Abstract
Background
Sleeve gastrectomy (LSG) is now the predominant bariatric surgery performed, yet there is limited long-term data comparing important outcomes between LSG and Roux-en-Y gastric bypass (RYGB). This study compares weight loss and impact on comorbidities of the two procedures.
Methods
We retrospectively evaluated weight, blood pressure, hemoglobin A1c, cholesterol, and medication use for hypertension, diabetes, and hyperlipidemia at 1–4 years post-operatively in 380 patients who underwent RYGB and 334 patients who underwent LSG at the University of Michigan from January 2008 to November 2013. Follow-up rates from 714 patients initially were 657 (92%), 556 (78%), 507 (71%), and 498 (70%) at 1–4 years post-operatively.
Results
Baseline characteristics were similar except for higher weight and BMI in LSG. There was greater weight loss with RYGB vs. LSG at all points. Hemoglobin A1c and total cholesterol improved more in RYGB vs. LSG at 4 years. There was greater remission of hypertension and discontinuation of all medications for hypertension and diabetes with RYGB at 4 years.
Conclusions
Weight loss, reduction in medications for hypertension and diabetes, improvements in markers of diabetes and hyperlipidemia, and remission rates of hypertension were superior with RYGB vs. LSG 4 years post-operatively. Choice of bariatric procedures should be tailored to surgical risk, comorbidities, and weight loss goals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction/Purpose
Obesity is a common disease afflicting tens of millions of Americans with far-reaching consequences. Greater than one third of the American adult population has obesity, and the prevalence of grade 3 obesity (BMI > 40 kg/m2) is increasing the fastest among any weight category with an increase of 33% from 2000 to 2012 and a prevalence of 6.1% [1]. Worldwide, obesity has more than doubled from 1980 to 2014, and 1.9 billion adults have overweight and 600 million have obesity as of 2014 [2]. The consequences of obesity are well recognized and include increased cost of care and greater risk for type 2 diabetes, hypertension, dyslipidemia, cancer, osteoarthritis, cardiovascular disease, and death [3,4,5,6]. Therefore, treating this disease has become a priority in both clinical practice and in public health policy.
Treatment for obesity can include lifestyle modifications through diet and exercise, medications, and bariatric surgery. Compared with nonsurgical approaches, more favorable weight loss, remission rates of obesity-related comorbidities, and improvement in hemoglobin A1c, blood pressure, and lipids are observed with a surgical approach [7,8,9,10]. The most serious risks of obesity (cardiovascular disease and mortality) have been shown to be reduced with bariatric surgery [3, 11,12,13].
While bariatric surgery is highly effective, the optimal weight loss surgery remains controversial. Developed in the 1970s to facilitate effective weight loss while avoiding the severe malabsorption associated with early bariatric surgery procedures, Roux-en-Y gastric bypass (RYGB), with modifications, continues to be one of the two most frequently performed weight loss surgeries worldwide [14, 15]. It has shown excellent durability for management of weight, type 2 diabetes, hypertension, and dyslipidemia [16]. Sleeve gastrectomy (LSG) was first developed as the initial step of the previously popular biliopancreatic diversion. Since gaining approval as a stand-alone procedure, it is now the most commonly performed weight loss surgery, with LSG overtaking RYGB in popularity in 2013 in the USA and in 2014 globally [14, 15, 17].
Individual studies comparing LSG and RYGB with at least moderate term follow-up generally show similar or generally greater weight loss with RYGB; similar long-term remission rates for diabetes, hypertension, and dyslipidemia; similar or greater complication rates with RYGB; and similar quality of life measurements [7, 15, 18,19,20,21,22,23,24,25,26,27,28,29,30,31]. However, these studies have been limited, to some degree, by small initial sample size, unclear definitions of comorbidity resolution/improvement, or study design. The STAMPEDE trial notably showed greater weight loss and lower medication requirements for diabetes with RYGB vs. LSG without other significant differences, although the low sample size was a clear limitation [7]. With these limitations and the shift towards a majority of patients undergoing LSG, further study is needed to answer the question of whether the two surgeries are truly “equivalent” in efficacy. With this in mind, we utilized the robust clinical data registry for our cohort, MI-BASiC (Michigan Bariatric Surgery Cohort) which was previously described and whose 2-year data have been reported [22]. We now report clinically relevant 4-year data including weight loss, metabolic parameters, and most importantly impact on obesity-related comorbidities.
