Abstract
Background
Initial weight loss after bariatric surgery has been associated with improvements in reproductive hormones and sexual functioning in women. Few studies have investigated the durability of these changes.
Objectives
The objective of this paper is to investigate changes in sex hormones, sexual functioning, and relevant psychosocial constructs over 4 years in women who underwent bariatric surgery.
Setting
The setting is a prospective cohort of 106 women from the Longitudinal Assessment of Bariatric Surgery consortium.
Methods
Changes in sex hormones were assessed by blood assay. Sexual functioning, quality of life (QOL), body image, depressive symptoms, and marital adjustment were assessed by psychometric measures.
Results
Women lost on average (95% confidence interval) 32.3% (30.4%, 34.3%) at postoperative year 3 and 30.6% (28.5%, 32.8%) at postoperative year 4. Compared to baseline, women experienced significant changes at 4 years in all hormones assessed, except estradiol. Women reported significant improvements in sexual functioning (i.e., arousal, desire, and satisfaction) through year 3, but these changes were not maintained through year 4. Changes in relationship quality followed a similar pattern. Improvements in physical aspects of QOL, body image, and depressive symptoms were maintained through 4 years.
Conclusions
Improvements in reproductive hormones and physical aspects of QOL, body image, and depressive symptoms were maintained 4 years after bariatric surgery. Improvements in sexual functioning, relationship satisfaction, and mental components of QOL eroded over time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Initial weight losses typically seen with bariatric surgery are associated with improvements in morbidity, mortality, and psychosocial status [1,2,3]. Many of these benefits are observed before individuals reach their maximum weight loss and endure as weight plateaus [4]. Benefits in quality of life (QOL), for example, are largely maintained through the first postoperative decade, with only modest erosion over time for most individuals [5, 6].
Sexual health is an important element of QOL [4]. Obesity can have a detrimental impact on both reproductive hormones and sexual functioning for women and men [7, 8]. For example, adiposity is associated with higher levels of estradiol and total testosterone, which can inhibit sexual response. Both the modest weight losses seen with non-surgical treatment of obesity, and the more substantial weight losses seen with bariatric surgery, have been associated with improvements in these reproductive hormones [9,10,11,12]. We recently found that a surgically induced weight loss of 33% of total body weight was associated with significant decreases in estradiol, total testosterone, and DHEA-S as well as significant increases in FSH, LH, and SHGB in women 2 years after surgery [9]. These women also reported significant improvements in most domains of sexual functioning, as well as improvements in health- and weight-related QOL, body image, and depressive symptoms [9].
Little is known about the longer term durability of these improvements. Within the first postoperative decade, some patients are likely to have maintained their weight loss while others have regained variable amounts of weight. This paper reports on changes in sex hormones, sexual function, and related psychosocial variables 4 years after bariatric surgery.
Methods
Study Design
The study was an ancillary investigation to the Longitudinal Assessment of Bariatric Surgery (LABS) consortium and which investigated long-term outcomes of bariatric surgery [13,14,15,16].
One hundred and six women from two study sites (the Neuropsychiatric Research Institute [NRI] and the University of Pittsburgh Medical Center [UPMC]) were recruited. Participants were assessed prior to surgery and annually through the first four postoperative years. Year 2 was the primary point of postoperative interest. The present study investigated changes 3 and 4 years after surgery, which was the proposed duration of the study. The trial was approved by the Institutional Review Boards at NRI, UPMC, and the University of Pennsylvania. Informed consent was obtained.
Participants
Participants met the general clinical criteria for bariatric surgery as well as the specific inclusion criteria of the study [8, 9, 17]. At the time of enrollment, women had to report involvement in a relationship that included sexual activity and for at least 12 months duration. This allowed for methodological control of a consistent opportunity for sexual activity with a partner. Women received a gift card for completing each assessment.
Measures
Participants underwent blood draws and completed questionnaires at baseline and again annually for 4 years. These measures are described in detail in previous reports from this study [8, 9, 17]; they are described in brief below.
Blood samples were obtained after an overnight fast. They were assessed at the Clinical Translational Research Center at the University of Pennsylvania. Hormones associated with sexual and reproductive functioning were assessed by standard methods.
