Abstract
Background
The long-limb Roux-en-Y gastric bypass (LLRYGB) was introduced in 1987 as a salvage operation for inadequate weight loss after a standard Roux-en-Y gastric bypass (RYGB).
Methods
We report on 53 consecutive patients (44 females) with conversion of a failed RYGB to a LLRYGB performed by a single surgeon between 2002 and 2014. No patient had an ascertainable anatomic abnormality to explain his/her weight regain. LLRYGB revision consisted of a 75-cm to 100-cm alimentary Roux limb and a 75-cm to 100-cm common channel; after 2011, in suitable patients, the Roux limb was lengthened to greater than 250 cm.
Results
Average values for weight (lbs) were as follows: pre-original RYGB = 329; lowest measured after RYGB = 196; at time of LLRYGB = 285; and at 1, 2, 3, 4, >5 years post LLRYGB = 225, 207, 199, 197, 195, for a sustained weight loss >90 lbs. Average values for BMI (kg/m2) were as follows: pre-original RYGB = 54.3; lowest measured after RYGB = 32.3; at time of LLRYGB = 47.2; and at 1, 2, 3, 4, >5 years post LLRYGB = 37.1, 34.4, 33.0, 32.8, 31.4, for a sustained BMI reduction >16.5 kg/m2. Zero operative mortality; 3 (5.7%) late deaths; 7 (13.2%) 30-day complications; 33 (62.3%) long-term complications with 23 (43.4%) needing TPN; and 14 (26.4%) requiring operative revision.
Conclusion
A salvage LLRYGB procedure can be performed safely and is weight successful, but fraught with long-term nutritional problems and a high necessity for revision. A Roux segment over 250 cm may improve outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Torres and Oca in 1987 introduced a long-limb Roux-en-Y gastric bypass (LLRYGB) as a secondary salvage procedure for an inadequate weight response following a standard Roux-en-Y gastric bypass (RYGB) [1]. The LLRYGB was employed by Brolin et al. in 1992 as a primary operation for the super obese [2].
It has long been demonstrated that between 20 to 40% of primary RYGB obese and super obese patients fail to achieve a satisfactory long-term weight response with no demonstrable evidence of an anatomic cause (e.g., fistula) [3–6]. The bariatric surgeon is obligated to provide revisional surgery as part of the remedial care of patients who have failed the weight loss objective of a first operative attempt [7]. It is imperative, therefore, that we continuously and objectively analyze the outcomes for the revisional surgery being carried out. We herein report on 53 consecutive patients with conversion of a RYGB to a LLRYGB performed by a single surgeon between 2002 and 2014.
Methods
The 53 patients in this series all had their revision to a LLRYGB performed by the same surgeon (HB). The operative objective of the original RYGB surgeon was to construct the traditional 30 ml upper gastric pouch with a 1-cm gastrojejunostomy anastomosis to a retrocolic, 75-cm-long jejunal Roux limb; the length of the biliopancreatic limb was not recorded. All anastomoses were performed open with a linear stapler and over sewn with interrupted 5/0 Tevdek® stutures [8].
Pre-revision to a LLRYGB, the patients all underwent nutritional assessment and counseling, and psychiatric appraisal if deemed necessary. The pre-reoperative evaluation included both endoscopy and an upper gastrointestinal X-ray series. None of the 53 patients had a gastrogastric or gastrointestinal fistula or other ascertainable anatomic abnormality. The size of the upper gastric pouches and gastrojejunal outlets varied, but many were within the size originally intended. Only one patient failed to have an acceptable weight loss after her original operation; the other 52 patients had an adequate weight response originally but regained an inordinate amount of weight subsequently. In association with their regaining of weight, several patients experienced a return of their preoperative bariatric comorbidities.
The revisions to a LLRYGB were all performed by open surgery. The procedure until 2011 consisted of division of the alimentary Roux limb just proximal to the anastomosis of the Roux to the biliopancreatic limb and a single anastomosis reconstruction of bowel continuity of the Roux limb to the ileum, 75 cm to 100 cm proximal to the ileocecal valve; closure of mesenteric defects was routine [9]. Starting in 2011, the Roux segment was lengthened to over 250 cm, if it was anatomically safe to do so. This procedure consisted of resection of the jejunojunostomy Roux to biliopancreatic limb trifurcation and performing both a jejunojunostomy to lengthen the Roux and a jejunoileostomy of the biliopancreatic limb to the terminal ileum. This change in technique was prompted by Scopinaro’s work on protein absorption following biliopancreatic diversion [10]. Figure 1 presents schematics for the two revision procedures.