Materials and Methods
Patients
We have previously described our cohort MI-BASiC (Michigan Bariatric Surgery Cohort) [22]. Briefly, consecutive patients 18 years of age or older undergoing RYGB or LSG for obesity at the University of Michigan between January 2008 and November 2013 were included in our retrospective study. All patients had either BMI > 40 kg/m2 or an obesity-related comorbidity and BMI > 35 kg/m2. Exclusion criteria included previous weight loss surgery, inability to complete the surgery related to unexpected operative finding, or surgery performed for a reason other than obesity and its related comorbidities. Based on these criteria, 380 patients were included for RYGB (304 female) and 334 for LSG (259 female). The number of included patients is slightly lower than our prior study (383 patients in RYGB and 336 for LSG) due to the finding on more detailed chart review that the now excluded patients had surgery for a different indication or had prior weight loss surgery [22]. Institutional review board approval was obtained, and informed consent was not required due to the nature of the investigation.
Data Collection
In the multidisciplinary University of Michigan Adult Bariatric Surgery Program, patients undergo a rigorous preoperative evaluation and are followed postoperatively with the surgeon and dietitians at 2 weeks and 2 months. Subsequent follow-up is with the endocrinologist and dietitian at the Post-Bariatric Endocrine Clinic where patients are asked to present at 6 months postoperatively, 12 months postoperatively, and annually thereafter to evaluate and treat long-term care issues including weight regain, vitamin deficiencies, and obesity-related comorbidities.
Retrospective electronic medical review was performed, and data were abstracted from visits that occurred preoperatively (within 60 days prior to surgery) and annually postoperatively at 1 to 4 years (± 180 days). Additional follow-up from our prior publication was obtained by manual chart review as augmentation to prior automatic data abstraction. Baseline demographic characteristics collected included sex and age. Data collected at baseline and follow-up, when available, included weight, height, BMI, blood pressure, HbA1c, lipids, and medication use for diabetes, hypertension, and dyslipidemia. The number of medications was recorded at each time point when available, and if a medication dose was reduced this was also captured as was the discontinuation of all medications for the specified obesity-related comorbidity. Remission of diabetes was defined as hemoglobin A1c less than 6.5% without medications for diabetes, which is consistent with the definition set forth by the American Diabetes Association for partial remission of diabetes, although patients in our study were required to have only a single hemoglobin A1c less than 6.5% rather than 1 year of such measurements [32]. Remission of hypertension was defined as blood pressure less than 140/90 without medications for hypertension. A decrease in medications was defined as a dose reduction and/or fewer medications for the specified condition. Excess body weight loss (%) was calculated by dividing total weight loss by the difference between actual body weight and ideal body weight, which is the weight at a BMI of 25 kg/m2 for each patient. Thirty-day surgical complications and healthcare utilization were collected by electronic medical record review. Specific definitions for complications and utilization were previously reported [22].
Statistical Analysis
Continuous data are reported as mean (standard error of the mean). Changes in laboratory data, weight, BMI, blood pressure, and medication use were compared between procedures by the Mann-Whitney-Wilcoxon rank sum test. Comorbidity resolution/remission and categorical evaluation of medication use were compared by a two-tailed Fisher’s exact test. P values are reported for each test, and threshold for statistical significance was set at < 0.05. Analyses were performed using SAS 9.4.
Results
Baseline Characteristics
The study population (MI-BASiC cohort) included 714 patients (563 females, 79%) with mean age of 44 years and baseline BMI of 48.4 kg/m2. Baseline characteristics (Table 1) were similar between the two groups except BMI and weight, which were significantly greater in the LSG group. In RYGB, 131 patients were being treated for diabetes (34.4%), 201 were prescribed anti-hypertensives (52.9%), and 101 were treated for dyslipidemia (26.6%). The corresponding presence of comorbidities in LSG at baseline were 100 (29.9%), 182 (54.5%), and 97 (29.0%) patients, respectively. There were no significant differences in the presence of comorbidities at baseline.
Data Availability
Table 2 shows data availability at baseline and at 1 through 4 years postoperatively. For weight/BMI, SBP, A1c, and cholesterol, percent data availability was calculated using the number of patients having weight/BMI data at baseline as the denominator. For “SBP in HTN,” the number of patients having HTN at baseline within the respective group was used as the denominator. Similarly, for “A1c in DM,” the number of patients having DM at baseline in the group was used as the denominator.
Weight Loss and Metabolic Parameters
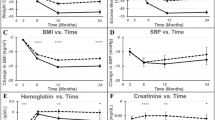
Figure 1a–c shows a comparison of total weight loss (TWL) in kilograms, percent TWL, and percent excess weight loss (EWL) between LSG and RYGB with SEM provided as error bars in the figures and below for select values. At 1 year after surgery, patients undergoing RYGB lost 40.4 ± 0.8 kg of total weight, 30.4 ± 0.5% of total weight, and 68.5 ± 1.2% of excess weight while patients in the LSG group lost 34.3 ± 0.9 kg, 24.2 ± 0.6%, and 51.5 ± 1.3% respectively with p values < 0.0001 for all weight-related measures. Differences were preserved at 4 years post-operatively at which time RYGB patients lost 34.4 ± 1.1 kg of total weight, 25.7 ± 0.7% of total weight, and 57.6 ± 1.5% EWL vs. LSG patients who lost 26.7 ± 1.2 kg, 18.6 ± 0.7%, and 38.5 ± 1.5% with p values < 0.0001 for all measures. Patients in both groups had clear weight regain/obesity recidivism over time.
Comparison of weight and metabolic outcomes of sleeve gastrectomy (LSG, dotted line) vs. Roux-en-Y gastric bypass (RYGB, solid line). All graphs show change in the specified variable over time rather than absolute values. Error bars represent SEM. SBP systolic blood pressure. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001 for comparison between procedures
Figure 1d–f shows a comparison of hemoglobin A1c, total cholesterol, and systolic blood pressure between LSG and RYGB. Decreases in A1c were consistent over time in RYGB with reductions ranging from 0.91 to 1.12% (± 0.16% at 4 years), while the improvements in A1c in LSG decreased over time from an A1c reduction of 0.73% at 1 year to 0.45% at 4 years (± 0.10% at 4 years). The p value for comparison between the two groups at 4 years was 0.004. Total cholesterol at 4 years decreased 0.3 ± 5.4 mg/dL in RYGB and increased 12.7 ± 3.6 mg/dL in LSG (p = 0.01). In fact, mean cholesterol was higher than baseline at all timepoints following LSG and lower than baseline at all timepoints following RYGB, although it was quite close to baseline at 4 years in RYGB. Systolic blood pressure at 1 year decreased similarly in both groups with a 14.2 ± 1.2 mmHg decrease with RYGB and 11.5 ± 1.3 mmHg decrease with LSG (p = 0.13). Improvements lessened over time with 4 year SBP decreases of 8.8 ± 1.3 mmHg with RYGB and 7.3 ± 1.6 mmHg with LSG (p = 0.66). Only at 3 years was there a significant difference in favor of RYGB at which point SBP decreased 12.6 ± 1.3 mmHg vs. 6.5 ± 1.5 mmHg (p = 0.001).
Effect on Obesity-Related Comorbidities
Figure 2 compares changes in hemoglobin A1c in patients with diabetes at baseline (Fig. 2a) and changes in systolic blood pressure in patients with hypertension at baseline (Fig. 2b), rather than examining these variables in the entire cohort as in Fig. 1. Among patients with diabetes, hemoglobin A1c improvements at 1 year were 1.51 ± 0.17% in RYGB and 0.89 ± 0.14% in LSG (p = 0.01) while improvements at 4 years were 1.28% (± 0.21%) vs. 0.45% (± 0.15%) (p = 0.002). Among patients with hypertension, systolic blood pressure improved 10.5 ± 1.8 mmHg with RYGB vs. 8.4 ± 1.9 mmHg with LSG at 1 year (p = 0.42) and improved 5.3 ± 1.9 mmHg with RYGB vs. 4.1 ± 2.4 mmHg with LSG at 4 years (p = 0.92).
Table 3 compares the efficacy of LSG and RYGB in our cohort for obesity-related comorbidities including diabetes, hypertension, and hyperlipidemia at 3 and 4 years post-operatively. Patients who achieved remission are included within the group of patients who discontinued all medications.
Effect of Follow-Up Duration
Among patients who followed up for 4 years vs. those who did not, baseline weight in RYGB was 131.7 (± 1.5) kg vs. 138.0 (± 3.3) kg respectively (p = 0.13) and in LSG was 141.9 (± 3.3) kg vs. 139.7 (± 1.8) kg respectively (p = 0.48). In RYGB, age and baseline hemoglobin A1c were modestly lower in patients who did not follow-up at 4 years while there were no significant differences in other relevant baseline characteristics in RYGB or LSG among patients lost to follow-up. Total weight loss at 3 years in RYGB patients who followed up at 4 years was 27.2 vs. 31.7% in those who did not, and in LSG, corresponding total weight loss was 20.5 vs. 24.6% (p > 0.05 for both surgeries).
Discussion
Reports of outcomes comparing sleeve gastrectomy and Roux-en-Y gastric bypass at 4 years of follow-up are scarce due to the widespread adoption of LSG only after 2010 [15]. This is one of the largest studies to compare the procedures and utilizes a cohort that includes consecutive patients in nearly equal numbers and includes comparisons of weight loss, metabolic outcomes, and impact on comorbidities, with acute complications data from this cohort having been previously described [22].
Significantly greater weight loss by all parameters (TWL, % TWL, and % EWL) was observed with RYGB in our cohort and is clinically significant.
Markers of comorbidities in the entire cohort generally favored RYGB, specifically with significantly improved hemoglobin A1c at 1, 2, and 4 years. While this particular measure does not incorporate medication use or whether the patient had diabetes initially, it provides an important measure of the overall impact on dysglycemia in all consecutive patients as A1c is directly and continuously related to risk of progression to diabetes and the risk of microvascular complications, which can occur in patients with diabetes or prediabetes [33, 34]. Among patients with diabetes at baseline, a similar trend in favor of RYGB is observed with statistical significance at all timepoints except for 3 years and corresponding clinical significance with a 0.83% absolute difference in average A1c for RYGB vs. LSG at 4 years. The remission rate for diabetes did not differ significantly between RYGB and LSG at 3 or 4 years. However, more patients were able to discontinue all medications for diabetes in RYGB at 4 years vs. LSG (Table 3).
Total cholesterol increased in LSG and decreased in RYGB at all timepoints. While it was unexpected to see an increase in total cholesterol with LSG, it does reflect other studies which show a more beneficial effect on lipids with RYGB [35]. Significant differences were found in favor of RYGB at all timepoints. With less data available and a desire to set a strict definition for hyperlipidemia remission, we did not evaluate changes in cholesterol exclusively in patients with hyperlipidemia or determine remission rates for hyperlipidemia. More patients in RYGB were able to decrease the number and/or dose of medications (p = 0.009) or discontinue all medications (p = 0.02) at 3 years with no significant difference at 4 years.
Systolic blood pressure improved significantly in both groups. For the entire cohort, and in patients with baseline hypertension, the only significant difference in SBP was at 3 years in favor of RYGB. Importantly, more patients in RYGB experienced remission of hypertension at 3 and 4 years and more patients discontinued all medications for hypertension at 3 and 4 years vs. LSG.
Validation of our results by comparison to other studies is challenging as study populations have important differences. The longest reported follow-up for LSG is 8 years, and while this study reports greater excess weight loss than we observed, patients had a much lower baseline BMI (42.8 vs. 49.8 kg/m2) which is known to significantly impact the excess weight loss. Also, many of the surgeries were revisions, which would have been excluded from our data [36, 37]. A study of LSG with similar baseline characteristics as our patient population showed similar weight loss and diabetes remission at 5 vs. 4 years in our study [38]. Comparisons to important studies involving RYGB also have important differences in baseline factors that affect outcome. For example, we observed greater weight loss for RYGB at 4 years than patients in the STAMPEDE trial at 5 years; however, this is confounded by lower baseline BMI and longer follow-up duration in the STAMPEDE trial [7].
Limitations to the study include incomplete data availability, although the available weight and blood pressure measurements are satisfactory for this population which typically has high attrition rates, and patients lost to follow-up had similar baseline weight and weight loss trajectories as those who followed up through the end of the study. We did not take into account long-term complications of the surgeries including ulcers, hypoglycemia, dumping syndrome, vitamin deficiencies, and quality of life for which an alternative approach to obtaining the comparative data would be needed, although short-term complications have been reported [22]. Quality of life has been evaluated in other studies with no difference found in a recent systematic review [39]. Patient selection may have factored into which intervention each patient had as it was not a randomized trial. One potential limitation in the interpretation of these results is the higher baseline BMI and weight in LSG, which likely reflects initial insurance coverage for LSG only for patients with BMI > 50 kg/m2. Additionally, operative risk is higher with increased BMI [40], and with higher complication rates with RYGB, providers may choose LSG preferentially for patients with greater BMI. Prior analyses of patients stratified by BMI show that lower pre-operative weight (as in RYGB in our cohort) predicts lower % TWL, which actually strengthens our results demonstrating clearly superior weight loss with RYGB [41]. Percent excess weight loss, however, must be cautiously interpreted as patients with higher baseline weight (as in LSG in our cohort) do have less robust weight loss by this measure [37].
Strengths of the study include large sample size, sequential patient inclusion which makes the results more applicable to typical patient populations without the stringent requirements for randomized clinical trials, moderate- to long-term follow-up of 4 years, unique timespan which allowed for nearly equal cohort sizes in a similar era, and measurement of important variables including weight, markers of comorbidities, medication use and remission for comorbidities, and short-term complication rates.
For the future, we hope to follow the patients further and learn more about the sustainability of the beneficial effects seen with these surgeries. The results of our cohort and recent systematic reviews favor RYGB for weight loss and improvements in obesity-related comorbidities at the expense of increased complications [35, 39, 42]. Though the difference may be appearing to close over time, the long-term data availability from both randomized studies and nonrandomized cohorts decreases over time which may limit the conclusions. With future analyses and greater resources directed to reaching patients lost to follow-up, we hope to shed light on patient characteristics that would aid in the decision for surgery type. The duration of the observed differences for 4 years may be significant enough to create long-lasting metabolic legacy effects even if the differences were to close in the next decade, almost reminiscent of the legacy effects carried over from the Diabetes Control and Complications Trial or the United Kingdom Prospective Diabetes Study [43, 44].
Conclusion
In our cohort, Roux-en-Y gastric bypass compared with sleeve gastrectomy offers superior weight loss, glycemic control, cholesterol levels, remission of hypertension, and reduction in medication usage for diabetes at 4 years post-operatively in patients who return for follow up. Our data points to the need to conduct careful long-term studies to allow full characterization of benefits and risks of both surgeries.
References
An R. Prevalence and trends of adult obesity in the US, 1999-2012. ISRN Obes. 2014;2014:185132.
Organization WH. Obesity and overweight fact sheet. 2016 [July 6, 2017]; Available from: http://www.who.int/mediacentre/factsheets/fs311/en/.
Boido A, Ceriani V, Cetta F, et al. Bariatric surgery and prevention of cardiovascular events and mortality in morbid obesity: mechanisms of action and choice of surgery. Nutr Metab Cardiovasc Dis. 2015;25(5):437–43.
Global BMIMC, Di Angelantonio E, Bhupathiraju Sh N, et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388(10046):776–86.
Wang YC, McPherson K, Marsh T, et al. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet (London, England). 2011;378(9793):815–25.
Lehnert T, Sonntag D, Konnopka A, et al. Economic costs of overweight and obesity. Best Pract Res Clin Endocrinol Metab. 2013;27(2):105–15.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes—5-year outcomes. N Engl J Med. 2017;376(7):641–51.
Ribaric G, Buchwald JN, McGlennon TW. Diabetes and weight in comparative studies of bariatric surgery vs conventional medical therapy: a systematic review and meta-analysis. Obes Surg. 2014;24(3):437–55.
Ikramuddin S, Korner J, Lee WJ, et al. Lifestyle intervention and medical management with vs without Roux-en-Y gastric bypass and control of hemoglobin A1c, LDL cholesterol, and systolic blood pressure at 5 years in the diabetes surgery study. JAMA. 2018;319(3):266–78.
Jakobsen GS, Smastuen MC, Sandbu R, et al. Association of bariatric surgery vs medical obesity treatment with long-term medical complications and obesity-related comorbidities. JAMA. 2018;319(3):291–301.
Kwok CS, Pradhan A, Khan MA, et al. Bariatric surgery and its impact on cardiovascular disease and mortality: a systematic review and meta-analysis. Int J Cardiol. 2014;173(1):20–8.
Pontiroli AE, Morabito A. Long-term prevention of mortality in morbid obesity through bariatric surgery. A systematic review and meta-analysis of trials performed with gastric banding and gastric bypass. Ann Surg. 2011;253(3):484–7.