Participants also completed a number of validated and widely used psychometric measures. The Female Sexual Function Index (FSFI) assessed several domains of sexual functioning: desire, arousal, lubrication, orgasm, satisfaction, and pain [18, 19]. Lower scores indicate poorer function. The Short Form Health Survey-36-item version (SF-36) assessed health-related quality of life (HRQOL) [20]. The Impact of Weight on Quality of Life-Lite (IWQOL-Lite) was used to measure weight-related QOL [21,22,23]. The Body Image Quality of Life Inventory (BIQLI) measured the body image quality of life [24]. The Body Shape Questionnaire (BSQ) was used to evaluate dissatisfaction with body shape [25]. The Dyadic Adjustment Scale assessed domains of romantic relationship satisfaction [26]; unfortunately, the measure did not assess changes in relationship status over the course of the study. Beck Depression Inventory-I (BDI-I) assessed depressive symptoms [27].
Statistical Analyses
The analytic approach was similar to that used in other outcome studies from the LABS consortium. It was selected again here to facilitate uniform interpretation of results across studies. It is summarized briefly here.
Descriptive statistics summarized baseline characteristics of participants. A mixed model was used to report the changes over time. Pairwise comparisons were made between baseline and each follow-up time point; corrections for multiple comparisons are detailed in the tables. The reported modeling values and changes account for missing data. The observed mean and standard deviation are reported in the Supplementary Tables. Growth mixture models estimated changes in total FSFI score over time. The Bayesian Information Criteria (BIC), minimum class size, entropy, and interpretability were all used to determine the groups. The modeled trajectories were plotted with bars indicating the interquartile range (IQR) of the observed total FSFI score at each time point. Analyses were conducted using SAS (Statistical Analysis System, version 9.4) and Mplus (version 7). All reported P values are two-sided. P values less than 0.05 were considered statistically significant.
Results
Demographic Characteristics
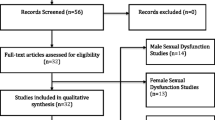
Baseline demographic and descriptive characteristics were detailed in the baseline paper and are presented in again Table 1 to assist with interpretation [8]. Participants had a median BMI of 44.5 kg/m2. The sample was predominately white (96%) and well educated (75% with some college experience). Figure 1 displays the enrollment and participant retention. Participants were considered as having data at any point in time if any single measurement was obtained.
Weight Loss
Women lost, on average (95% confidence interval), 32.8% (30.7%, 34.8%) of initial body weight at year 1, 33.4% (31.5%, 35.4%) at year 2, 32.3% (30.4%, 34.3%) at year 3, and 30.6% (28.5%, 32.8%) at year 4. The difference in percent weight change from year 1 to year 4, 2.2% (0.8%, 3.5%), was statistically significant (P = 0.003).
Sex Hormones
The sex hormone data are presented in Table 2. Women had significant improvements in all but one of the hormones of interest (DHEA-S) at the end of the first postoperative year. At postoperative years 2, 3, and 4, all hormones were significantly improved from baseline with the exception of estradiol.
Sexual Functioning
Participants reported significant improvement from baseline to years 1, 2, and 3 as seen with the total FSFI score, as well as the arousal, desires, and satisfaction domain subscale scores (see Table 2). Changes on the orgasm subscale, while suggesting improvement, did not reach statistical significance. By postoperative year 4, none of the changes in sexual functioning remained statistically significant.
Changes in the FSFI scores over time are represented in Fig. 2. Five unique groups characterize the changes. Group 1 (n = 40; 38.8%) represents women with no sexual dysfunction at baseline and no significant change over time. The small number of women in group 2 (n = 8) reported sexual dysfunction at baseline (FSFI total ≤ 26) and experienced a worsening of their sexual functioning within the first year of surgery. Their functioning improved over time but remained below baseline levels throughout. Women in group 3 (n = 28; 27.2%) reported moderate to poor levels of sexual functioning at baseline and no change over time. The average woman in group 4 (n = 12; 11.7%) had a sexual dysfunction prior to surgery. She experienced a statistically and clinically significant improvement in sexual functioning at postoperative years 1, 2, and 3. By postoperative year 4, the women in this group had higher sexual function than those at baseline but were still characterized as having sexual dysfunction (FSFI total ≤ 26). Women in group 5 (n = 15; 14.6%) experienced low sexual functioning at baseline and all postoperative years.
Psychosocial Variables
Table 3 presents the psychosocial variables. Statistically significant improvements in almost all domains of health and weight-related QOL were reported at all postoperative time points and as compared to preoperative levels. The exceptions were the mental component summary and mental health subscales of the SF-36. Women also reported statistically significant improvements in body image and depressive symptoms throughout the four postoperative assessments. Women reported statistically significant improvements in overall relationship satisfaction and the Affectional Expression subscale of the DAS through postoperative year 3. Dyadic Consensus was significantly improved through year 2, but the improvements were not statistically significant by postoperative year 4.
Discussion
This study provides new information on the durability of changes in sex hormones, sexual functioning, and psychosocial functioning in women 4 years after bariatric surgery. Participants lost, on average, 30% of their body weight 4 years after surgery, as typically seen after bariatric surgery. Women experienced significant improvements in most reproductive hormones of interest. They reported significant improvements in overall sexual functioning and sexual arousal, desire, and satisfaction through the first three postoperative years. However, these reported benefits did not differ from baseline at postoperative year 4. Improvements in most domains of health-related QOL, weight-related QOL, body image, and depressive symptoms continued through the fourth postoperative year.
As we previously reported, women experienced statistically significant improvements in reproductive hormones 2 years after surgery [9]. All of these improvements endured at the third and fourth postoperative year. The present results suggest that the early improvements in these hormones remain while women maintain relative weight stability following the large weight loss typically seen with bariatric surgery.
Women reported significant improvements in overall sexual functioning, as well as improvements in sexual desire, arousal, and satisfaction with their sexual functioning 2 years after bariatric surgery [9]. At postoperative year 3, these improvements were maintained. By the fourth postoperative year, when women had experienced a statistically significant weight regain compared to postoperative year 1, these changes no longer differed from baseline. Women who reported the poorest quality of sexual functioning prior to surgery reported dramatic improvements in functioning 1 year after surgery and comparable to those women who reported the highest quality of functioning before surgery. However, the sexual function of this group of women declined during years 2 through 4.
Previous studies have found self-reported improvements in QOL, body image, and depressive symptoms in the first 2 years following bariatric surgery, when patients are at or near their maximum weight loss [3, 28, 29]. The present study extends this research and suggests that most of these benefits are well maintained through the first four postoperative years even as patients regain some weight. The exceptions to this were the Mental Health subscale and Mental Component summary scores of the SF-36, which at postoperative years 3 and 4 did not significantly differ from baseline. It may be that even a modest weight regain years after bariatric surgery is emotionally upsetting to women. Although speculative, it may be that these women are experiencing some anticipatory emotional distress—a concern that they have started on a trajectory of weight regain which may progress over time.
The erosion in self-reported sexual functioning at postoperative year 4 is both surprising and challenging to interpret. As noted above, women did not experience a change in sex hormones that could account for the change in sexual functioning. Age also was unrelated to changes in sexual functioning or reproductive hormones. Women did experience a statistically significant weight gain from year 1 to year 4, although whether or not the 2.2% change in weight is large enough to impact sexual behavior is open for discussion and further study. Some of the early changes in marital satisfaction that women reported in the first two or three postoperative years were no longer statistically significant at postoperative year 4. In our investigation of changes in male sex hormones and sexual behavior, we found a similar pattern of results—significant changes in relevant sex hormones and several domains of psychosocial functioning, but no statistically significant changes in self-reported sexual functioning [17]. Sexual behavior and satisfaction are strongly associated with more general relationship satisfaction [4], thus the need to consider and assess both the physiological and psychosocial contributions to sexual functioning.
The present study extends previous investigations in this area, most of which have only reported 1- or 2-year outcomes. However, the study has some limitations. Women studied were almost exclusively white and had a high level of education. While this is true of many studies in bariatric surgery, the nature of the sample limits our ability to comment on the variables of interest in non-white women. We also experienced some loss to follow-up, where participants completed some, but not all, of the study measurements. The absence of reliable information on menstrual or menopause status, including changes over the 4 years, leaves us unable to comment on how changes in reproductive hormones may be associated with menopause status. We also were not able to comment on changes in relationship status over the course of the study. The inclusion of weight stable comparison group also would have added additional methodological rigor to the study.
