Abstract
Background
The purpose of this study is to register the number of steps taken during the first postoperative week by patients who underwent laparoscopic Roux-en-Y gastric bypass surgery (LRYGB) and evaluate whether goals for steps taken per day could affect the patients’ physical activity level, time to first flatus and stool, days at hospital, and recovery.
Methods
Fifty-five patients undergoing LRYGB surgery carried a step counter on the first postoperative week and recorded the number of steps taken. They also registered hours spent sitting, lying down and sleeping, assessed their level of recovery, and noted the first day of flatus and defecation. The intervention group was informed to try to reach a daily goal regarding the number of steps to be taken.
Results
The patients took 2000–3000 steps/day on the first postoperative days. There were significant differences between the groups in numbers of steps taken in favor of the intervention group on four of the postoperative days. The patients in the intervention group found that the goals were set at the right level, except for the second day, where they thought 1300 steps were too few. There were no significant differences between the groups in the mean time spent sitting or lying. Neither were there any differences in time for first flatus, stool, days at hospital, nor degree of recovery.
Conclusions
Goals set for steps taken per day increase the amount of steps walked in patients undergoing gastric bypass surgery. Step counters and predefined goals can be used to facilitate mobilization after obesity surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Bariatric surgery is associated with long-term weight loss, a lower risk of disease, and decreased overall mortality [1, 2], although the benefits should still be weighed against the risk of complications. The overall mortality in the first 30 days after bariatric surgery is low, and major complications affect approximately 1–2 % of people operated [3–5].
Due to tradition, patients undergoing major abdominal surgery have been mostly bedridden in the immediate postoperative phase [6–8]. This prolonged bed rest combined with physical inactivity causes co-morbidity related to reduced muscle mass and lung volumes and impaired heart function, and the costs of the consequences are high [6–11]. Another clinically often emphasized consequence of bedrest and immobilization is prolonged postoperative ileus. However, evidence is missing concerning the link between early ambulation with recovery of bowel function passing flatus/stool and having bowel movements [12, 13]. Nowadays, the time in bed is still considerable but has been reduced due to increased awareness of the risks related to immobilization and routine of thrombosis prophylaxis. A larger proportion of patients also undergo laparoscopic or minimal invasive surgery with smaller impact on respiratory function, lower risk of postoperative complications, and less postoperative pain [14, 15]. Early and frequent physical activity after abdominal surgery is one of several important factors evaluated in clinical pathways to promote a speedy recovery, shorten the period of care, and reduce costs [16–18]. In addition, no disadvantages have been found [16–18].
Step count devices have recently become a common tool to measure and increase the level of physical activity [19]. Using targets/goals in combination with the registration of number of steps has also been shown to increase the number of steps over registration of the results only [20]. The goals must be challenging but cannot exceed the person’s capacity. There is a linear relationship between the degree of goal setting and achievement, and a factor for success to increase physical activity is to set goals for steps taken [19, 21] Use of individual goals after laparoscopic cholecystectomy has previously been shown to have an impact on women’s recovery [22].
There is currently limited knowledge of the number of steps that patients walk during the first week after LRYGB surgery and whether a goal for steps taken per day increases the amount of physical activity. Knowledge is also lacking on how much time during which the patients are inactive in the first week after surgery. The aim of this study was therefore to register the number of steps taken during the first postoperative week by patients who underwent an LRYGB and to evaluate whether a well-defined goal of steps to take per day could affect the patients’ level of physical activity, time of first flatus and stool, days at hospital, and postoperative recovery.
Method
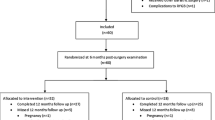
This randomized controlled trial included adult patients (>18 years) undergoing laparoscopic Roux-en-Y gastric bypass surgery (LRYGB) at a university hospital in Sweden. Exclusion criteria were the following: previous bariatric surgery, difficulties walking or using walking aids, and patients unable to use Swedish in speech and writing. Of 78 patients assessed for eligibility, 66 patients were randomized. A strict randomization was not performed as it was not possible to separate patients from the two groups postoperatively, and if not separated, there was a risk of interference on the part of the intervention group to the registration group. Patients who underwent surgery the same week were therefore randomized to either the intervention or registration group. Opaque, sealed envelopes were drawn by an independent person who did not have knowledge of the number of patients/ week or which patients were scheduled each week. In addition, the coordinator who planned the operation schedule had no knowledge of the randomization.
Before surgery, all patients received written information on the importance of being active postoperatively and received standard care according to current treatment programs. All patients in the intervention group and the registration group wore a step counter (SILVA, Ex3 Plus) throughout their waking hours each day for a week starting the day after surgery.
This step counter contains a 3D sensor to detect movement by using three axes: X, Y, and Z. Depending on how the patient moves, the step counter assesses movements using the three axes at the same time. It also contains software to interpret the movement and force and filters unwanted data. The step counter was worn around the neck, as this has been found to give accurate data in a population of obese women [23].