Reges O, Greenland P, Dicker D, et al. Association of bariatric surgery using laparoscopic banding, Roux-en-Y gastric bypass, or laparoscopic sleeve gastrectomy vs usual care obesity management with all-cause mortality. JAMA. 2018;319(3):279–90.
Deitel M. History of bariatric surgery. In: Korenkov M, editor. Bariatric surgery: technical variations and complications. Berlin: Springer; 2012. p. 1–9.
Melissas J, Stavroulakis K, Tzikoulis V, et al. Sleeve gastrectomy vs Roux-en-Y gastric bypass. Data from IFSO-European Chapter Center of Excellence Program. Obes Surg. 2017;27(4):847–55.
Adams TD, Davidson LE, Litwin SE, et al. Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med. 2017;377(12):1143–55.
Spaniolas K, Kasten KR, Brinkley J, et al. The changing bariatric surgery landscape in the USA. Obes Surg. 2015;25(8):1544–6.
Dicker D, Yahalom R, Comaneshter DS, et al. Long-term outcomes of three types of bariatric surgery on obesity and type 2 diabetes control and remission. Obes Surg. 2016;26(8):1814–20.
Dogan K, Gadiot RP, Aarts EO, et al. Effectiveness and safety of sleeve gastrectomy, gastric bypass, and adjustable gastric banding in morbidly obese patients: a multicenter, retrospective, matched cohort study. Obes Surg. 2015;25(7):1110–8.
Ignat M, Vix M, Imad I, et al. Randomized trial of Roux-en-Y gastric bypass versus sleeve gastrectomy in achieving excess weight loss. Br J Surg. 2017;104(3):248–56.
Lee WJ, Pok EH, Almulaifi A, et al. Medium-term results of laparoscopic sleeve gastrectomy: a matched comparison with gastric bypass. Obes Surg. 2015;25(8):1431–8.
Lager CJ, Esfandiari NH, Subauste AR, et al. Roux-En-Y gastric bypass vs. sleeve gastrectomy: balancing the risks of surgery with the benefits of weight loss. Obes Surg. 2017;27(1):154–61.
Pekkarinen T, Mustonen H, Sane T, et al. Long-term effect of gastric bypass and sleeve gastrectomy on severe obesity: do preoperative weight loss and binge eating behavior predict the outcome of bariatric surgery? Obes Surg. 2016;26(9):2161–7.
Perrone F, Bianciardi E, Benavoli D, et al. Gender influence on long-term weight loss and comorbidities after laparoscopic sleeve gastrectomy and Roux-en-Y gastric bypass: a prospective study with a 5-year follow-up. Obes Surg. 2016;26(2):276–81.
Zhang Y, Zhao H, Cao Z, et al. A randomized clinical trial of laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy for the treatment of morbid obesity in China: a 5-year outcome. Obes Surg. 2014;24(10):1617–24.
Jimenez A, Casamitjana R, Flores L, et al. Long-term effects of sleeve gastrectomy and Roux-en-Y gastric bypass surgery on type 2 diabetes mellitus in morbidly obese subjects. Ann Surg. 2012;256(6):1023–9.
Yang J, Wang C, Cao G, et al. Long-term effects of laparoscopic sleeve gastrectomy versus Roux-en-Y gastric bypass for the treatment of Chinese type 2 diabetes mellitus patients with body mass index 28-35 kg/m(2). BMC Surg. 2015;15:88.
Tang Q, Sun Z, Zhang N, et al. Cost-effectiveness of bariatric surgery for type 2 diabetes mellitus: a randomized controlled trial in China. Medicine (Baltimore). 2016;95(20):e3522.
Kehagias I, Karamanakos SN, Argentou M, et al. Randomized clinical trial of laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy for the management of patients with BMI < 50 kg/m2. Obes Surg. 2011;21(11):1650–6.
Peterli R, Wölnerhanssen B, Peters T, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity: the SM-boss randomized clinical trial. JAMA. 2018;319(3):255–65.
Salminen P, Helmiö M, Ovaska J, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss at 5 years among patients with morbid obesity: the sleevepass randomized clinical trial. JAMA. 2018;319(3):241–54.
Buse JB, Caprio S, Cefalu WT, et al. How do we define cure of diabetes? Diabetes Care. 2009;32(11):2133–5.
Zhang X, Gregg EW, Williamson DF, et al. A1C level and future risk of diabetes: a systematic review. Diabetes Care. 2010;33(7):1665–73.
Chawla A, Chawla R, Jaggi S. Microvasular and macrovascular complications in diabetes mellitus: distinct or continuum? Indian J Endocrinol Metab. 2016;20(4):546–51.
Li J, Lai D, Wu D. Laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy to treat morbid obesity-related comorbidities: a systematic review and meta-analysis. Obes Surg. 2016;26(2):429–42.
Noel P, Nedelcu M, Eddbali I, et al. What are the long-term results 8 years after sleeve gastrectomy? Surg Obes Relat Dis. 2017;13(7):1110–5.
Still CD, Wood GC, Chu X, et al. Clinical factors associated with weight loss outcomes after Roux-en-Y gastric bypass surgery. Obesity (Silver Spring, Md). 2014;22(3):888–94.
Nedelcu M, Loureiro M, Skalli M, et al. Laparoscopic sleeve gastrectomy: effect on long-term remission for morbidly obese patients with type 2 diabetes at 5-year follow up. Surgery. 2017;162(4):857–62.
Ettleson MD, Lager CJ, Kraftson AT, et al. Roux-en-Y gastric bypass versus sleeve gastrectomy: risks and benefits. Minerva Chir. 2017;72(6):505–19.
Maciejewski ML, Winegar DA, Farley JF, et al. Risk stratification of serious adverse events after gastric bypass in the bariatric outcomes longitudinal database. Surg Obes Relat Dis. 2012;8(6):671–7.
Sczepaniak JP, Owens ML, Shukla H, et al. Comparability of weight loss reporting after gastric bypass and sleeve gastrectomy using BOLD data 2008-2011. Obes Surg. 2015;25(5):788–95.
Li JF, Lai DD, Lin ZH, et al. Comparison of the long-term results of Roux-en-Y gastric bypass and sleeve gastrectomy for morbid obesity: a systematic review and meta-analysis of randomized and nonrandomized trials. Surg Laparosc Endosc Percutan Tech. 2014;24(1):1–11.
Nathan DM, Cleary PA, Backlund JY, et al. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353(25):2643–53.
Holman RR, Paul SK, Bethel MA, et al. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359(15):1577–89.
Acknowledgements
The authors would like to acknowledge the surgeons of the University of Michigan Health System (UMHS) bariatric surgery program who operated on our cohort: Jonathan Finks MD, Justin Dimick MD, and John Birkmeyer MD as well as the physician assistants Kendra Rogers PA-C and Clare Gargaro PA-C. We are also grateful for the dedication and care provided by the entire clinical staff of the UMHS Bariatric Surgery Program and the Division of Metabolism, Endocrinology, and Diabetes. Finally, we would like to thank all of our patients who have participated in the UMHS Bariatric Surgery Program and followed in our post-bariatric surgery clinic.
Funding
The study was supported by the Parker Family Foundation and the University of Michigan Health System as discretionary funding to Dr. Oral.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Kraftson is a clinical investigator for a study sponsored by Nestle. Dr. Varban receives salary support from Blue Cross Blue Shield of Michigan for leading quality improvement efforts within the Michigan Bariatric Surgery Collaborative. Dr. Oral has received grant support from Aegerion Pharmaceuticals, Ionis Pharmaceuticals, Akcea Therapeutics, Gemphire, GI Dynamics, and AstraZeneca; has been a consultant or advisor for AstraZeneca, BMS, TheraTherapeutics, Regeneron, and Aegerion; and has received drug or other nonmaterial support from Aegerion Pharamaceuticals, Akcea Therapeutics, Rhythm Pharmaceuticals, and Boehringer Ingelheim. All other authors have no conflict of interest to disclose.
Ethics
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent Statement
This retrospective data analysis is exempt from informed consent. Our study was approved by the IRB prior to any data collection.
Rights and permissions
About this article
Cite this article
Lager, C.J., Esfandiari, N.H., Luo, Y. et al. Metabolic Parameters, Weight Loss, and Comorbidities 4 Years After Roux-en-Y Gastric Bypass and Sleeve Gastrectomy. OBES SURG 28, 3415–3423 (2018). https://doi.org/10.1007/s11695-018-3346-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3346-1