Regardless, the study provides new information on the durability of improvements in reproductive hormones, sexual functioning, and more general psychosocial functioning in women 4 years after bariatric surgery. Early improvements in sex hormones and most domains of psychosocial functioning endure over time. While self-reported improvements in sexual functioning were maintained for the first three postoperative years, the changes no longer differed from baseline by postoperative year 4. Thus, women who undergo bariatric surgery should be counseled that the early changes in sexual functioning may not endure over time. Future studies are needed to confirm these observations as well as to assess the potential role of other variables, such as age or relationship-related changes, that may have contributed to the loss of these benefits.
References
Adams TD, Davidson LE, Litwin SE, et al. Gastrointestinal surgery: cardiovascular risk reduction and improved long-term survival in patients with obesity and diabetes. Curr Atheroscler Rep. 2012 Dec;14(6):606–15. https://doi.org/10.1007/s11883-012-0286-4.
Courcoulas AP, Christian NJ, Belle SH, et al. Three year weight and health outcomes in the Longitudinal Assessment of Bariatric Surgery (LABS) consortium. JAMA. 2013 Dec 11;310(22):2416–25. https://doi.org/10.1001/jama.2013.280928.
Sarwer DB, Wadden TA, Fabricatore AN. Psychosocial and behavioral aspects of bariatric surgery. Obes Res. 2005;13(4):639–48. https://doi.org/10.1038/oby.2005.71.
Sarwer DB, Lavery M, Spitzer JC. A review of the relationships between extreme obesity, quality of life, and sexual function. Obes Surg. 2012;22(4):668–76. https://doi.org/10.1007/s11695-012-0588-1.
Kolotkin RL, Davidson LE, Crosby RD, et al. Six-year changes in health-related quality of life in gastric bypass patients versus obese comparison groups. Surg Obes Relat Dis. 2012;8(5):625–33. https://doi.org/10.1016/j.soard.2012.01.011.
Karlsson J, Taft C, Rydén A, et al. Ten-year trends in health-related quality of life after surgical and conventional treatment for severe obesity: the SOS intervention study. Int J Obes. 2007;31(8):1248–61. https://doi.org/10.1038/sj.ijo.0803573.
Moore RH, Sarwer DB, Lavenberg J, et al. Relationship between sexual function and quality of life in persons seeking weight reduction. Obesity. 2013;21(10):1966–74. https://doi.org/10.1002/oby.20398.
Sarwer DB, Spitzer JC, Wadden TA, et al. Sexual functioning and sex hormones in persons with extreme obesity and seeking surgical and non-surgical weight loss. Surg Obes Relat Dis. 2013;9(6):997–1007. https://doi.org/10.1016/j.soard.2013.07.003.
Sarwer DB, Spitzer JC, Wadden TA, et al. Changes in sexual functioning and sex hormone levels in women following bariatric surgery. JAMA Surg. 2014;149(1):26–33. https://doi.org/10.1001/jamasurg.2013.5022.
Leenen R, van der Kooy K, Seidell JC, et al. Visceral fat accumulation in relation to sex hormones in obese men and women undergoing weight loss therapy. J Clin Endocrinol Metab. 1994;78(6):1515–20. https://doi.org/10.1210/jcem.78.6.8200956.
Legro RS, Dodson WC, Gnatuk CL, et al. Effects of gastric bypass surgery on female reproductive function. J Clin Endocrinol Metab. 2013;97(12):4540–8.
Turcato E, Zamboni M, De Pergola G, et al. Interrelationships between weight loss, body fat distribution and sex hormones in pre- and postmenopausal obese women. J Intern Med. 1997;241(5):363–72. https://doi.org/10.1046/j.1365-2796.1997.120129000.x.
Bastounis EA, Karayiannakis AJ, Syrigos K, et al. Sex hormone changes in morbidly obese patients after vertical banded gastroplasty. Eur Surg Res. 1998;30(1):43–7. https://doi.org/10.1159/000008556.
Belle SH, Berk PD, Courcoulas AP, et al. Safety and efficacy of bariatric surgery: Longitudinal Assessment of Bariatric Surgery. Surg Obes Relat Dis. 2007;3(2):116–26. https://doi.org/10.1016/j.soard.2007.01.006.
Belle SH, Berk PD, Chapman WH, et al. Baseline characteristics of participants in the Longitudinal Assessment of Bariatric Surgery-2 (LABS-2) study. Surg Obes Relat Dis.[published online ahead of print March 7, 2013]. https://doi.org/10.1016/j.soard.2013.01.023.