Patient follow-up assessments after LLRYGB revision included changes in weight in pounds (lbs) and in body mass index (BMI in kg/m2), up to 5+ years postoperatively; 30-day mortality and readmissions; and long-term mortality and adverse effects.
Results
Incidence of Revision to LLRYGB
This series of 53 revisions to a LLRYGB was performed from 2001 to 2014. During that time interval, our bariatric surgery center performed 5185 bariatric procedures, of which 2848 were primary RYGB procedures.
Weight Loss after LLRYGB
Table 1 provides the series patients’ sex, height (inches), pre-RYGB weight (lbs, kg), date of RYGB, lowest post-RYGB weight, ages, weight and BMI (kg/m2) at time of revision to LRYGB, date of LLRYGB, and post-revision weights and BMI for up to 5 years as available. Of the 53 patients, 44 were female (83%). The average duration between the original RYGB and the LLRYGB revision was 10.8 (range 2 to 30) years.
Table 2 provides the averages and ranges for weight (lbs) and BMI (kg/m2), and the number of subjects available for evaluation, at the following time points: prior to the original RYGB, lowest measured after RYGB, at time of LLRYGB, and at follow-up intervals of 1 to >5 years post LLRYGB. Over time after the salvage LLRYGB, the average weight and the average BMI continued to decrease.
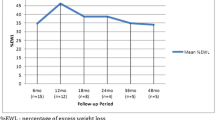
Table 3 provides the average weight loss (lbs) and change in BMI (kg/m2), and the number of subjects available for evaluation, for >5 years following LLRYGB. In spite of the diminishing sample size over time, it is evident that for >5 years after LLRYGB, there is a sustained weight loss over 90 lbs and a lowering of the BMI of 16.5 kg/m2 (33.5%). The BMI response to LLRYGB is plotted in Fig. 2.
Perioperative Complications and 30-day Readmissions
There were no perioperative or under 30-day deaths in this series. One patient was returned to the operating room for control of intraperitoneal hemorrhage.
Seven patients (13.2%) were readmitted within 30 days of their LLRYGB with readily manageable complications. These adverse events are enumerated, with the index number of the patient in whom they occurred, in Table 4.
Long-Term Mortality and Complications
There were 3 (5.7%) long-term deaths in this series. One woman (index #21) died of sepsis with multiple infections and respiratory failure 8 years after her LLRYGB and 7 years after takedown of her LLRYGB with restoration of her original RYGB anatomy. One woman (index #35) died of malnutrition 2 years after LLRYGB after she and her physicians refused takedown of her LLRYGB. One man (index #45) died of endocarditis with an infected aortic valve and severe aortic insufficiency 1 year after his LLRYGB.
There were 33 (62.3%) patients with long-term significant abnormalities in this series, which are outlined, together with the patient’s index number, in Table 5. Twenty-three (43.4%) of these patients received total parenteral nutrition (TPN) on one or more occasions.
>250-cm Alimentary Roux Limb Patients
There were 6 patients in the series (index numbers 46, 47, 49, 50, 51, 52) who had the >250-cm alimentary Roux limb. None of them had under 30-day readmissions, significant long-term surgical complications, or evidence of malnutrition.
LLRYGB Revisions
Twelve patients (22.6%) had their LLRYGB revised with construction of a longer common channel, and 2 (3.8%) patients had total takedown of the LLRYGB with restoration of bowel continuity to the original RYGB anatomy (Table 5). The average time from the LLRYGB to the revisional procedure or takedown was 3.2 years.
Discussion
This 53-patient series, with follow-up extending for greater than 5 years in 26% of the patients, of revisions of a RYGB to a long biliopancreatic limb RYGB (LLRYGB) for inadequate weight loss, demonstrates that this procedure can be performed with operative safety and good weight-loss outcomes, exemplified by a 33.5% lowering of the BMI. The procedure, however, is associated with an inordinate number of nutritional complications requiring revisional surgery on failure of conservative therapy in 14 (26.4%) patients, with lengthening of the common channel (n = 12) or restoration to the original RYGB anatomy (n = 2). The data would seem to indicate that lengthening the Roux limb to >250 cm may significantly relieve protein malnutrition without an over compensatory decrease in the desired weight response.