All patients were asked to note the number of steps walked in the activity diary (primary outcome) and how many hours they had been sitting, lying, or sleeping in the past 24 h, every evening during the first week after surgery. First flatulence, first stool, and number of days at the hospital were noted in the diary. On the seventh day, a self-assessed questionnaire on general postoperative recovery was included, “Postoperative Recovery Profile” (PRP) [24]. This questionnaire is short and covering five dimensions of recovery (physical symptoms, physical functions, psychological, social, and activity) [24]. The included items are statements which patients rate on a four-point scale: none, mild, moderate, and severe, and lower total rating corresponds to a higher degree of recovery.
The intervention group also received goals for the number of steps to achieve and exceed each day. The goal was gradually increased: day 1: 1000 steps; day 2: 1300 steps; day 3: 1600 steps; day 4: 2000 steps; day 5: 3000 steps; day 6: 4000 steps; day 7: >4000 steps. The targets were based on clinical experience and the results in a pilot study of five patients undergoing LRYGB who noted the number of steps for 1 week postoperatively. The intervention group also registered whether they experienced the day’s goal (number of steps) as being too high, just right, too low, or much too low.
Statistics and Ethics
The sample size calculation was based on the difference in the number of steps. Twenty patients were needed in each group to detect a difference of 250 steps between groups with 80 % power at a significance level of 5 % based on the results of the results of the pilot study. To compensate for dropouts and possible technical problems with accelerometers, we aimed to include approximately 30 patients/group.
SPSS version 22.0 was used for the statistical analyses. To present the results, mean and standard deviation or standard error of the mean was used for continuous variables and median and minimum/maximum or number of patients for categorical variables. ANOVA, t test, and Mann–Whitney U test were used for comparisons between the two groups. Wilcoxon’s sign rank test was used for analyses within the two groups. Significance tests were two-sided and conducted at the 5 % significance level.
The patients received written and verbal information, and informed consent was obtained from all participants included in the trial. The Regional Ethical Review Board of Gothenburg, Sweden approved the study (Reg no. 2012-12-20). The trial was registered in the national register of research, FoU, in Sweden, no. 91721.
Results
Of the 66 patients randomized, 55 were included in the final analysis (see Fig. 1). No significant differences were observed between the patients who fulfilled the exclusion criteria or who dropped out when compared to those who participated. Table 1 provides descriptive data for the 55 patients. No significant differences were seen between the groups before surgery.
The number of steps walked and the goal given for each day are shown in Table 2. There was an overall difference between the groups (ANOVA, p < 0.001). There were significant differences between the groups in number of steps taken during four of the days (days 2, 5, 6, and 7) in the first postoperative week (p < 0.05). The proportion of patients in the intervention group who managed to reach the goal was >60 % during the week and, on the first two postoperative days, 79 and 93 % of those patients fulfilled the goal.
The patients in the intervention group found the goals to be set at the right level except for the second day, where they thought that 1300 steps were too few.
The mean times spent sitting or lying during the first postoperative week are presented in Fig. 2. There were no significant differences between the groups. Neither were there any differences in time to first flatus and stool nor days at hospital (Table 1).
Recovery after surgery measured by PRP [24] was similar in the two groups on the seventh day after surgery: intervention group in median (min–max) 110.5 units (99–134) and registration group 111.0 units (62–120) (lower figures indicate a higher degree of recovery).
No side effects of the intervention were recorded.
Discussion
The results of this study indicate that goals set for steps taken per day increase the amount of steps walked among patients undergoing gastric bypass surgery. The intervention group took a significantly higher number of steps on postoperative days 2, 5, 6, and 7. There was no significant difference between the groups on the first postoperative day even though there was a difference of 494 steps taken (Table 2). This is probably due to a type II error while larger group would have been needed to reach statistical significance. The largest differences between the groups, 1200–1300 steps, were seen on the last days of the recording. This can be interpreted such that the goals set made it easier for the patients to be more active after returning home from the hospital. There is always a risk that patients are afraid of being active postoperatively, and it is a challenge to convince them and their relatives of the opposite and encourage them to walk and be as active as possible. Obesity itself often limits the ability to be physically active as to walk and run [25]. In this trial, the patients did not rate their preoperative activity level and it is possible that differences in preoperative physical activity level may have affected the results. However, no side effects of the intervention were observed, and this information can be valuable in the work to encourage patients to be more active in the postoperative phase.
The patients in the intervention group exceeded the goal of the number of steps taken per day during all the days of the week, except on the sixth day. The number of steps increased less during the first postoperative days than at the end of the week. The rapid escalation that occurred in order to reach the goal during the last days in the week may explain this, but on the other hand, the goal of the number of steps to be taken was based on the results from patients in a pilot study. The results in the main trial indicate that the patients in this group walked more. It was thus interesting to analyze how the patients experienced the goals that were set. In median, they thought the goals were neither too high nor too low, except for the second day when they thought it was too low. In future trials, even higher goals may be set to further increase activity. An idea is also to set a reachable goal but to tell the patients not only to reach that goal but to try to take as many steps as possible.
There is no evidence that mobilization accelerates recovery in bowel function after surgery [12, 13]. To our knowledge, there is only one trial evaluating the effect of mobilization on postoperative ileus after laparotomy [13]. In the trial, they conclude that ambulation, as a means to help resolve postoperative ileus, may be more perceived than real [13]. In contrast, there are trials where a concurrence between immobilization and decreased bowel function is proven [26, 27]. Even though the patients in the intervention group walked more than the patients in the registration group, this had no impact on postoperative recovery, first flatus, stool, or days at hospital. An interpretation is that increased activity does not have any impact on these outcomes, but other factors may also have influenced the results as differences in medication or nutrition. These variables were not registered in this trial which is another limitation of the study.
In previous trials of effects of fast-track programs, including intensive mobilization in patients undergoing upper open abdominal surgery, there are significant differences between groups participating and not participating in the concept [17]. However, the concepts include several other factors that may also have an impact on the outcome. The results of our study do not show any significant differences, but it is possible that higher goals and more steps could have an impact on recovery, bowel function, and time at hospital. It is also possible that the increased activity may have had an impact on other functions not evaluated in this trial as recovery of respiratory function and lower decrease in muscle mass.
The differences in the number of steps did not influence the patients’ inactive time, i.e., time spent sitting and lying without sleeping. The registration of time is less reliable, however, as the patients estimated the time, in contrast to the number of steps taken, which was registered by the step counter. A limitation of the study is the lack of objective and reliable registrations of time spent sitting or lying or time to first flatus and stool. It is possible to register activity with different tools worn around the arm or leg. We did not have access to this type of equipment when this study was undertaken, but new, easy, useable, and cheap testers that are being developed can be used in future clinical trials.
Step counters have been shown in a meta-analysis to have a positive effect on the increase of physical activity in intervention studies [20]. Factors that have been identified to improve the likelihood of a successful outcome in people using step counters to increase their physical activity level are goals, registering the number of steps taken and wearing step counters, where goal setting has the greatest impact on steps taken [20]. For instance, one study has found a correlation between setting a goal for the number of steps to take per day and the actual number of steps taken [28].
Based on the knowledge that simply wearing a step counter can influence the number of steps taken, another limitation in the study is the fact that the patients in the registration group also wore step counters and noted the results daily. This could have been avoided by using blinded step counters. There is also a possibility that the patients shook the step counter to show a greater number of steps, which is a source of uncertainty in all step counters.
In conclusion, goals set for steps to take per day increase the amount of steps walked in patients undergoing gastric bypass surgery. Step counters and predefined goals can be used to facilitate mobilization after obesity surgery.
References
Sjöstrom L. Bariatric surgery and reduction in morbidity and mortality: experiences from the SOS study. Int J Obes. 2008;32 Suppl 7:93–7.
Sjöström L, Narbro K, Sjöström CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357(8):741–52.
Buchwald H, Estok R, Fahrbach K, et al. Trends in mortality in bariatric surgery: a systematic review and meta-analysis. Surgery. 2007;142(4):621–32.
Årsrapport 2011. Scandinavian obesity surgery registry (SOREG) 2011; Available from: http://www.ucr.uu.se/soreg/index.php/dokument/cat_view/58-dokument/57-arsrapporter.
Colquitt JL, Picot J, Loveman E, Clegg AJ. Surgery for obesity. Cochrane Database Syst Rev. 2009;(2):CD003641. doi:10.1002/14651858.CD003641.pub3.
Monteleone S, Dalla Toffola E et al. Recovery of deambulation after cardio-thoracic surgery: a single center experience. Eur J Phys Rehabil Med. 2015. In press.
Fagevik Olsén M, Hahn I, Nordgren S, et al. Randomized controlled trial of prophylactic chest physiotherapy in major abdominal surgery. Br J Surg. 1997;84:1535–8.
Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78(5):606–17.
Harper CM, Lyles YM. Physiology and complications of bed rest. J Am Geriatr Soc. 1988;36(11):1047–54.
FYSS-Fysisk aktivitet i sjukdomsprevention och sjukdomsbehandling Stockholm: Yrkesföreningar för Fysisk Aktivitet i samarbete med Statens folkhälsoinstitut. FHI Rapport 2008(2008):4.
Bloomfield SA. Changes in musculoskeletal structure and function with prolonged bed rest. Med Sci Sports Exerc. 1997;29(2):197–206.
Story SK, Chamberlain RS. A comprehensive review of evidence-based strategies to prevent and treat postoperative ileus. Dig Surg. 2009;26(4):265–75.
Waldhausen JH, Schirmer BD. The effect of ambulation on recovery from postoperative ileus. Ann Surg. 1990;212(6):671–7.
Olbers T, Fagevik Olsén M, Maleckas A, et al. Randomized clinical trial of laparoscopic Roux-en Y gastric bypass versus laparoscopic vertical banded gastroplasty for obesity. Br J Surg. 2005;92(5):557–62.
Fagevik Olsén M, Josefson K, Lönroth H. Chest physiotherapy does not improve the outcome in laparoscopic fundoplication and vertical banded gastroplasty. Surg Endosc. 1999;13:260–3.
Frutos MD, Lujan J, Hernandez Q, et al. