Abstract
Background
Most patients do not meet the recommended level of physical activity after bariatric surgery, and psychological factors underlying postoperative physical activity remain poorly understood. This study aimed at identifying self-regulatory predictors of physical activity after bariatric surgery.
Methods
Questionnaire data including self-regulation variables and the short-version of the International Physical Activity Questionnaire were obtained in a prospective cohort of 230 patients 1 year after Roux-en-Y gastric bypass. The study sample consisted of participants consenting to wear an ActiGraph GT3X+ accelerometer for seven consecutive days, 18–24 months after surgery (n = 120).
Results
A total of 112 participants with complete self-report data provided valid accelerometer data. Mean age was 46.8 years (SD = 9.3), and 81.3% was women. Preoperative and postoperative BMI was 44.8 ± 5.5 and 30.6 ± 5.0 kg/m2, respectively. Total weight loss was 28.9% (SD = 7.5). By objective measures, 17.9% of the participants met the recommended level of moderate-to-vigorous-intensity of physical activity of ≥150 min/week, whereas 80.2% met the recommended level according to self-reported measures. Being single, higher education level, and greater self-regulation predicted objective physical activity in multivariate regression analysis. Greater self-regulation also predicted self-reported physical activity. Weight loss 1 year after surgery was not associated with self-reported or objectively measured physical activity.
Conclusions
Despite large differences between accelerometer-based and subjective estimates of physical activity, the associations of self-regulatory factors and weight loss with postoperative physical activity did not vary depending on mode of measurement. Self-regulation predicted both objective and self-reported physical activity. Targeting patients’ self-regulatory ability may enhance physical activity after gastric bypass.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Regular physical activity is recommend to improve weight loss maintenance and health outcomes after bariatric surgery [1, 2]. Norwegian national guidelines recommend physical activity (PA) of moderate intensity for a minimum of 150 min/week or vigorous intensity for a minimum of 75 min/week performed in bouts of at least 10 min [3], coinciding with public health guidelines in the UK and USA [4, 5]. Recent studies have shown that the majority of patients do not meet the recommended level of PA postoperatively [6]. Indeed, most patients make modest postoperative changes to their preoperative PA levels at best [7–9]. Some even decrease their activity levels [8]. It has been suggested that psychological factors are important for long-term weight management through affecting the patients’ ability to adjust their behavior postoperatively [10]. However, factors underlying postoperative PA remain poorly understood [11], and whether associations of psychological factors and weight loss with PA differ by mode of measurement has, to our knowledge, not been described in bariatric populations. Identifying predictors of postoperative PA could contribute to the development of more effective interventions for enhanced activity levels after surgery.
Self-regulation is essential for adopting new or maintaining health behaviors. This process depends on changes in a set of interrelated underlying cognitions such as intention, planning, and self-efficacy [12]. Intention comprises the motivation to perform a behavior [13] and has been identified as the dominant predictor of PA [14, 15]. Intention has been associated with more frequent and higher levels of PA after bariatric surgery [16]. Planning has been recognized as mediator of the relationship between intention and PA in several studies [17–19]. Planning refers to a person’s mental strategies for how to perform a future behavior (action planning) and how to anticipate potential barriers (coping planning) [20]. More planning preoperatively has been associated with higher PA levels among bariatric patients after surgery [21].
Self-efficacy reflects a person’s confidence in their ability to perform a certain behavior [22]. Higher self-efficacy has been related to higher levels of self-reported PA [21, 23]. Moreover, individual differences in action control, for example, keeping one’s goals in mind, monitoring one’s progress toward these goals, and exerting effort to reduce any discrepancies between current and intended behavior, play an essential role facilitating maintenance of behavior and to prevent relapses to previous behavior [24–26]. Monitoring exercise daily has been associated with increased PA postoperatively [8]. However, to our knowledge, no studies have examined action control in relation to PA after bariatric surgery. Based on the previous, the present study aimed at identifying self-regulatory predictors of physical activity after bariatric surgery.
