an endo-GIA™ 60-mm stapler. An antecolic and antegastric Roux-en-Y limb of 150 cm was positioned in a counterclockwise set-up. The gastrojejunal and the jejunojejunal anastomoses were made with full-thickness Velock® 3-0 running sutures.
Anastomotic integrity was systematically tested with intra-luminal injection of methylene blue in both approaches.
The Postoperative Protocol
The postoperative protocol was the same for both cohorts. Patients were allowed to drink water in the evening of the intervention; pureed food was started on postoperative day 2.
Based on the clinical and biological criteria, the patients could generally be discharged on postoperative day 3. Upon discharge, a single daily dose of omeprazole, Tinzaparin sodium injection 4500 IU per day, compression stockings for 28 days, as well as vitamin supplementation were prescribed.
Statistical Analyses
Continuous variables were expressed as means with their standard deviation (SD) or medians with Interquartile Range (IQR), as appropriate. Normally distributed variables were analyzed using the Student t test while non-parametric variables were analyzed using the Wilcoxon test. Categorical variables were expressed as percentages. The association between categorical variables was analyzed using Pearson’s Chi-square test or Fisher’s exact test as appropriate. All variables with probability values < 0.05 were considered to be statistically significant. A logistic regression model was used to control for possible confounding factors. All statistical analyses were performed using R software (Free Software Foundation, University of Paris–Jussieu) by a medical biostatistician (KZ).
Results
Between 2009 and 2016, a total of 251 patients underwent a gastric bypass surgery. One hundred sixty-nine patients underwent L-GB and starting in 2013; the RA-GB cohort included 20 patients the first year (2013), 27 patients in the second year (2014), 15 in the third (2015), and 20 in the fourth (2016) (supplementary file 1).
Table 1 presents the comparison of demographic data. There were no significant differences between the two groups with regard to age, gender, initial weight, BMI, comorbidities (e.g., arterial hypertension (AHT), prior abdominal surgery, diabetes, cardiovascular disease, or rheumatologic complications), and the American Society of Anesthesiologists (ASA) score. There was a significant difference between the two groups in terms of the rate of sleep apnea (41.4% vs. 24.9%, p = 0.012) and the rate of smoking (7.3% vs. 19.5%, p = 0.007) favoring RA-GB versus L-GB.
All patients were assessed at 30 days. At 1 year, 88 patients were lost to follow-up (35%), 34 in the RA-GB group, and 54 in the L-GB group (41.5% vs. 32.0%, p = 0.177). Table 2 summarizes the postoperative course for the two groups. Postoperative complications were more frequently observed in the L-GB group (21.9% vs. 9.8%, p = 0.019). However, no significant difference was found between the groups regarding the rate of severe complications (6.1% vs. 13.0% for RA-GB and L-GB respectively; p = 0.149). It is worth noticing that the readmission rate at 90 days is almost double in the L-GB (RA-GB 4.9% vs. L-GB 8.9%; p = 0.385) even if it did not reach statistical significance.
Table 3 summarizes the postoperative complications. No differences were observed in the rate of anastomotic fistula (RA-GB 2.4% vs. L-GB 3.0%, p = 0.815), duration of operation, (134 ± 35 vs. 135 ± 37 min, p = 0.925), or blood loss (26 ml vs. 36 ml, p = 0.054). The rate of revision surgery was higher in L-GB group (26.6% vs. 15.9%) but it was not statistically significant. Moreover, revision surgery was not associated with a higher complication rate in this series (Supplementary file 2).
The median duration of hospital stay was 3 [3–4] days for the RA-GB group vs. 4 [3–5] days for the L-GB group, (p = 0.038).
Bariatric Results
The average percentage of excess weight loss at 1 year in the RA-GB group was 71.3% ± 20.5 vs. 73.7% ± 23.5, in the L-GB group (p = 0.360).
Learning Curve Analysis for the RA-GB Group
Table 4 presents the comparison of durations for the overall procedure and the main intraoperative steps for the first and the last year of the study. A significant decrease was seen for all of the surgical steps, except for the docking time. Operative duration decreased until the 22nd operation, showed a slightly increase between the 23rd and the 41st (from 133 to 141 min) to finally drop again after the 42nd (Fig. 1).
The first complication occurred in the 15th patient. The complication rate dropped after the52nd intervention (Fig. 2).
Discussion
Outcome comparison between RA-GB (from the first patient) and the historical L-GB cohort showed RA-GB to be associated with lower overall complication rate. Of notice, this difference was no longer observed for severe complication rate. Also RA-GB was associated with a shorter hospital stay, without increasing the operative time. Our results support the notion that RA-GB is at least as effective as L-GB. In spite of the fact that the rate of revision surgery was higher in L-GB group, it was not associated with a higher complication rate. These results are in accordance with the literature that showed all adverse events rate similar to or slightly higher than primary gastric bypass [28]. In the long term, there was no significant difference in the percentage of excess weight loss between the two groups, but the important loss of follow-up rate (35%) observed after 1 year forbids any definitive conclusion.
We were unable to find any randomized trials comparing RA-GB to L-GB. There are, however, numerous monocenter cohorts, a few meta-analyses, and a national cohort study from the USA. The rates of complications for these various studies varied from 11 to 26.2% for L-GB vs. 2.2 to 29% for RA-GB [10,11,12,13], which matches the complication rates found in our study.
The rate of anastomotic leak in our study was 3% which compares favorably to the 1%–5% rate usually found in the literature [29,29,31] Of notice, the technique used for anastomosis was not the same in the two groups, since we performed manual anastomoses for patients in RA-GB and mechanical anastomoses for patients in L-GB. Concerning this particular subject, the literature provides contradictive results with some reports showing fewer anastomotic leak with robotic approach [9, 12], while others reported the opposite [10, 13, 14]. The meta-analysis by Economopoulos et al., comparing laparoscopic to RA-GB, did not reveal any statistically significant difference in the rate of postoperative leaks (OR = 0.68 [0.32–1.45]), but found fewer anastomotic strictures after RA-GB [16].
Celio et al. [17] compared 2415 RA-GB with 135,040 L-GB over a 7-year period in the American BOLD (bariatric outcome longitudinal database) cohort. They observed a higher rate of complications and leaks and a longer operative time in the RA-GB group. However, because of the poor quality of data (administrative data base) and the fact that the period of analysis (2007 to 2012) corresponds with the beginning of the uptake of the robotic technique in bariatric surgery, its results do not rule off this question. Indeed, due to the lack of tactile feedback, special caution is warranted when handling the small intestines with the robot, and it is probably that a certain number of complications observed at the beginning of the robotic may be overcome later on the learning curve.
We did not find any difference in operative time between the two groups what is in opposition with most comparative studies and meta-analyses that have shown RA-GB to be longer than standard laparoscopic surgery [11, 12, 18, 21, 32,32,34]. We, as others, found an improvement in operative time [20, 21] along the learning curve.
Our analysis of the learning curve based on the duration of the procedure and the complication rate places the turning point for better results in RA-GB between 40 and 50 procedures, whereas 50–100 procedures have been reported to be necessary for L-GB [35].
We found that the percentage of excess weight loss at 1 year did not differ statistically between patients undergoing RA-GB or L-GB which is in accordance with the literature [12, 18, 19, 36, 37]. We observed a high percentage of loss to follow-up at 1 year, but this is similar to other studies [15].
We found fewer complications in the RA-GB group. However, our study has the classical drawbacks of non-randomized comparisons. Also, the single-center nature of this analysis and the low volume potentially limit its generalizability, but at opposite, this allow to avoid surgical variation and for that reason to evaluate only the surgical technique link to the device. Herein, postoperative care may have evolved and data in the L-GB group, which were retrospectively collected, may under-report complications and comorbidities. If, however, the lower rate of complications observed in RA-GB can be confirmed by other studies, this might be an advantage that should be taken into consideration when the two procedures are compared in the future.
Lastly, cost performance is an important issue regarding robotic surgery. In our institution, each robotic procedure has an additional cost of €3500. Theoretically, as with many other technologies, the price of robotic machines is bound to come down. Furthermore, although this remains to be proven, the additional expenses may someday be offset by the advantages of robot-assisted surgery (e.g., easier dissection of the gastric pouch and faster manual anastomoses).
