Abstract
Background
Despite reported effectiveness, weight loss surgery (WLS) still remains one of the least preferred options for outpatient providers, especially in Germany. The aim of this study was to examine the effect of stigma and knowledge on recommendation of WLS and referral to a surgeon by general practitioners (GPs) and internists.
Method
The sample consists of 201 GPs and internists from Germany. The questionnaire included questions on the perceived effectiveness of WLS, the frequency of recommendations of WLS, and the frequency of referral to WLS. Stigma, as well as knowledge was also assessed in this context. Linear and logistic regression models were conducted. A mediation analysis was carried out within post hoc analysis.
Results
Knowledge (b = 0.258, p < 0.001) and stigma towards surgery (b = −0.129, p = 0.013) were related to the frequency of recommendation of WLS. Additionally, respondents, who were more likely to express negative attitudes towards WLS, were less likely to recommend WLS and thus refer patients to WLS (b = −0.107, p < 0.05). Furthermore, respondents with more expertise on WLS were more likely to recommend and thus refer patients to WLS (b = 0.026, p < 0.05).
Conclusion
This study showed that stigma plays a role when it comes to defining treatment pathways for patients with obesity. The question remains how this might influence the patients and their decision regarding their treatment selection. Interventions are required to make treatment decisions by physicians or patients independent of social pressure due to stigma.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Outpatient providers play a very important role in terms of counseling or discussion about treatment for obesity. Generally, about 36.6 % of patients who seek help from a general practitioner (GP) for several reasons are overweight and 22.8 % are obese [1]. Especially GPs and internists are often faced with the decision to refer their patients to a specialist, being considered gate keepers in the health care system [2]. Their patients rely on their expertise and their advice when choosing specific treatment pathways [2, 3]. In this context, the discussion about a suitable treatment method such as bariatric surgery, hence recommending it to the patient, provides the basis for later referral to a surgeon.
With regard to treatment options, conservative methods such as dietary changes, increases in physical activity, or pharmacological interventions, for example, are seen most effective and therefore recommended far more often by GPs or health care professionals (HCPs). Besides conservative methods, weight loss surgery (WLS) has developed to be an acknowledged alternative for patients with severe obesity [1, 4–8]. Compared to other countries worldwide, however, the number of bariatric surgeries that are performed in Germany is very low [7]. Apart from financial or economic controversies, WLS still does not seem to be fully accepted. Even if people in the general public perceive WLS as effective, they are also hesitant to recommend this kind of treatment to people with obesity [9]. The same skepticism can be observed in health care professionals, and there seems to be a discrepancy between perceptions of effectiveness and actual recommendation or referral. The discrepancy between perceived success and actual recommendation of WLS is particularly high for GPs (42.3 %) and internists (31.8 %) compared to other professionals, indicating that high perceptions of effectiveness surprisingly do not result in corresponding number of surgeries prescribed [10]. On the contrary, in the USA, where surgery rates are much higher, a study found that 79.6 % of physicians feel positive about bariatric surgery as an option to treat obesity. In terms of recommendation, they would recommend surgery to a patient with obesity (79.4 %) or type 2 diabetes (81.8 %) [11]. However, at the same time, only 64.9 % of the providers were willing to refer a patient with type 2 diabetes and a BMI over 35 kg/m2 as the guidelines would propose [11]. Recommendation and referral behavior of HCPs may therefore be an additional driver for the low rate of patients that actually undergo weight loss surgery, even in the USA [12]. Previous research revealed that certain physician’s characteristics were indeed associated with a willingness to refer patients to WLS [13] and HCPs of different specialty areas show a lack of knowledge of guidelines [9, 10, 14]. A lack of knowledge regarding WLS among physicians, especially among the non-referrers, is clearly recognizable [13]. For instance, about 38 % of physicians believe that weight regain was less than 5 kg only [13]. As a result, knowledge or expertise on WLS still seems to be insufficient, having an effect on referral behavior of general practitioners and internists. This in turn might have an impact on the perception of the general public and patients themselves. Out of the group of patients eligible for surgery, half of the patients would consider WLS as a treatment option if it had been recommended by their physician, but only 20 % stated that they have actually been recommended for WLS by their physician [15]. In addition, when asking physicians whether they would advise a patient who meets criteria for WLS to see a surgeon, only 23.8 % would recommend this [16]. These studies provide evidence for the influence of the physician on the patient’s decision-making, and in turn on low surgery rates.
The physicians’ attitude might therefore play a role when treating patients with obesity. Two thirds of patients report that their primary care physicians “don’t understand how difficult it is to be overweight” and about one third agrees on the statement “doctors don’t believe me when I tell them that I don’t eat that much” [17]. Pejorative attitudes (e.g., stigmatization, among health care professionals towards patients with obesity) seem to be an ubiquitous problem that can be allocated to many domains of health care [18]. Even primary care physicians assign negative stereotypes to patients with obesity [18] and prospective WLS-patients report weight-related stigmatization by their physicians [19]. Stigmatization is often accompanied by the view that patients with obesity or overweight are lazy and lack willpower to lose weight, having an influence on the kind of treatment that patients with obesity receive [19–21]. Moreover, individuals that have been known to have had WLS are not seen as being responsible or actively involved in the process of weight reduction by providers [18], indicating the false belief that WLS does not include effort or difficulty for the patient. Weight-related bias therefore has to be considered another influencing factor. One might think that more negative attitudes may result in higher referral rates of WLS because HCPs may assume that their patients lack the willpower and endurance to lose weight with conservative treatment methods solely and thus are in need of a more radical treatment method such as surgery.
The question remains whether there is a so-called surgery-related type of stigmatization towards patients with obesity among health care professionals that influences the aforementioned treatment pathways.
Studies that investigated the willingness of general practitioners and HCPs in terms of recommending surgery and referring to a surgeon have been limited to small samples and specific patient groups (such as patient with type 2 diabetes) [10, 12]. Therefore, the aim of this study was to determine and explain referral behavior by general practitioners and internists. Additionally, recommendation of WLS is tested with regard to its potential mediating role in explaining the association between stigma or knowledge and referral to WLS. We hypothesized that the willingness to advise patients to undergo weight loss surgery and the willingness to refer patients to a surgeon are dependent on two major factors: knowledge about weight loss surgery and stigma towards patients with obesity and WLS. It is expected that higher knowledge, endorsing individual-based causes for obesity, and lower stigmatizing attitudes are associated with a higher probability to suggest WLS to patients, and also to refer them to a surgeon.
Methods
Participants
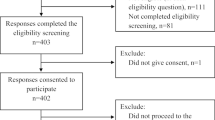
The sample consisted of general practitioners as well as internists (n = 201, response rate 16.3 %, originally 1236 physicians have been contacted). They received questionnaires by mail. Participants were chosen by randomly selecting different regions in Germany. For each region, all physicians that could be tracked down using the telephone directory received the letter and questionnaire and a stamped addressed return envelope. Informed consent was obtained from all subjects. Approval from the Ethics Committee of the University of Leipzig was obtained.
Procedure
Measures
Socio-Demographics and Other Measures
Participants were asked about their gender, age, their specific occupational working area as well as their body weight and height in order to calculate their BMI (in kg/m2).
Stigmatizing Attitudes
In order to investigate weight-related stigmatizing behavior, the short form of the Fat Phobia Scale [19] was used. The Fat Phobia Scale (FPS) has been used widely to test stigmatizing attitudes among health care professionals especially due to its good psychometric properties [20], making it possible to classify and compare the score to other scores which can be found in the literature. Calculations of Cronbach’s alpha indicated good reliabilities (α = 0.79). Contrary to other explicit measures of weight stigma, such as the Anti-Fat Attitude Test [21], the FPS provides a more subtle evaluation by providing the respondent with a semantic differential. Additionally, it is possible to also examine attitudes towards a normal weight person which can be compared to the person with obesity. Two vignettes (written description of two women, one being obese and the other one being normal-weight) were presented and placed separately within the questionnaire to avoid bias. Participants were asked to rate these women using 14 opposite adjective pairs (e.g., 1 = “lazy” and 5 = “industrious”). A mean score was calculated over all 14 adjectives. The greater the score of the Fat Phobia Scale, the more likely is this person to show negative attitudes towards people with overweight or obesity [19, 22].
Secondly, perceived causes of obesity were also examined. Participants were asked about the importance of “having no willpower” as a reason for the patients’ excess weight on a five-point-scale (1 = not important at all; 5 = exceptionally important).
Stigmatizing Attitudes Towards Weight Loss Surgery
In addition, participants were asked whether they agree with the statement “I find it too easy, if an individual with obesity can reach normal-weight through bariatric surgery.” on a five-point-scale (1 = I do not agree at all; 5 = I completely agree). In terms of known side effects and substantial changes associated with weight loss surgery, we argue that understating surgery as being “too easy” in terms of personal effort for weight change can be considered as an indicator for negative attitudes towards WLS and subsequently towards people with obesity.
Knowledge About Weight Loss Surgery
In this section, participants were asked about their general knowledge on weight loss surgery on a five-point-scale (1 = I do not know anything about it; 5 = I know a lot about it). In addition to that, participants were asked to rate the effectiveness of WLS by indicating it as being “useful” or “not useful at all.” In order to assess the perceived efficiency, participants were then asked to rate the amount of weight (in %) a patient with obesity can lose within 1 year after WLS was performed.
Dependent Variables: Recommending WLS and Referral to a Surgeon
Participants were asked whether or not they refer patients with obesity to other specialists and health care professionals (answer format: yes/no). If this was the case, an open question followed to state the type of specialist they refer their patients to.
Additionally, respondents were asked to indicate how often they recommended WLS to their patients. The answer format was a five-point Likert scale from 1 = never to 5 = very often.
Data Analysis
All calculations were performed by using STATA 13.1. for Windows (18). The frequency of recommending weight loss surgery was used as the dependent variable in a linear regression model. Beta-coefficients as well as p values are reported in the context of the research question. The model contained the following independent variables: personal knowledge about WLS, whether it was rated as useful, participants’ BMI, their belief about the amount of weight one can lose after WLS, their stigmatizing attitudes (FPS score overweight vignette), endorsement for a lack of willpower as a major cause of obesity, whether they think it is too easy to lose weight with WLS, and their age and gender. BMI categories were determined according to WHO conventions [23].
A logistic regression model was used to investigate determinants of referral behavior. We subdivided the dependent variable to indicate either “referral to a surgeon” or “referral to other specialties and no referral to a surgeon.” In addition to recommendation frequency, the same independent variables (age, gender, BMI) as in the linear model were introduced. Odds ratios are reported for this model.
To further investigate mediation effects, a mediation analysis was performed using the STATA 13.1 [24] command medeff to detect direct effects, indirect effects, and the overall effect. Two mediation models were run, using knowledge and stigma as separate independent variables, recommendation frequency as the mediating variable, and referral behavior as the outcome variable. Adjustments were made for age, gender, and BMI of the participants.
Results
Table 1 describes the general characteristics of the sample. The mean age was approximately 53.3 years and 45.8 % of the participants were female. The majority in this sample were general practitioners (80.0 %), 35.5 % were overweight and only 7.6 % can be classified as being obese. For gender and age, this sample replicated current distributions of general practitioners and internists in Germany [25, 26].
The participants state that they sometimes (48.0 %) or rarely (34.3 %) recommended WLS to their patients. Similar patterns were found by looking at the number of physicians, who refer their patients to a surgeon (17.8 %), to other weight loss treatments (38.4 %), and not at all (43.8 %). Information on knowledge about weight loss surgery reveals that more than 70 % rated their own knowledge as moderate to good, and 56.4 % found WLS as being useful to reduce body weight. According to the participants, the mean percentage of body weight that can be lost with WLS is 21.2 % (overall range 0.0 to 80.0 %). For stigma-related variables, the mean fat phobia score of this sample was 3.4, indicating a slightly negative attitude towards people with obesity or overweight. One in three respondents agreed with the statement that weight loss through WLS is a too easy option for the patients. With regard to perceived causes of obesity, more than half of the participants (58.3 %, including category 5 and 4) believed that “having no willpower” is the main reason for excess weight, whereas only 13.3 % (including category 1 and 2) did not or only slightly agree with this statement.
In addition, Table 2 shows the results of the linear regression model with the item “How often do you recommend WLS?” as the dependent variable (F (9152) = 9.36, p < 0.001; R 2 = 0.3565). In general, it was found that all knowledge variables were associated with the frequency of recommendations of WLS. The more respondents knew about WLS, the greater the frequency of recommending it to their patients (b = 0.258; p < 0.001). However, if they perceived WLS as not useful, recommendations decreased (b = −0.616; p < 0.001). Recommendations were linked to the percentage of body weight loss, which participants thought could be managed with WLS: physicians, who rated the loss as being greater, recommended WLS more often (b = 0.014; p = 0.03) than physicians who believed that only smaller amount of body weight could be lost with WLS. Results for the stigma towards individuals with obesity, the FPS, as well as the question for perceived causes of obesity (no willpower) were not significant; however, results from the stigma towards WLS revealed a relation between stigma in physicians and the frequency of recommendation of WLS. If physicians believed that it is too easy to lose weight with WLS, they were less likely to recommend WLS to their patients (b = −0.129; p = 0.013).
Table 3 summarizes the results of the logistic regression model with “referral to a surgeon vs. no referral or referral to other treatment” as the dependent variable. This model demonstrates that neither stigma towards WLS nor knowledge of WLS significantly influenced the physicians’ decision to refer patients to a surgeon. The only significant predictor was the frequency of recommendations, which increased the likelihood of referral to a surgeon by OR = 2.169 (p = 0.043). The effect of stigmatizing attitudes towards WLS on referral behavior vanished after introducing the frequency of recommending WLS.
A mediation analysis (Fig. 1) was performed to investigate effects of stigma towards WLS and knowledge on referral behavior, and whether these affects were mediated by recommendation. For recommendation, a significant direct effect (b = −0.107, p < 0.05) of stigma on referral behavior was observed, but also a significant mediated effect (b = −0.263, % of total effect through mediation = 43.68 %) of stigma through recommendation on referral behavior (a). Participants, who reported more negative attitudes towards WLS, responded with fewer recommendations and hence fewer referral to a surgeon. Furthermore, we noted a significant direct effect (b = 0.026, p < 0.05) of knowledge on referral behavior but also a significant mediated effect (b = 0.373, % of total effect through mediation = 71.1 %) of knowledge through recommendation on referral behavior (b). Participants, who expressed more knowledge of WLS, responded with more recommendations and hence were more likely to refer patients to a surgeon.
Discussion
The results indicate that knowledge about, as well as stigma towards WLS was related to the frequency of recommendations for WLS. The more practitioners subjectively knew about WLS and the more they believed that it is an effective method, the more likely they were giving recommendations for WLS. In terms of stigma towards WLS, it was found that these physicians tended to recommend WLS less often, if they believed that it was too easy to lose weight with WLS. In terms of mediation pathways, surgery-related stigmatization as well as knowledge at least partly explained the association of recommendation and referral behavior. Additionally, the proportion of providers that recommended surgery or referred to surgery was comparably low when assuming that our participants mainly thought about obesity class I patients as in comparable studies [11]. In light of tendencies among surgical colleagues to offer surgery not only to those with a BMI over 40 kg/m2 or diabetic patients with obesity class 2, but also to patients with lower BMIs and severe co-morbidities [27], our findings have great implications for clinical practice. It seems essential to intervene in order to reduce surgery-related stigma and in order to increase knowledge about surgery in outpatient providers as they are central in the care for patients with obesity.
Many physicians still believe that obesity is controllable, self-inflicted and the patients themselves are responsible for it; hence, weight could easily be reduced by dieting and exercise instead of concentrating on the benefits of WLS [18, 28, 29]. Again, there are calls to move away from making unsuccessful pre-operation dieting a prerequisite for candidacy for surgery [27], but rather to make a decision for or against surgery based on the patients’ weight history and well-being. Instead of focusing on losing weight or concentrating on numbers, the fact that WLS has been shown to help treating obesity-related comorbidities such as T2D or cardiovascular diseases should be taken into account. When WLS is considered as a treatment method, health care professionals ought to look at the whole picture and determine the severity of obesity on an individual level, for instance by using the Edmonton Staging System of Obesity [30, 31]. A lack of knowledge about surgery and its prerequisites should not act as a barrier to successful treatment of obesity-related comorbidities. This is undermined by findings from the USA, where only two thirds of providers caring for T2D patients declare that they follow the guidelines for surgery entry and only 20 % acknowledge the possible need for patients with lower BMI but comorbid T2D [11]. Current views increasingly suggest bariatric surgery as being beneficial to treat diabetic patients, which implies that candidacy for surgery ought to rather be based on the presence of comorbidities, rather than BMI alone [32, 33]. In other words, no patient should be prohibited from taking the chance of reaching a satisfactory health status if he or she is applicable for WLS according to medical diagnosis and criteria.
It remains unknown, what kind of role patients play in this context and whether they have an influence on the referral behavior of the physician. Because stigma and knowledge only have an impact on the utterance of a recommendation and not elicit factual transfer, one could conclude that it may additionally depend on the patient whether there is a referral or not. Furthermore, the impact that surgery-related stigma might have on the patient’s decision in addition to the physician’s decision on the treatment pathway should also be part of future investigations. Our findings indicate that this reluctance in referral behavior may in part be due to stigmatizing attitudes and a lack of knowledge in practitioners. This might also have a major impact on the patients themselves. Interestingly, about 43.3 % of prospective surgery patients reported feelings of being treated disrespectfully by a HCP because of their weight, compared to 21.6 % of non-surgery patients [34]. As a result, patients may feel stigmatized and internalize the physician’s attitude towards WLS, who might consider WLS as being too easy and “over-utilized” to reduce excess body weight [35]. Previous research suggests that stigma does not stop after those affected by it have lost weight. Weight-related bias rather continues independent of the weight loss method [18], but seems to be more pronounced when patients lost weight by the help of surgery. In the same study, most negative attitudes were shown towards people who lost weight with surgery, hence put in less effort compared to dieting or exercising [18]. Surgery-related stigma might result in patients being fearful of surgery, simply because they do not want to be stigmatized for choosing WLS, remaining a target for weight teasing despite having lost weight. On the other hand, signaling that WLS is like “losing weight simply overnight” and without any endeavor could foster unrealistic weight loss goals or expectations. Therefore, the patient’s perspective should also be a focus of future investigations covering this area of research to fully understand stigma in the context of weight loss surgery.
One limitation of this study is the low response rate. However, compared to other related studies, the size of the sample is very similar [2, 11, 13, 35, 36]. Nevertheless, a larger sample might—for instance by having incentives—make it possible to look at the mediation pathways in greater detail. Moreover, referral behavior to WLS was assessed using an open question. It might therefore be possible that respondents did not state “weight loss surgery” as an option because it did not cross their minds immediately. It has been argued that one possible explanation for the results stated above might be the patient’s choice against WLS. This could have been assessed by asking about the actual percentage of patients that underwent weight loss surgery in response to their physician’s referral. With regard to the measurements used to determine the level of stigma in this sample, a scale which investigates implicit weight stigmatization could be added in addition to the Fat Phobia Scale. As has been argued in the literature, this might help to detect the presence of automatic, unconscious prejudice otherwise hidden by social desirability. Moreover, the short version of the FPS has been used for economic reasons, because it is less timely and easily applicable. However, a more comprehensive and up-to-date measurement should be the focus of future studies in this context.
Conclusion
Because WLS is a good method for patients with severe obesity, it is of great importance to inform the medical staff, clear up misunderstandings, and reduce stigma towards WLS. Family doctors and internists should be free of prejudice against overweight and obesity and sufficiently inform the patient objectively or give them advice on suitable weight reduction methods. The decision for, or against a specific weight loss strategy, should be made self-contained and without any social pressure. Future research should evaluate whether weight-related stigma not only affects recommendations but also how stigma in general might influence the quality of counseling (e.g., informed consent about possible risk related to surgery) or follow-up examinations by the physician. Possible intervention such as the “5As” of obesity should aim to inform HCPs with different backgrounds about bariatric surgery as a part of obesity management and to improve physician-patient-interaction in order to assure integrated treatment and counseling [37–39].
References
Picot J, Jones J, Colquitt JL, et al. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess. 2009;13:1–190. 215–357, iii-iv.
Rosemann T, Wensing M, Rueter G, et al. Referrals from general practice to consultants in Germany: if the GP is the initiator, patients’ experiences are more positive. BMC Health Serv Res. 2006;6:5.
Höhne A, Jedlitschka K, Hobler D, et al. Hausarztzentrierte Versorgung in Deutschland. Der Hausarzt als Lotse? Gesundheitswesen. 2009;71:414–22.
Piché M, Auclair A, Harvey J, et al. How to choose and use bariatric surgery in 2015. Can J Cardiol. 2015;31:153–66.
Maggard MA, Shugarman LR, Suttorp M, et al. Meta-analysis: surgical treatment of obesity. Ann Intern Med. 2005;142:547–59.
Garb J, Welch G, Zagarins S, et al. Bariatric surgery for the treatment of morbid obesity: a meta-analysis of weight loss outcomes for laparoscopic adjustable gastric banding and laparoscopic gastric bypass. Obes Surg. 2009;19:1447–55.
Expertengruppe Metabolische Chirurgie. Berechnungen der Expertengruppe Metabolische Chirurgie auf Grundlage nationaler Statistiken. München; 2012. Available from: http://www.expertengruppe-mbc.de/berlin-2012.html
Vasas P, Pór F. Surgical options for reducing body weight. Orv Hetil. 2014;155:971–7.
Sikorski C, Luppa M, Dame K, et al. Attitudes towards bariatric surgery in the general public. Obes Surg. 2013;23:338–45.
Avidor Y, Still CD, Brunner M, et al. Primary care and subspecialty management of morbid obesity: referral patterns for bariatric surgery. Surg Obes Relat Dis. 2007;3:392–407.
Sarwer DB, Ritter S, Wadden TA, et al. Physicians’ attitudes about referring their type 2 diabetes patients for bariatric surgery. Surg Obes Relat Dis. 2012;8:381–6.
Dumon KR, Murayama KM. Bariatric surgery outcomes. Surg Clin N Am. 2011;91:1313–38.
Balduf LM, Farrell TM. Attitudes, beliefs, and referral patterns of PCPs to bariatric surgeons. J Surg Res. 2008;144:49–58.
Hell E, Miller K. Bariatric surgery—stereotypes and paradigms. Zentralbl Chir. 2002;127:1032–4.
Wee CC, Huskey KW, Bolcic-Jankovic D, et al. Sex, race, and consideration of bariatric surgery among primary care patients with moderate to severe obesity. J Gen Intern Med. 2014;29:68–75.
Foster GD, Wadden TA, Makris AP, et al. Primary care physicians’ attitudes about obesity and its treatment. Obes Res. 2003;11:1168–77.
Wadden TA, Anderson DA, Foster GD, et al. Obese women’s perceptions of their physicians’ weight management attitudes and practices. Arch Fam Med. 2000;9:854–60.
Vartanian LR, Fardouly J. The stigma of obesity surgery: negative evaluations based on weight loss history. Obes Surg. 2013;23:1545–50.
Bacon JG, Scheltema KE, Robinson BE. Fat phobia scale revisited: the short form. Int J Obes Relat Metab Disord. 2001;25:252–7.
Stein J, Luppa M, Ruzanska U, et al. Measuring negative attitudes towards overweight and obesity in the German population—psychometric properties and reference values for the German short version of the Fat Phobia Scale (FPS). PLoS ONE. 2014;9, e114641.
Lewis RJ, Cash TF, Jacobi L, et al. Prejudice toward fat people: the development and validation of the antifat attitudes test. Obes Res. 1997;5:297–307.
Sikorski C, Luppa M, Brähler E, et al. Obese children, adults and senior citizens in the eyes of the general public: results of a representative study on stigma and causation of obesity. PLoS ONE. 2012;7, e46924.
World Health Organization. Obesity: preventing and managing the global epidemic. Genf; 2000.
Hicks R, Tingley D. Causal mediation analysis. Stata J. 2011;11:609–15.
Kopetsch T. Dem deutschen Gesundheitswesen gehen die Ärtze aus!: Studie zur Altersstruktur- und Arztzahlentwicklung. Berlin; 2010.
Bundesärztekammer. Struktur der Ärzteschaft 2013; 2013. Available from: http://www.bundesaerztekammer.de/downloads/Stat13AbbTab.pdf
Sharma AM. Is it time to lower the bar for bariatric surgery? Obes Surg. 2014;24:520–1.
Warner CH, Warner CM, Morganstein J, et al. Military family physician attitudes toward treating obesity. Mil Med. 2008;173:978–84.
Thuan J, Avignon A. Obesity management: attitudes and practices of French general practitioners in a region of France. Int J Obes (Lond). 2005;29:1100–6.
Sharma AM, Kushner RF. A proposed clinical staging system for obesity. Int J Obes (Lond). 2009;33:289–95.
Gill RS, Karmali S, Sharma AM. The potential role of the Edmonton obesity staging system in determining indications for bariatric surgery. Obes Surg. 2011;21:1947–9.
O’Brien PE. Controversies in bariatric surgery. Br J Surg. 2015;102:611–8.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes—3-year outcomes. N Engl J Med. 2014;370:2002–13.
Anderson DA, Wadden TA. Bariatric surgery patients’ views of their physicians’ weight-related attitudes and practices. Obes Res. 2004;12:1587–95.
Sansone RA, McDonald S, Wiederman MW, et al. Gastric bypass surgery: a survey of primary care physicians. Eat Disord. 2007;15:145–52.
Perlman SE, Reinhold RB, Nadzam GS. How do family practitioners perceive surgery for the morbidly obese? Surg Obes Relat Dis. 2007;3:428–33.
Campbell-Scherer DL, Asselin J, Osunlana AM, et al. Implementation and evaluation of the 5As framework of obesity management in primary care: design of the 5As Team (5AsT) randomized control trial. Implement Sci. 2014;9:78.
Rueda-Clausen CF, Benterud E, Bond T, et al. Effect of implementing the 5As of obesity management framework on provider-patient interactions in primary care. Clin Obes. 2014;4:39–44.
Vallis M, Piccinini-Vallis H, Sharma AM, et al. Clinical review: modified 5 As: minimal intervention for obesity counseling in primary care. Can Fam Physician. 2013;59:27–31.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
FUCEJ, CLS, HHK, SRH declare to have no conflict of interest. CLS has received speaker honoria from Johnson & Johnson Medical.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study. Participants were informed about the study on the first page of the questionnaire and they were instructed that upon returning the filled out questionnaire, their data would be used for scientific publications.
Statement of Human Rights
This study has been approved by the ethics committee of the University of Leipzig and has been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Jung, F.U.C.E., Luck-Sikorski, C., König, HH. et al. Stigma and Knowledge as Determinants of Recommendation and Referral Behavior of General Practitioners and Internists. OBES SURG 26, 2393–2401 (2016). https://doi.org/10.1007/s11695-016-2104-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-016-2104-5