It is now nearly 50 years since the advent of the loop gastric bypass by Mason and Ito [11], and about 40 years since its modification to the RYGB by Griffen et al. [12]. The RYGB is the procedure that has been most frequently performed worldwide since the beginnings of metabolic/bariatric surgery. It is, therefore, not surprising that over time there are more and more RYGB patients who exhibit a regaining of weight and obesity comorbidities. With the introduction of the LLRYGB 29 years ago as a salvage procedure for a failed RYGB [1], there have been several, albeit not many, reports of outcomes following LLRYGB.
It is essential that two distinctions are made in analyzing the LLRYGB literature: (1) if the LLRYGB is employed as a primary or as a salvage procedure and (2) if the long limb of the operation is the alimentary Roux limb or the biliopancreatic limb. A short common channel, 50 to 150 cm in length, between the ileocecal valve and the anastomosis of the distal alimentary Roux limb to the distal biliopancreatic limb completes both variations. The majority of reports are of LLRYGB as a primary procedure with a long alimentary Roux limb; some of these primary procedures utilize both a measured long alimentary Roux limb and a long biliopancreatic limb. The far fewer literature reports of LLRYGB as a secondary, salvage procedure, as a rule, employ a long biliopancreatic limb and a relatively short Roux limb.
The original primary procedure series by Brolin consisted of 45 super obese patients, with a mean follow-up of 43 ± 17 months, in whom two variations of the RYGB were performed: a standard RYGB with a 75-cm alimentary Roux limb (n = 22) and a LLRYGB with a 150-cm alimentary Roux limb (n = 23) [2]. Though the Roux extension was minimal, the authors reported improved weight loss in comparison to the standard RYGB (BMI 35 ± 5 kg/m2 vs. BMI 45 ± 13 kg/m2, p < 0.001) at 24 months, with no differences in metabolic sequelae or diarrhea.
In 1998, Murr et al. compared a Scopinaro biliopancreatic diversion (n = 11) to what they termed a very, very LLRYGB (n = 19) in super obese patients [13]. Their biliopancreatic diversion consisted of a 200-cm alimentary Roux limb and a 50-cm common channel. Their own procedure consisted of a 300–400-cm alimentary Roux limb with a 100-cm common channel. The weight loss following their procedure was not equal to that of the biliopancreatic diversion: BMI 37 ± 2 kg/m2 for the biliopancreatic diversion vs. 42.2 kg/m2 for the very, very long RYGB at 4 years, with essentially no differences in adverse effects.
The same institution published a follow-up report in 2006 of their very, very LLRYGB performed in 257 consecutive patients; 188 (74%) participated in a postoperative survey [14]. Though the authors still recommended the procedure for select individuals, their outcomes tempered their previous enthusiasm. Weight loss was excellent with a BMI at follow-up of 37 ± 9 kg/m2; however, operative mortality was 1%, side effects were significant, and nine patients (4%) required revision of the procedure with proximal relocation of the Roux enteroenterostomy, essentially lengthening the common channel.
In the years following the 1992 Brolin et al.’s report, others experimented using a LLRYGB as a primary bariatric procedure. MacLean et al., in 2001, reported on 242 patients, followed for a mean of 5.5 years, in whom they compared a standard RYGB with a LLRYGB [5]. Their standard RYGB, performed in 96 morbidly obese and 66 super obese patients, consisted of a 40-cm alimentary Roux limb and a 10-cm biliopancreatic limb beyond the Ligament of Treitz; their LLRYGB, performed in 50 morbidly obese and 30 super obese patients, consisted of a 100-cm alimentary Roux limb and a 100-cm biliopancreatic limb. The authors concluded that the morbidly obese patients did not benefit from a LLRYGB (final BMI 28.6 ± 4.7 kg/m2 for the RYGB and 28.5 ± 3.8 kg/m2 for the LLRYGB), however, that the super obese patients did benefit (final BMI 35.8 ± 6.7 kg/m2 for the RYGB and 32.7 ± 5.1 kg/m2 for the LLRYGB).
In 2002, Brolin et al. published a follow-up report on their original operative procedure of a RYGB with a 50–75-cm alimentary Roux limb (n = 99) or a RYGB with a 150-cm Roux (n = 152), and added a comparison to a true LLRYGB with a 75-cm common channel (n = 47), established by anastomosis of a short biliopancreatic limb to the remainder of the small intestine as the Roux limb [15]. Weight loss was directly proportional to Roux limb length or reversely proportional to the length of the common channel. Malnutrition complications and the need for revision (n = 2) occurred in the LLRYGB group.
In 2006, Christou et al. published an over 10-year follow-up of their patients who had received a LLRYGB (n = 83) and compared them to their patients with a standard RYGB (n = 189) [6]. Their short limb RYGB consisted of a 40-cm alimentary Roux limb with a 10-cm biliopancreatic limb beyond the Ligament of Treitz; the LLRYGB consisted of a 100-cm Roux limb and 100-cm biliopancreatic limb. There was a significant regain of weight in both groups 5 years after surgery, and by 10+ years, there was no difference in results between the RYGB and LLRYGB groups. The overall failure rate for >10 years was 20.4% for the morbidly obese and 34.9% for the super obese.
Emphasizing the effect on the obesity comorbidities, Pinheiro et al., in 2008, in 105 randomized patients, demonstrated a statistically significant difference in the impact on type 2 diabetes and hyperlipidemia between a gastric bypass with a Roux limb of 150 cm and a biliopancreatic limb of 50 cm and a gastric bypass with a Roux limb of 250 cm and a biliopancreatic limb of 100 cm [16]. Type 2 diabetes was controlled in 58% of the patients with the shorter limbs and in 93% of the patients with the longer limbs (p < 0.05); comparable limb length percentages for lipid disorder improvement were 57 and 70% (p < 0.05). However, at 48 months, the excess weight loss was similar (70 and 74%).
Probably the longest follow-up of LLRYGB patients was provided by Kellum et al. in 2011 [17]. They compared in a 20–25-year follow-up report, super obese patients with a gastroenterostomy performed 250 cm proximal to the ileocecal junction and common channels of 50–150 cm (n = 49), their so-named distal RYGB (D-RYGB), to super obese patients with a 150-cm alimentary Roux limb and a 75-cm biliopancreatic limb (n = 92). In their D-RYGB group, there was one perioperative death and eight deaths 6 to 19 years after surgery. Limb-lengthening revisions were required after failure of conservative therapy for protein malnutrition in 21 patients (42.7%). The authors advised against the D-RYGB as a primary bariatric operation.
In 2011, Kalfarentzos et al. commented on their 960 patients with 3 different LLRYGB procedures with generally satisfactory results [18]. They found that complications and long-term mortality were inversely correlated with the residual functioning bowel (alimentary Roux limb plus common channel).
Finally, in comparing relative bowel length for primary LLRYGBs, the article by Nergaard deserves attention [19]. These authors compared 2 different LLRYGB procedures in a randomized study of 187 consecutive patients with a 5-year follow-up interval. The group with a 200-cm biliopancreatic limb and a 60-cm alimentary Roux limb (n = 93) in comparison to a group with a 60-cm biliopancreatic limb and a 150-cm Roux limb (n = 94) had a greater weight loss, exhibited increased vitamin and mineral deficiencies, and had more frequent stools. The authors’ rate of significant complications, including protein malabsorption, was similar between groups.
Turning from employment of an LLRYGB as a primary procedure to its use as a salvage operation for failure of adequate weight loss after a prior RYGB, the report by Torres and Oca [1] was followed by that of Fox et al. in 1996 [20]. These authors described their remedial operation as consisting of a 250-cm length of small intestine from the upper gastric pouch to the ileocecal junction, containing a 100-cm common channel constructed by anastomosis of the biliopancreatic limb to the alimentary Roux limb. Their follow-up data are replete with early and late complications accompanying the excellent weight response achieved (mean excess weight loss 83, 89, and 94% at 1, 2, and 3 years, respectively).
The next major report of a LLRYGB as a salvage procedure is that of Sugerman et al. in 1997 [21]. Their paper analyzed outcomes of a LLRYGB after a failed RYGB in 27 formerly super obese individuals followed for 5 years. Their LLRYGB consisted of a 200-cm alimentary Roux limb and a 50-cm common channel for their first five patients, and a 100-cm Roux and a 150-cm common channel thereafter (n = 22). All of their first five patients with the ultrashort common channel had severe malnutrition and required revision, and two died of hepatic failure. Three of the subsequent 22 patients with a longer common channel also required revisional bowel lengthening for malnutrition. Weight loss was uniformly satisfactory with a reduction from the average BMI pre-LLRYGB of 46 ± 2 to 37 ± 2 kg/m2 at 1 year and 32 ± 2 kg/m2 at 5 years.
In 2001, Fobi et al. published a retrospective chart review of 65 patients who had undergone a LLRYGB salvage operation [22]. Their LLRYGB consisted of transecting the alimentary Roux limb just proximal to the jejunojejunostomy site and moving this segment to a point half the length of the original common channel, effectively reducing the common channel by 50%. Again, weight loss was adequate: BMI 41.87 kg/m2 at time of LLRYGB and 34.60 kg/m2 >1 year thereafter. Fifteen (23.1%) patients developed protein malnutrition and six (9.2%) required revisional surgery back to a standard RYGB.
In 2011, the 1996 authors published their >10 years follow-up [23]. Many of their revisions were not, however, for a failed RYGB but rather for failed gastroplasties and bands. The average reduction in the BMI was maintained; 41.4 ± 8 kg/m2 at the time of the LLRYGB and 28 ± 4 kg/m2 at 10-year follow-up. They reported no deaths, no leaks, and no protein malabsorption.
The parameters we chose to employ for our LLRYGB were based on the following reasoning: These patients had all regained significant amounts of weight after a standard RYGB with a relatively small upper gastric pouch and a 75-cm to 100-cm alimentary Roux limb. Further gastric pouch surgery, therefore, was not entertained. We elected to decrease the length of the small intestinal absorptive surface by leaving a long biliopancreatic limb, which serves only as the conduit for bile and gastric and pancreatic digestive enzymes. Thus, the major factor in determining digestion/absorption would be the length of the common channel that we measured at 75 to 100 cm, comparable to the parameters employed by others [21–23]. We also wished to perform the simplest and safest operation. We chose, therefore, transection of the existing alimentary Roux limb just proximal to the jejunojunostomy, and distal, single anastomosis, relocation of the Roux limb to establish the short common channel. Adding length to the alimentary Roux, to a minimum of 250 cm, a procedure requiring resection of the original jejunojunostomy trifurcation and two anastomoses, may be warranted in mitigating malabsorption and limiting the necessity for revisions, while yet maintaining a satisfactory and lasting weight response. It was considered not to be safe to achieve the same result by transecting the distal biliopancreatic limb just proximal to the jejunojunostomy and, thereby, retaining a short piece of the distal biliopancreatic limb, with a limited vascular pedicle, as part of the newly lengthened Roux limb.
Conclusions
LLRYGB as a salvage procedure for a failed RYGB can be performed with operative safety with minimal <30-day complications and excellent remedial weight loss. The trade-off in long-term, primarily malabsorptive, complications, however, is high with 43.4% of patients needing TPN and 26.4% requiring revision to a longer common channel or restoration of bowel continuity to the original RYGB. A more judicious balance of an effective weight response and malabsorptive complications may be obtainable by lengthening the alimentary Roux limb to >250 cm.
References
Torres J, Oca C. Gastric bypass lesser curvature with distal Roux-en-Y. Bariatric Surg. 1987;5:10–5.
Brolin RE, Kenler HA, Gorman JH. Long-limb gastric bypass in the superobese. A prospective randomized study. Ann Surg. 1992;215(4):387–95.
Sugerman HJ, Kellum JM, Engle KM, et al. Gastric bypass for treating severe obesity. Am J Clin Nutr. 1992;55:560S–6S.
Pories WJ, Macdonald Jr KG, Morgan EJ, et al. Surgical treatment of obesity and its effect on diabetes: 10-yr follow-up. Am J Clin Nutr. 1992;55:582S–5S.
MacLean LD, Rhode BM, Nohr CW. Long- or short-limb gastric bypass? J Gastrointest Surg. 2001;5(5):525–30.
Christou NV, Look D, MacLean LD. Weight gain after short- and long-limb gastric bypass in patients followed for longer than 10 years. Ann Surg. 2006;244(5):734–40.