Methods
Participants and Study Design
Patients eligible for surgery were 18–60 years with a body mass index (BMI) ≥40 or ≥35 kg/m2, combined with obesity-related comorbidity, and failed previous attempts of sustained weight loss. Questionnaire data were retrieved from the Oslo Bariatric Surgery Study, a prospective cohort study of patients recruited from Oslo University Hospital from 2011 to 2013. Details regarding the recruitment process are previously described [21]. Participants that underwent gastric bypass with questionnaire data (including IPAQ-SF) before and 1 year after surgery (N = 230) were asked to wear an ActiGraph GT3X+ accelerometer for seven consecutive days, 18–24 months after surgery. A subsample of 120 (52.2%) patients consented to use the monitor.
Measures
Objective Physical Activity
The ActiGraph GT3X+ activity monitor (Actigraph, LLC, Pensacola, FL, USA) was used to assess levels of PA. The participants were instructed to wear the accelerometers on their right hip during all waking hours for seven consecutive days, except during showering and bathing. Participants had to have more than 10 h of valid data per day for at least 4 days to be included in the analyses. The accelerometer data was used to assess PA levels with regard to mean counts per minute (cpm), sedentary time and minutes of intensity-specific PA, steps taken per day, and percentage of the study population that met the current national PA recommendations. Low, moderate, and vigorous intensity activity were defined as activity in the cpm range of 100–2019, 2020–5998, and 5999 and above, respectively [27, 28]. Adherence to PA recommendations was determined by summing the time spent performing moderate-to-vigorous physical activity in continuous bouts lasting at least 10 min (with allowance for two interruptions) (bout-related moderate-to-vigorous physical activity (MVPA)). If the amount of bout-related MVPA was 150 min or more per week, the participant achieved the recommended level of PA.
Self-Report Physical Activity
The short version of the International Physical Activity Questionnaire (IPAQ-SF) [29] was used to obtain self-reported PA. IPAQ-SF captures time spent in various levels of activity, and mean scores are estimated by weighting type of activity (walking, moderate, and vigorous) by energy requirements reported as metabolic equivalent values per week (MET-min/week). Moderate walking is defined as 3.3 METs, and moderate intensity is commonly defined as 3–5.9 METs [30]. Thus, to capture all activity of moderate and vigorous intensity, a continuous measure of total MET-min/day was used as a measure of self-reported moderate to vigorous PA. Data cleaning and processing was done according to the IPAQ-SF scoring protocol [31]. The recommended level of PA according to the Norwegian national guidelines [3] is 600 MET-min/week based on the IPAQ-SF scoring protocol [31].
Independent Variables
Weight was measured on the day of surgery and 1 year after, using a calibrated Seca 635 III (0–300 kg) platform scale with patients wearing light clothing and no shoes. Postoperative weight loss was used as independent variable to examine whether greater weight loss 1 year after surgery would contribute to higher levels of subsequent PA.
The independent variables are described in Table 1.
The study protocol was approved by the Regional Ethics Committee for Medical Research (2012/17028) South-Eastern Norway and the Data Protection Officer at Oslo University Hospital. Informed consent was obtained from all participants included in the study.
Statistical Analysis
To select variables for the multivariate regression analyses, Pearson correlation coefficients were calculated. Because of high correlations between the psychological variables, a principal component analysis was used to examine if a more parsimonious structure could describe the data. Only variables significantly correlated (p < .05) with objective or self-reported PA were included in the hierarchical regression models. Total accumulated MVPA was used as dependent variable in the correlation and regression analyses instead of MVPA in bouts lasting for at least 10 min (bout-related MVPA), because 30% of the participants did not accumulate any bout-related MVPA minutes. Independent t tests and one-way ANOVA were used to compare demographic and psychological variables between groups and between patients in the study sample. Time difference between surgery and IPAQ-SF and monitor data retrieval was not related to any of the study variables and was therefore not included in the analyses.
Results
The final study sample consisted of 112 participants with complete self-report PA data at follow-up and valid accelerometer recordings. The majority of the participants were women (n = 91; 83.1%), most were employed (n = 81; 72.3%), 38 (34.2%) had a college/university degree, and 73 (65.8%) were married/had a partner. Mean height was 170.2 cm (SD = 8.5), and preoperative and postoperative weight was 124.9 kg (SD = 19.5) and 89.0 kg (SD = 17.3), respectively. BMI before and postsurgery were 44.8 kg/m2 (SD = 5.5) and 30.6 kg/m2 (SD = 5.0), respectively. Percent total weight loss was 28.9% (SD = 7.5).
There were no differences with regard to age, BMI, gender, self-reported levels of PA, or percent total weight loss between the study sample and those who declined to wear the accelerometers. However, there were significant differences in the self-regulatory factors between the two groups. Participants using the monitors scored higher on intention (p < .01), self-efficacy (p < .05), action planning (p < .01), and action control (p < .05).
Data describing self-reported and objective measures of PA are listed in Table 2. Regarding objective measures of walking capacity, 19.6% walked less than 5000 steps/day and 13.4% met the commonly recommended level of ≥10.000 steps/day. Adherence to PA guidelines was 80.2% according to subjective measures and 17.9% according to accelerometer data. Differences in demographic, anthropometric, and self-regulation variables depending on whether the participants met the recommended MVPA-level according to objective measures are described in Table 3. Adherence was associated with higher self-efficacy, better action control skills, higher level of education, and being single.
Table 4 presents the correlations between the independent variables and objective and subjective MVPA. Intention, action and coping planning, self-efficacy, and action control were positively correlated with objective MVPA. The correlations were small to medium sized, with the strongest correlation being with action control (r = .34, p < .001). The same variables correlated slightly stronger and positively with self-reported MVPA. A small, negative association between age and self-reported MVPA was found. Weight loss was not associated with PA, but positively correlated with some of the self-regulatory variables.
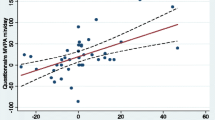
The self-regulation variables were highly inter-correlated (Table 4). A principal component analysis suggested that these motivational and self-regulatory variables would be best described as a single factor. The first component with an Eigenvalue of 10.2 (all factor loadings above 0.35) accounted for 57% of the variance and the next component with an Eigenvalue of 1.4 only accounted for additional 8.1% of the variance. A single component labeled “self-regulation” was therefore extracted, which correlated with objective MVPA (r = .35, p < .001) and self-reported MVPA (r = .38, p < .001).
Two-step hierarchical regression analyses (Table 5) tested the unique contribution of the relevant demographic variables and self-regulation on objective and subjective MVPA. In the first model, being single and higher education level predicted objective MVPA at step 1, accounting for 16.4% of the variance (p < .001). Step 2 tested the effect of self-regulation on MVPA and the explained variance increased to 23.5% (p < .01). In the second model with subjective MVPA as outcome measure, age was entered in step 1 and accounted for 3% of the variance in self-reported MVPA (p < .05). After entering self-regulation at step 2, the explained variance increased to 15% (p < .001). Greater self-regulation emerged as the only significant predictor of self-reported MVPA.
Discussion
The main purpose of this study was to explore levels and predictors of PA after gastric bypass. The accelerometer-based estimates of postoperative PA were considerably lower than subjective estimates and thus confirm the problem of overestimation when using self-report data. The difference in adherence to recommended PA guidelines according to mode of measure, 17.9% (objective measures) versus 80.2% (self-report), has only been reported in two previous bariatric surgery studies with similar large discrepancies, but with smaller study samples [35, 36].
Our findings showed that greater weight reduction did not predict higher levels of neither self-reported nor objective PA, contradicting studies describing associations between weight reduction and improved fitness and exercise performance postsurgical [37, 38]. It may be that extensive weight loss and enhanced physical functioning (e.g., reduction in comorbid conditions or weight-related chronic orthopedic pain) result in a subjective feeling of being more capable of performing different activities, which is not always translated into actual behavior [39].
We observed a strong association between intention, self-efficacy, planning, and action control, as well as higher levels of both objective and self-reported PA. Previous studies have reported associations of intention [16] and planning [21] with self-reported PA, but to our knowledge, the current study is the first to examine associations between self-regulatory factors and objective measures of postsurgical MVPA. The high inter-correlation among the psychological variables indicated that participants with higher intention to be physically active also made more plans, were more self-efficacious, and had better action control skills. This pattern also resembles standard advice provided to patients in preparation for surgery, which prompts motivation, confidence, and self-regulation [40]. The statistical overlap between the psychological variables was confirmed in a principal component analysis showing one underlying factor named self-regulation. In further analyses, self-regulation was identified as an important predictor of both objective and self-reported MVPA. Interventions targeting peoples’ abilities to make plans, how to increase self-efficacy, and improve action control skills have proven to facilitate long-term behavior change in other patient rehabilitation groups [26]. Our findings imply that such interventions may contribute to improved long-term outcomes in bariatric surgery patients.
Self-regulation was the only variable that emerged as predictor of self-reported MVPA, whereas being single was the second variable identified as a positive predictor of objective MVPA when controlling for level of education and self-regulation. To be single or divorced has previously been related to better weight loss outcomes, and it has been suggested that this is because single people are likely to have more time for regular PA [41, 42]. Moreover, partners/spouses influence each other’s behavior [43]. The risk of returning to old habits might be higher if previous unhealthy behavior (e.g., sedentary behavior) is upheld by the partner/spouse.
The final unique predictor of objective MVPA was higher education level. This finding coincides with results from a recent report with objective measures of PA in a population-based sample of Norwegian adults [44] and findings from other population-based studies describing subjective PA [45]. Our results indicate that patients with lower education and those in a relationship may have additional need for support to become more physically active postsurgical.
In accordance with evidence from both population-based studies of PA [45] and postbariatric surgery [8], we found that younger age was associated with higher levels of self-reported MVPA. Further, we found no gender differences in self-reported or objectively measured PA, similar to recent observations both in a bariatric sample [46] and in normal populations using monitor data [27]. King et al. [47], however, found that men were more active than women, which is also commonly reported in studies with self-reported PA [45].
There are limitations to the study. All participants underwent gastric bypass, and the findings may not be generalizable to other bariatric surgical procedures. Furthermore, an accelerometer located on the trunk may underestimate or miss cycling or upper body movements [48]. The differences observed for most of the self-regulatory factors between the study cohort and the non-respondents might represent a selection bias. Study strengths were in particular, applying the ActiGraph GT3X+ accelerometer, a widely used and validated activity monitor. Additionally, only participants with valid accelerometer data (≥4 days of recordings) were included in the study sample, with the majority (85.7%) wearing the monitors for 6 or 7 days.
Conclusions
Despite large differences in accelerometer-based and subjective estimates of activity levels, the associations of self-regulatory factors and weight loss with postoperative MVPA did not vary depending on mode of measurement. Self-regulation predicted both objective and self-reported MVPA, suggesting that improving self-regulation capabilities may enhance activity levels after gastric bypass. The findings of poor adherence to recommended level of physical activity indicate that behavioral adjustment constitutes a great challenge after bariatric surgery.
References
Coen PM, Goodpaster BH. A role for exercise after bariatric surgery? Diabetes Obes Metab. 2016;18(1):16–23. doi:10.1111/dom.12545.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Obesity. 2013;21(S1):S1–S27.
Helsedirektoratet. Anbefalinger om kosthold, ernæring og fysisk aktivitet. In: Helsedirektoratet, editor. Oslo: Andvord Grafisk AS; 2012
O’Donovan G, Blazevich AJ, Boreham C, et al. The ABC of physical activity for health: a consensus statement from the British Association of Sport and Exercise Sciences. J Sports Sci. 2010;28(6):573–91.
Haskell WL, Lee I-M, Pate RR, et al. Physical activity and public health. Updated recommendations for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116.
Reid RE, Carver TE, Andersen KM, et al. Physical activity and sedentary behavior in bariatric patients long-term post-surgery. Obes Surg. 2015;25(6):1073–7. doi:10.1007/s11695-015-1624-8.
Berglind D, Willmer M, Eriksson U, et al. Longitudinal assessment of physical activity in women undergoing Roux-en-Y gastric bypass. Obes Surg. 2015;5(1):119–25. doi:10.1007/s11695-014-1331-x.
King WC, Hsu JY, Belle SH, Courcoulas AP, Eid GM, Flum DR, et al. Pre- to postoperative changes in physical activity: report from the Longitudinal Assessment of Bariatric Surgery-2 (LABS-2). Surg Obes Relat Dis. 2011;8(5):522-532. doi:10.1016/j.soard.2011.07.018.
King WC, Chen JY, Bond DS, et al. Objective assessment of changes in physical activity and sedentary behavior: pre- through 3 years post-bariatric surgery. Obesity. 2015;23(6):1143–50. doi:10.1002/oby.21106.
Wimmelmann CL, Dela F, Mortensen EL. Psychological predictors of weight loss after bariatric surgery: a review of the recent research. Obes Res Clin Pract. 2013;8(4)
Galioto R, Gunstad J, Heinberg LJ, et al. Adherence and weight loss outcomes in bariatric surgery: does cognitive function play a role? 2013;23(10), 1703–1710. doi:10.1007/s11695-013-1060-6
Parschau L, Barz M, Richert J, et al. Physical activity among adults with obesity: testing the health action process approach. Rehabil Psychol. 2014;59(1):42–9.
Fishbein M, Ajzen I. Belief, attitude, intention, and behavior: an introduction to theory and research. Reading: Addison-Wesley; 1975.
Rhodes RE, Bruijn GJ. How big is the physical activity intention–behaviour gap? A meta-analysis using the action control framework. Br J Health Psychol. 2013;18(2):296–309.
Hagger MS, Chatzisarantis NL, Biddle SJ. A meta-analytic review of the theories of reasoned action and planned behavior in physical activity: predictive validity and the contribution of additional variables. J Sport Exerc Psychol. 2002;24(1).
Bond DS, Thomas GJ, Ryder B, et al. Ecological momentary assessment of the relationship between intention and physical activity behavior in bariatric surgery patients. Int J Behav Med. 2011;1–6.
Scholz U, Schüz B, Ziegelmann JP, et al. Beyond behavioural intentions: planning mediates between intentions and physical activity. Br J Health Psychol. 2008;13(3):479–94.
Reuter T, Ziegelmann JP, Wiedemann AU, et al. Changes in intentions, planning, and self-efficacy predict changes in behaviors. J Health Psychol. 2010;15(6):935–47.
Conner M, Sandberg T, Norman P. Using action planning to promote exercise behavior. Ann Behav Med. 2010;40(1):65–76.
Sniehotta FF, Scholz U, Schwarzer R. Action plans and coping plans for physical exercise: a longitudinal intervention study in cardiac rehabilitation. Br J Health Psychol. 2006;11(1):23–37.
Bergh I, Kvalem IL, Risstad H, et al. Preoperative predictors of adherence to dietary and physical activity recommendations and weight loss one year after surgery. Surg Obes Relat Dis. 2016;12(4):910–8. doi:10.1016/j.soard.2015.11.009.
Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215.
Hübner C, Baldofski S, Zenger M, et al. Influences of general self-efficacy and weight bias internalization on physical activity in bariatric surgery candidates. Surg Obes Relat Dis. 2014 (0).
Parschau L, Fleig L, Koring M, et al. Positive experience, self-efficacy, and action control predict physical activity changes: a moderated mediation analysis. Br J Health Psychol. 2013;18(2):395–406.
Sniehotta FF, Nagy G, Scholz U, et al. The role of action control in implementing intentions during the first weeks of behaviour change. Br J Soc Psychol. 2006;45(1):87–106.
Sniehotta FF, Scholz U, Schwarzer R. Bridging the intention–behaviour gap: planning, self-efficacy, and action control in the adoption and maintenance of physical exercise. Psychol Health. 2005;20(2):143–60.
Hansen BH, Kolle E, Dyrstad SM, et al. Accelerometer-determined physical activity in adults and older people. Med Sci Sports Exerc. 2012;44(2):266.
Troiano RP, Berrigan D, Dodd KW, et al. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181.
Craig C, Marshall A, Sjostrom M, et al. International Physical Activity Questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95. doi:10.1249/01.MSS.0000078924.61453.FB.
Ainsworth BE, Haskell WL, Herrmann SD, et al. Compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43(8):1575–81.
IPAQ. Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ). Short and long forms. 2005 [cited 2015 11/19]; Available from: https://sites.google.com/site/theipaq/scoring-protocol.
Brethauer SA, Kim J, el Chaar M, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Obes Surg. 2015;25(4):587–606.
Renner B, Schwarzer R. Risk and health behaviors documentation of the scales of the research project: “risk appraisal consequences in Korea” (RACK). Berlin: International University Bremen & Freie Universität Berlin; 2005.