Longitudinal Assessment of Bariatric Surgery (LABS) Consortium, Flum DR, Belle SH, et al. Perioperative safety in the longitudinal assessment of bariatric surgery. NEJM. 2009;361(5):445–54.
Sarwer DB, Spitzer JC, Wadden TA, et al. Sexual functioning and sex hormones in men who underwent bariatric surgery. Surg Obes Relat Dis. 2014;11(3):643–51. https://doi.org/10.1016/j.soard.2014.12.014.
Rosen R, Brown C, Heiman J, et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26(2):191–208. https://doi.org/10.1080/009262300278597.
Wiegel M, Meston C, Rosen R. The female sexual function index (FSFI): cross-validation and development of clinical cutoff scores. J Sex Marital Ther. 2005;31(1):1–33. https://doi.org/10.1080/00926230590475206.
Ware JE, Snow KK, Kosinski M, et al. SF-36 health survey manual and interpretation guide. Boston: New England Medical Center, The Health Institute; 1993.
Kolotkin RL, Head S, Hamilton M, et al. Assessing the impact of weight on the quality of life. Obes Res. 1995;3(1):49–56. https://doi.org/10.1002/j.1550-8528.1995.tb00120.x.
Kolotkin RL, Crosby RD, Kosloski KD, et al. Development of a brief measure to assess quality of life in obesity. Obes Res. 2001;9(2):102–11. https://doi.org/10.1038/oby.2001.13.
Kolotkin RL, Crosby RD. Manual for the Impact of Weight on Quality of Life Measure (IWQOL and IWQOL-Lite). Durham: Obesity and Quality of Life Consulting; 2011.
Cash TF, Fleming EC. The impact of body-image experiences: development of the Body Image Quality of Life Inventory. Int J Eat Disord. 2002;31(4):455–60. https://doi.org/10.1002/eat.10033.
Cooper PJ, Taylor MJ, Cooper Z, et al. The development and validation of the body shape questionnaire. Int J Eat Disord. 1987;6(4):485–94. https://doi.org/10.1002/1098-108X(198707)6:4<485::AID-EAT2260060405>3.0.CO;2-O.
Spanier GB. Measuring dyadic adjustment: new scales for assessing the quality of marriage and similar dyads. J Marital Fam Ther. 1976;38(2):15–38.
Beck AT, Steer RA, Brown GK. Beck depression inventory II (BDI-II) manual. San Antonio: Harcourt Brace; 1993.
Herpertz S, Kielmann R, Wolf AM, et al. Do psychosocial variables predict weight loss or mental health after obesity surgery? A systematic review. Obes Res. 2004 Oct;12(10):1554–69. https://doi.org/10.1038/oby.2004.195.
van Hout GC, Boekestein P, Fortuin FA, et al. Psychosocial functioning following bariatric surgery. Obes Surg. 2006 Jun;16(6):787–94. https://doi.org/10.1381/096089206777346808.
Funding
This ancillary study to the Longitudinal Assessment of Bariatric Surgery-2 was funded by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) grant no. R01DK072452.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
During the time of the study, Dr. Sarwer served as a paid consultant for Allergan, BariMD, BAROnova, EnteroMedics, and Ethicon Endo-Surgery, which are manufacturers of products for non-surgical weight loss treatment and bariatric surgery. At the time of the conduct of the study, he also was on the board of directors of the Surgical Review Corporation, which created the International Center of Excellence for Bariatric Surgery program to evaluate bariatric surgeons and hospitals around the world. Dr. Wadden serves on advisory boards for Novo Nordisk, Nutrisystem, and Orexigen Pharmaceuticals. Dr. Courcoulas has received research grants from Allergan, Pfizer, Covidien, EndoGastric Solutions, and Nutrisystem and is on the Scientific Advisory Board of Ethicon J & J Healthcare System. Dr. Mitchell, Ms. Spitzer, Ms. Lancaster, Mr. Gourash, and Dr. Christian have no relationships to disclose.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Electronic Supplementary Material
ESM 1
(DOCX 23 kb).
Rights and permissions
About this article
Cite this article
Sarwer, D.B., Wadden, T.A., Spitzer, J.C. et al. 4-Year Changes in Sex Hormones, Sexual Functioning, and Psychosocial Status in Women Who Underwent Bariatric Surgery. OBES SURG 28, 892–899 (2018). https://doi.org/10.1007/s11695-017-3025-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-3025-7