Conclusion
Notwithstanding the lack of formal proof and the fact that surgeons are naturally enthusiastic persons, we do believe that the use of robots is a significant step forward for surgeons. Although clinical advantage of RA-GB over L-GB may not be unanimous, we can actually estate that RA-GB is a safe and effective procedure in experienced hands.
References
OMS | Obésité et surpoids [Internet]. Available from: http://www.who.int/mediacentre/factsheets/fs311/fr/
O’Brien PE, McPhail T, Chaston TB, et al. Systematic review of medium-term weight loss after bariatric operations. Obes Surg. 2006;16:1032–40.
Puzziferri N, Roshek TB, Mayo HG, et al. Long-term follow-up after bariatric surgery: a systematic review. JAMA. 2014;312:934–42.
Masson E. Évaluation du taux de réadmissions précoces comme indicateur de la qualité des soins à l’hôpital [Internet]. EM-Consulte. [cited 2016 Sep 20]. Available from: http://www.em-consulte.com/article/106659/figures/evaluation-du-taux-de-readmissions-precoces-comme-
Griffen WO, Young VL, Stevenson CC. A prospective comparison of gastric and jejunoileal bypass procedures for morbid obesity. Ann Surg. 1977;186:500–9.
Wittgrove AC, Clark GW, Tremblay LJ. Laparoscopic gastric bypass, Roux-en-Y: preliminary report of five cases. Obes Surg. 1994;4:353–7.
Wittgrove AC, Clark GW. Laparoscopic gastric bypass, Roux-en-Y-500 patients: technique and results, with 3-60 month follow-up. Obes Surg. 2000;10:233–9.
Alleblas CCJ, de Man AM, van den Haak L, et al. Prevalence of musculoskeletal disorders among surgeons performing minimally invasive surgery: a systematic review. Ann Surg. 2017;266:905–20.
Buchs NC, Morel P, Azagury DE, et al. Laparoscopic versus robotic Roux-en-Y gastric bypass: lessons and long-term follow-up learned from a large prospective monocentric study. Obes Surg. 2014;24:2031–9.
Benizri EI, Renaud M, Reibel N, et al. Perioperative outcomes after totally robotic gastric bypass: a prospective nonrandomized controlled study. Am J Surg. 2013;206:145–51.
Park CW, Lam ECF, Walsh TM, et al. Robotic-assisted Roux-en-Y gastric bypass performed in a community hospital setting: the future of bariatric surgery? Surg Endosc. 2011;25:3312–21.
Snyder BE, Wilson T, Leong BY, et al. Robotic-assisted Roux-en-Y gastric bypass: minimizing morbidity and mortality. Obes Surg. 2010;20:265–70.
Moon RC, Gutierrez JC, Royall NA, et al. Robotic Roux-en-Y gastric bypass, is it safer than laparoscopic bypass? Obes Surg. 2016;26:1016–20.
Smeenk RM, van ‘t Hof G, Elsten E, et al. The results of 100 robotic versus 100 laparoscopic gastric bypass procedures: a single high volume centre experience. Obes Surg. 2016;26:1266–73.
Economopoulos KP, Theocharidis V, McKenzie TJ, et al. Robotic vs. laparoscopic Roux-En-Y gastric bypass: a systematic review and meta-analysis. Obes Surg. 2015;25:2180–9.
Markar SR, Karthikesalingam AP, Venkat-Ramen V, et al. Robotic vs. laparoscopic Roux-en-Y gastric bypass in morbidly obese patients: systematic review and pooled analysis. Int J Med Robot Comput Assist Surg MRCAS. 2011;7:393–400.
Celio AC, Kasten KR, Schwoerer A, et al. Perioperative safety of laparoscopic versus robotic gastric bypass: a propensity matched analysis of early experience. Surg Obes Relat Dis Off J Am Soc Bariatr Surg. 2017;13:1847–52.
Stefanidis D, Bailey SB, Kuwada T, Simms C, Gersin K. Robotic gastric bypass may lead to fewer complications compared with laparoscopy. Surg Endosc 2017;32(2):610–16.
Ayloo SM, Addeo P, Buchs NC, et al. Robot-assisted versus laparoscopic Roux-en-Y gastric bypass: is there a difference in outcomes? World J Surg. 2011;35:637–42.
Sanchez BR, Mohr CJ, Morton JM, et al. Comparison of totally robotic laparoscopic Roux-en-Y gastric bypass and traditional laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis Off J Am Soc Bariatr Surg. 2005;1:549–54.
Scozzari G, Rebecchi F, Millo P, et al. Robot-assisted gastrojejunal anastomosis does not improve the results of the laparoscopic Roux-en-Y gastric bypass. Surg Endosc. 2011;25:597–603.
Rogula T, Koprivanac M, Janik MR, et al. Does robotic Roux-en-Y gastric bypass provide outcome advantages over standard laparoscopic approaches? Obes Surg. 2018;28:2589–96.
Haute Autorité de Santé - Obésité : prise en charge chirurgicale chez l’adulte [Internet]. [cited 2018 Jan 29]. Available from: https://www.has-sante.fr/portail/jcms/c_765529/fr/obesite-prise-en-charge-chirurgicale-chez-l-adulte
Deitel M, Greenstein RJ. Recommendations for reporting weight loss. Obes Surg. 2003;13:159–60.
Dindo D, Demartines N, Clavien P-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Lönroth H. Laparoscopic gastric bypass. Obes Surg. 1998;8:563–5.
Germain A, Reibel N, Brunaud L. Totally robotic gastric bypass. J Visc Surg. 2011;148:e267–72.
Brethauer SA, Kothari S, Sudan R, et al. Systematic review on reoperative bariatric surgery: American society for metabolic and bariatric surgery revision task force. Surg Obes Relat Dis Off J Am Soc Bariatr Surg. 2014;10:952–72.
Lee S, Carmody B, Wolfe L, et al. Effect of location and speed of diagnosis on anastomotic leak outcomes in 3828 gastric bypass cases. J Gastrointest Surg Off J Soc Surg Aliment Tract. 2007;11:708–13.
DeMaria EJ, Sugerman HJ, Kellum JM, et al. Results of 281 consecutive total laparoscopic Roux-en-Y gastric bypasses to treat morbid obesity. Ann Surg. 2002;235:640–5. 645-647
Chang S-H, Freeman NLB, Lee JA, et al. Early major complications after bariatric surgery in the USA, 2003–2014: a systematic review and meta-analysis. Obes Rev Off J Int Assoc Study Obes. 2018;19:529–37.
Hubens G, Balliu L, Ruppert M, et al. Roux-en-Y gastric bypass procedure performed with the da Vinci robot system: is it worth it? Surg Endosc. 2008;22:1690–6.
Artuso D, Wayne M, Grossi R. Use of robotics during laparoscopic gastric bypass for morbid obesity. JSLS. 2005;9:266–8.
Hagen ME, Pugin F, Chassot G, et al. Reducing cost of surgery by avoiding complications: the model of robotic Roux-en-Y gastric bypass. Obes Surg. 2012;22:52–61.
Zevin B, Aggarwal R, Grantcharov TP. Simulation-based training and learning curves in laparoscopic Roux-en-Y gastric bypass. Br J Surg. 2012;99:887–95.
Mohr CJ, Nadzam GS, Alami RS, et al. Totally robotic laparoscopic Roux-en-Y gastric bypass: results from 75 patients. Obes Surg. 2006;16:690–6.
Deng JY, Lourié DJ. 100 robotic-assisted laparoscopic gastric bypasses at a community hospital. Am Surg. 2008;74:1022–5.
Acknowledgements
We thanks Dr Remi Houdart and Dr José Hobeika who performed many of the L-GB cases included in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval Statement
For this type of study, formal consent is not required.
Informed Consent Statement
Does not apply.
Conflict of Interest
Disclosure Author 6, Author 3, and Author 4 are proctors for Intuitive Surgical and Covidien. Author 1 and Author 2 have no conflicts of interest or financial ties to disclose.
Electronic Supplementary Material
ESM 1
(DOCX 20 kb)
Rights and permissions
About this article
Cite this article
Cahais, J., Lupinacci, R.M., Oberlin, O. et al. Less Morbidity with Robot-Assisted Gastric Bypass Surgery than with Laparoscopic Surgery?. OBES SURG 29, 519–525 (2019). https://doi.org/10.1007/s11695-018-3545-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3545-9