Sniehotta FF, Schwarzer R, Scholz U, et al. Action planning and coping planning for long-term lifestyle change: theory and assessment. Eur J Soc Psychol. 2005;35(4):565–76.
Bond DS, Jakicic JM, Unick JL, et al. Pre- to postoperative physical activity changes in bariatric surgery patients: self report vs. objective measures. Obesity. 2010;18(12):2395–7.
Berglind D, Willmer M, Tynelius P, et al. Accelerometer-measured versus self-reported physical activity levels and sedentary behavior in women before and 9 months after Roux-en-Y gastric bypass. Obes Surg. 2015:1–8
De Souza SAF, Faintuch J, Sant’Anna AF. Effect of weight loss on aerobic capacity in patients with severe obesity before and after bariatric surgery. Obes Surg. 2010;20(7):871–5.
Wilms B, Ernst B, Thurnheer M, et al. Differential changes in exercise performance after massive weight loss induced by bariatric surgery. Obes Surg. 2012:1–7. English
Josbeno DA, Kalarchian M, Sparto PJ, et al. Physical activity and physical function in individuals post-bariatric surgery. Obes Surg. 2011;21(8):1243–9.
Kvalem IL, Bergh I, Soest T, et al. A comparison of behavioral and psychological characteristics of patients opting for surgical and conservative treatment for morbid obesity. BMC Obesity. 2016;3(1):1–11.
Lutfi R, Torquati A, Sekhar N, et al. Predictors of success after laparoscopic gastric bypass: a multivariate analysis of socioeconomic factors. Surgical Endoscopy And Other Interventional Techniques. 2006;20(6):864–7. English
Livhits M, Mercado C, Yermilov I, et al. Behavioral factors associated with successful weight loss after gastric bypass. Am Surg. 2011;76(10):1139–42.
Homish GG, Leonard KE. Spousal influence on general health behaviors in a community sample. Am J Health Behav. 2008;32(6):754–63.
Hansen BH, Kolle E, Anderssen SA. Fysisk aktivitetsnivå blant voksne og eldre i Norge. Oppdaterte analyser basert på nye nasjonale anbefalinger i 2014. Oslo: Helsedirektoratet, 2014 IS-2183
Bauman A, Bauman R, Reis J, et al. Correlates of physical activity: why are some people physically active and others not? Lancet (London, England). 2012;380(9838):258–71.
Chapman N, Hill K, Taylor S, et al. Patterns of physical activity and sedentary behavior after bariatric surgery: an observational study. Surg Obes Relat Dis. 2014;10(3):524–30.
King WC, Engel SG, Elder KA, et al. Walking capacity of bariatric surgery candidates. Surg Obes Relat Dis. 2012;8(1):48–59. doi:10.1016/j.soard.2011.07.003.
Jørgensen T, Andersen LB, Froberg K, et al. Position statement: testing physical condition in a population—how good are the methods? Eur J Sport Sci. 2009;9(5):257–67.
Acknowledgments
We are grateful for the assistance with the recruitment process from the personnel at the Department of Morbid Obesity and Bariatric Surgery, Oslo University Hospital. We also thank Jon A. Kristinsson for contributions to the development of the study and Marianne Sæter and Thomas Nordvik for assistance with data retrieval.
Author Contributions
ILK, FFS, and IB designed the study. TM, ILK, and IB were involved in the data collection. IB, ILK, and BHH performed the statistical analyses, and IB drafted the manuscript. All authors contributed to the interpretation of the analyses and revisions of the manuscript. All authors have read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study protocol was approved by the Regional Ethics Committee for Medical Research (2012/17028) South-Eastern Norway and the Data Protection Officer at Oslo University Hospital. Informed consent was obtained from all participants included in the study.
Funding
Falko F. Sniehotta is funded by Fuse, the Centre for Translational Research in Public Health, a United Kingdom Clinical Research Collaboration Public Health Research Centre of Excellence based on funding from the British Heart Foundation, Cancer Research United Kingdom, Economic and Social Research Council, Medical Research.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Bergh, I., Kvalem, I.L., Mala, T. et al. Predictors of Physical Activity After Gastric Bypass—a Prospective Study. OBES SURG 27, 2050–2057 (2017). https://doi.org/10.1007/s11695-017-2593-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2593-x