Abstract
Background
Bariatric surgery is the most effective long-term treatment of severe obesity. Unfortunately, many patients experience inadequate weight loss, weight plateau, or weight recidivism. We sought to determine the efficacy of high-dose liraglutide (3.0 mg once daily) in patients with prior bariatric surgery.
Methods
We performed a retrospective chart review of 33 consecutive patients, aged 18–65, who received liraglutide for weight loss in the setting of any previous bariatric surgery. Indications were weight recidivism (> 10% weight regain from lowest post-surgical weight), inadequate weight loss (< 20% weight loss from initial clinic assessment, or pre-surgical weight if unavailable), and plateau (patient desires further weight loss but does not fit into either other category). Our primary outcomes were median percentage weight loss and median BMI change at 16 and 28 weeks, inclusive of time taken to titrate the medication to target dose. Secondary outcomes were the presence of adverse effects and the need to discontinue the medication.
Results
Of a total of 33 patients identified, 20 met inclusion criteria and had adequate data to be included in our analysis. At 16 weeks median percentage weight loss was 7.1% (IQR 5.1–12.2%), and at 28 weeks 9.7% (IQR 7.8–13.9%). Median BMI change was 3.5 kg/m2 (16 weeks, IQR 2.2–4.6 kg/m2) and 4.7 kg/m2 (28 weeks, IQR 3.7−5.6 kg/m2). There were no major adverse events.
Conclusions
High-dose liraglutide is an effective adjunct treatment for weight loss in patients with prior bariatric surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction/Purpose
Bariatric surgery is a safe and effective treatment to achieve significant long-term weight loss in patients with severe obesity [1]. However, a substantial number of patients experience inadequate weight loss, a weight-loss plateau, or weight recidivism [2]. Long term, as many as 10–20% of patients regain all of the weight lost through surgery [3]. The causes for this are numerous and varied. Although some negative outcomes are related to defined anatomic and surgical issues, including gastrogastric fistulas, adjustable gastric band slippage, and pouch or stoma dilatation [4], which can be addressed by revision surgery, in many cases poor outcomes are attributable to behavioral, medical, and psychosocial factors [5]. There is a significant economic and resource burden to bariatric revision surgery [6]. This has led to growing interest in the use of pharmacotherapy as an adjunct to bariatric surgery to achieve and sustain weight loss.
Liraglutide is a glucagon-like peptide-1 (GLP-1) analogue and has been approved for the medical treatment of obesity both in Canada and in the USA. High-dose liraglutide (3.0 mg) has been shown to significantly enhance and sustain weight loss in patients who have previously lost weight on a low-calorie diet [7]. This supports the notion that liraglutide may also be useful as a pharmacological adjunct to bariatric surgery in patients with inadequate weight loss or weight recidivism.
Here, we present a retrospective review of 20 patients with previous bariatric surgery who completed 28 weeks of high-dose liraglutide therapy for the purpose of weight loss.
Materials and Methods
We performed a retrospective chart review of consecutive patients at the Edmonton Adult Bariatric Specialty Clinic, who received liraglutide for weight loss following bariatric surgery to determine the efficacy of liraglutide in this setting. Indications were weight recidivism (> 10% weight regain from lowest post-surgical weight), inadequate weight loss (< 20% weight loss from initial clinic assessment, or pre-surgical weight if unavailable), and weight-loss plateau (patient desires further weight loss but does not fit either of the other categories). Included were patients 18–65 years of age, with previous bariatric surgery of any kind, a BMI ≥ 30 kg/m2, who were interested in adjunctive anti-obesity medication, and in whom informed consent was obtained. Exclusions included any patient with a personal or family history of medullary thyroid carcinoma (MTC) or multiple endocrine neoplasia type 2 (MEN2), any personal history of non-familial MTC, current use of GLP-1 receptor agonist or other approved weight loss medication, personal history of acute or chronic pancreatitis, significant active cardiovascular disease, intolerance or allergy to liraglutide, active pregnancy or breastfeeding or imminent plans to become pregnant, ongoing post-operative complications, and reversal of the primary bariatric surgical procedure (i.e., removal of adjustable gastric band). Patients with discontinuation of liraglutide prior to 28 weeks, loss to follow-up, revision surgery prior to 28 weeks (including removal of adjustable gastric band), or initiation of complete meal replacement prior to 28 weeks were not included in the final analysis.