Buchwald H. Revisional metabolic/bariatric surgery: a moral obligation. Obes Surg. 2015;25(3):547–9.
Buchwald H. Open Roux-en-Y gastric bypass. In: Buchwald’s atlas of metabolic & bariatric surgical techniques and procedures. New York: Elsevier; 2011. p. 96–111.
Buchwald H. Roux-en-Y gastric bypass revision to a long-limb Roux-en-Y gastric bypass technique. In: Buchwald’s atlas of metabolic and bariatric surgical techniques and procedures. New York: Elsevier; 2011. p. 354–7.
Scopinaro N. Thirty-five years of biliopancreatic diversion: notes on gastrointestinal physiology to complete the published information useful for a better understanding and clinical use of the operations. Obes Surg. 2012;22:427–32.
Mason EE, Ito C. Gastric bypass in obesity. Surg Clin North Am. 1967;47:1345–52.
Griffen WO, Young VL, Stevenson CC. A prospective comparison of gastric and jejunoileal bypass operation for morbid obesity. Ann Surg. 1977;186:500–7.
Murr MM, Balsiger BM, Kennedy FP. Malabsorptive procedures for severe obesity: comparison of pancreaticobiliary bypass and very very long limb Roux-en-Y gastric bypass. J Gastrointest Surg. 1999;3(6):607–12.
Nelson WK, Fatima J, Houghton SG, et al. The malabsorptive very, very long limb Roux-en-Y gastric bypass for super obesity: results in 257 patients. Surgery. 2006;140(4):517–23.
Brolin RE, LaMarca LB, Kenler HA. Malabsorptive gastric bypass in patients with superobesity. J Gastrointest Surg. 2002;6(2):195-205.
Pinheiro JS, Schiavon CA, Pereira PB. Long-limb Roux-en-Y gastric bypass is more efficacious in treatment of type 2 diabetes and lipid disorders in super-obese patients. Surg Obes Relat Dis. 2008;4(4):521–5.
Kellum JM, Chikunguwo SM, Maher JW. Long-term results of malabsorptive distal Roux-en-Y gastric bypass in superobese patients. Surg Obes Relat Dis. 2011;7(2):189–94.
Kalfarentzos F, Skroubis G, Karamanakos S, et al. Biliopancreatic diversion with Roux-en-Y gastric bypass and long limbs: advances in surgical treatment for super-obesity. Obes Surg. 2011;21(12):1849–58.
Nergaard BJ, Leifsson BG, Hedenbro J. Gastric bypass with long alimentary limb or long pancreato-biliary limb—long-term results on weight loss, resolution of co-morbidities and metabolic parameters. Obes Surg. 2014;24(10):1595–602.
Fox SR, Fox KM, Oh KH. The gastric bypass for failed bariatric surgical procedures. Obes Surg. 1996;6(2):145–50.
Sugerman HJ, Kellum JM, DeMaria EJ. Conversion of proximal to distal gastric bypass for failed gastric bypass for superobesity. J Gastrointest Surg. 1997;1(6):517–25.
Fobi MA, Lee H, Igwe D, et al. Revision of failed gastric bypass to distal Roux-en-Y gastric bypass: a review of 65 cases. Obes Surg. 2001;11(2):190–5.
Srikanth MS, Oh KH, Fox SR. Revision to malabsorptive Roux-en-Y gastric bypass (MRNYGBP) provides long-term (10 years) durable weight loss in patients with failed anatomically intact gastric restrictive operations: long-term effectiveness of a malabsorptive Roux-en-Y gastric bypass in salvaging patients with poor weight loss or complications following gastroplasty and adjustable gastric bands. Obes Surg. 2011;21(7):825–31.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All ethical standards for a retrospective analysis were met: all patient identifiers are known only to the authors and are maintained in a secure file; no patient identity is revealed.
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
No informed consent was required for this retrospective analysis. Appropriate operative consent was obtained for each patient prior to surgery.
Rights and permissions
About this article
Cite this article
Buchwald, H., Oien, D.M. Revision Roux-en-Y Gastric Bypass to Biliopancreatic Long-Limb Gastric Bypass for Inadequate Weight Response: Case Series and Analysis. OBES SURG 27, 2293–2302 (2017). https://doi.org/10.1007/s11695-017-2658-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2658-x