All patients were evaluated for a surgical cause of suboptimal weight loss prior to administration of medication. Patients were also assessed by a registered dietician and counseled on strategies to achieve a daily 500 kcal deficit diet. Patients were educated about common side effects, cost and coverage issues, weight loss expectations, and the long-term nature of medical treatment strategies. Primary outcomes were median percentage weight loss and median BMI change at 16 and 28 weeks on liraglutide 3.0 mg subcutaneously (inclusive of time taken to titrate the medication to target dose). Given the retrospective nature of this study, data was collected for the closest available date. Secondary outcomes included the presence of adverse effects and need to discontinue medication.
Ethics approval was obtained from the local ethics review board.
Results
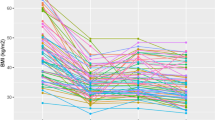
A total of 33 patients were identified who received any dose of liraglutide following bariatric surgery. Of these, 20 patients met inclusion criteria and had adequate data to be included in our analysis. Thirteen patients were excluded, as outlined in the consort diagram (Fig. 1). Baseline characteristics are reported in Table 1. Median weight loss was 7.1% at 16 weeks (IQR 5.1–12.2%) and 9.7% at 28 weeks (IQR 7.8–13.9%). Median BMI change was 3.5 kg/m2 at 16 weeks (IQR 2.2–4.6 kg/m2) and 4.7 kg/m2 at 28 weeks (IQR 3.7−5.6 kg/m2). Precisely one half of participants achieved a 28-week weight lower than their nadir post-surgical weight. Individual data is shown in Table 2. Changes in median body weight pre-surgery, at nadir, at initiation of liraglutide, and after 16 and 28 weeks are illustrated in Fig. 2. There were no major adverse events. Frequency of adverse effects is shown in Table 3.
Consort Diagram. Flow of patients through the study. Charts were reviewed for all post-surgical patients started on liraglutide between December 2015 and June 2017. Patients were included in the final analysis if they completed 28 weeks of liraglutide, and no confounding factor was present. Consort diagram of all post-surgical patients started on liraglutide between December 2015 and June 2017
Median weight at each point of interest. Box and whisker plot of median patient weight pre-surgery (126.25 kg), nadir (92.45 kg), prior to starting liraglutide (109.55 kg), after 16 weeks of liraglutide (99.4 kg), and after 28 weeks of liraglutide (95.9 kg). Bottom and top of box represent the first and third quartiles, respectively. The ends of the whiskers represent the minimum and maximum of the data
Three patients discontinued liraglutide prematurely. The first was a 40-year-old female with type 2 diabetes who had a Roux-en-Y gastric bypass (RYGB) done 20 months prior to initiation of therapy. She experienced significant nausea, diarrhea, gastroesophageal reflux, and loss of appetite to the point that she self-discontinued the medication after a few doses. The second was a 44-year-old non-diabetic female who developed a rash after 15 weeks on liraglutide. Liraglutide was held for 5 weeks and the rash resolved completely. She was then able to resume liraglutide at a lower dose without any further rash. It is not clear whether liraglutide was the cause of her rash. She did not have any other adverse effects on liraglutide. The third patient was a 60-year-old female who discontinued the medication due to cost.
We performed a subgroup analysis, comparing patients who achieved > 5% weight loss at 16 weeks to patients who did not. This is in keeping with the Canadian [8] and European Medical Agency [9] product monograph stopping rule criteria. Fifteen early responders and five early non-responders were identified. At 28 weeks, early responders achieved a median 12.2% weight loss (IQR 8.7–15.5%) and a median BMI change of 4.9 kg/m2 (IQR 4.1–5.7 kg/m2). Early non-responders achieved a median weight loss of only 6.4% (IQR 3.6–7.7%) and a median BMI change of 2.0 kg/m2 (IQR 1.6−4.1 kg/m2).
A further subgroup analysis was performed looking only at patients with type 2 diabetes (n = 5). At 16 weeks, patients with type 2 diabetes achieved a median weight loss of 5.7% (IQR 4.9–8.5%) and median BMI reduction of 3.5 kg/m2 (IQR 2.6–3.8 kg/m2). At 28 weeks, patients with type 2 diabetes maintained a median weight loss of 8.4% (IQR 7.7–9.1%), corresponding to a BMI change of 4.1 kg/m2 (IQR 3.7–4.6 kg/m2).
Stratified by indication for liraglutide, all three groups had similar results at 28 weeks. Patients with recidivism (n = 10) lost a median 12.9% body weight (IQR 8.7–16.1%), corresponding to a median BMI change of 5.6 kg/m2 (IQR 4.5−5.7 kg/m2). Patients with weight plateau (n = 3) lost a median 8.9% body weight (IQR 7.6–8.9%), corresponding to a median BMI change of 3.7 kg/m2 (IQR 2.9–4.3 kg/m2). Patients with inadequate weight loss (n = 7) lost a median 8.4% body weight (IQR 7.3–12.3%), corresponding to a BMI change of 4.1 kg/m2 (IQR 3.1–5.3 kg/m2).
Discussion
Our findings of substantial clinically meaningful sustained weight loss on liraglutide in patients who had previously undergone bariatric surgery support the notion that liraglutide holds promise as an adjunctive weight loss medication for patients who have achieved unsatisfactory outcomes with bariatric surgery.
Our findings are consistent with previous retrospective analyses on the use of anti-obesity medications in patients with previous bariatric surgery. Thus, Pajecki et al. [10] reported on 15 patients with prior bariatric surgery, and either excess weight loss less than 50% after 2 years of follow-up or more than 15% weight regain from nadir, who received liraglutide at doses from 1.2 to 3.0 mg daily for eight to 28 weeks follow-up. Significant weight loss was achieved compared with baseline (100.9 ± 18.3 kg. vs 93.5 ± 17.4 kg, p < 0.0001). The most common side effect was nausea, and four patients discontinued therapy due to either cost or inadequate weight loss. Similarly, Creange et al. [11] reported significant weight loss achieved at 16 (3.3 kg lost) and 24 weeks (10.2 kg lost) in a retrospective review of 25 patients with prior bariatric surgery, who received between 1.2 and 3.0 mg of liraglutide for weight loss. Another retrospective study reported weight loss (3.4 kg from baseline) in 15 bariatric surgery patients with type 2 diabetes, who were treated with liraglutide for a minimum of 2 years for glycemic control [12]. Finally, a retrospective review of 319 patients from two sites who had prior bariatric surgery and had been placed on any obesity medication (only 12% of patients were on liraglutide) for subsequent weight loss showed a mean-added benefit of 7.6% weight loss (8.1 kg) [13]. Together with our observations on high-dose liraglutide, these studies support the idea that pharmacological adjuncts can have substantial efficacy in the post-surgical population.
Our analysis of early responders and early non-responders supports the use of 5% as a cutoff at 16 weeks to predict clinically significant weight loss at 28 weeks. This cutoff has been used in the non-surgical population to differentiate “early responders” from “early non-responders” and has been shown to predict superior weight loss as well as improvements in glycemic parameters at 160 weeks [14]. Our findings show that the same “stopping rule” enables clinicians to identify post-surgery patients who are unlikely to benefit from prolonged use of the medication.
Our analysis of patients with type 2 diabetes suggests that clinically meaningful weight loss can be achieved in patients with prior bariatric surgery, compared to baseline. Liraglutide (3.0 mg) has been shown to be effective as a weight loss medication in patients with type 2 diabetes without a prior history of bariatric surgery [15]. Our findings support the notion that a history of prior bariatric surgery should not necessarily preclude the use of this medication for the purpose of weight loss in patients with diabetes.
Patients with a history of recidivism or inadequate weight loss following surgery clearly had statistically and clinically significant weight loss at 28 weeks, compared with baseline. While patients who received liraglutide for weight plateau had a trend of similar magnitude, this difference was not statistically significant, likely owing to a sample size of only three patients.
Gastrointestinal adverse events were especially frequent in our cohort, with 37.9% of patients reporting nausea, although only one patient discontinued the medication due to gastrointestinal side effects. This is similar to the rates of nausea reported in previous phase 3 trials investigating liraglutide for weight loss [15, 16], suggesting that patients with prior bariatric surgery are not more prone to nausea than the general population.
Limitations of our study include a retrospective analysis, heterogeneity of bariatric surgeries performed, and a relatively short trial period of 28 weeks. Moreover, our study was not designed to provide mechanistic insights into the action of liraglutide in this population. GLP-1 receptor agonists are believed to promote weight loss through central effects in the hypothalamus and delays in gastric emptying [17]. Thus, the utility of this medication in the post-bariatric surgery population has been questioned, due to elevated endogenous GLP-1 levels observed following bariatric surgery [18]. Our results show that, administration of high-dose liraglutide clearly provides additional weight-loss benefits in patients with post-bariatric surgery. Finally, there was a wide variation in the duration that passed between surgery and initiation of liraglutide. Thus, we cannot comment on the optimal time to start liraglutide post-surgery.
Conclusion
There is a growing body of data suggesting that pharmacotherapy, including liraglutide, is a useful adjunct to bariatric surgery in achieving further weight loss. Our findings support this notion. Our findings also show that a 5% “stopping rule” can be used to identify non-responders. Overall, liraglutide was well tolerated and no serious adverse events were identified. Clearly, further studies on the use of liraglutide (and other anti-obesity medications) in post-bariatric surgery patients appear warranted.
References
Sjöström L. Review of the key results from the Swedish Obese Subjects (SOS) trial—a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013;273(3):219–34.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
Sjostrom CD, Lissner L, Wedel H, et al. Reduction in incidence of diabetes, hypertension and lipid disturbances after intentional weight loss induced by bariatric surgery: the SOS Intervention Study. Obes Res. 1999;7:477–84.
De Gara CJ, Karmali S. The anatomy of a weight recidivism and revision bariatric surgical clinic. Gastroenterol Res Pract. 2014;2014:721095.
Karmali S, Brar B, Shi X, et al. Weight recidivism post-bariatric surgery: a systematic review. Obes Surg. 2013;23(11):1922–33.
Sheppard CE, Lester ELW, Chuck AW, et al. The utility of weight loss medications after bariatric surgery for weight regain or inadequate weight loss: a multi-center study. Surg Obes Relat Dis. 2017;13(3):491–500. Impact of Weight Regain. Gastroenterology Research and Practice. 2013;2013:379564
Wadden TA, Hollander P, Klein S, et al. Weight maintenance and additional weight loss with liraglutide after low-calorie-diet-induced weight loss: the SCALE maintenance randomized study. Int J Obes. 2013;37(11):1443–51.
Novo Nordisk Canada Inc. Saxenda® Product Monograph. [Internet]. 2017 [cited 2018 Feb 5]. Available from: http://www.novonordisk.ca/content/dam/Canada/AFFILIATE/www-novonordisk-ca/OurProducts/PDF/Saxenda_PM_English.pdf.
European Medicines Agency. Guideline on Clinical Evaluation of Medicinal Products used in Weight Control. [Internet]. 2014 [cited 2018 Feb 5]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2014/07/WC500170278.pdf.
Pajecki D, Halpern A, Cercato C, et al. Short-term use of liraglutide in the management of patients with weight regain after bariatric surgery. Rev Col Bras Cir. 2013;40(3):191–5.
Creange C, Lin E, Ren-Fielding C, et al. Use of liraglutide for weight loss in patients with prior bariatric surgery. Surg Obes Relat Dis. 2016;12(7):S157.
Gorgojo-martínez JJ, Feo-ortega G, Serrano-moreno C. Effectiveness and tolerability of liraglutide in patients with type 2 diabetes mellitus and obesity after bariatric surgery. Surg Obes Relat Dis. 2016;12(10):1856–63.
Stanford FC, Alfaris N, Gomez G, et al. The utility of weight loss medications after bariatric surgery for weight regain or inadequate weight loss: a multi-center study. Surg Obes Relat Dis. 2017;13(3):491–500.
Lau D et al. Early weight loss responders to liraglutide 3.0 mg had greater weight loss, regression to normoglycemia and reduced T2D development at 3 years vs. early non-responders: SCALE obesity and prediabetes. Can J Diabetes. 2016;40(5):S33.
Davies MJ, Bergenstal R, Bode B, et al. Efficacy of liraglutide for weight loss among patients with type 2 diabetes: the SCALE diabetes randomized clinical trial. JAMA. 2015;314:687–99.
Pi-sunyer X, Astrup A, Fujioka K, et al. A randomized, controlled trial of 3.0 mg of liraglutide in weight management. N Engl J Med. 2015;373(1):11–22.
Nuffer WA, Trujillo JM. Liraglutide: a new option for the treatment of obesity. Pharmacotherapy. 2015;35(10):926–34.
Laferrère B. Bariatric surgery and obesity: influence on the incretins. Int J Obes Suppl. 2016;6(Suppl 1):S32–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Author 1: The author declares no conflict of interest.
Author 2: Novo Nordisk Canada (travel and speaker fees), Shire Pharma Canada (development of educational materials, speaker fees), and Valeant Canada (travel and speaker fees).
Author 3: Novo Nordisk Canada (travel, speaker, and consultant fees), and Valeant (consultant fees).
Author 4: Novo Nordisk (travel, speaker, consultant fees, and advisory board), Merck (travel, speaker, and consultant fees), and Valeant (advisory board).
Ethics and Consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Rye, P., Modi, R., Cawsey, S. et al. Efficacy of High-Dose Liraglutide as an Adjunct for Weight Loss in Patients with Prior Bariatric Surgery. OBES SURG 28, 3553–3558 (2018). https://doi.org/10.1007/s11695-018-3393-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3393-7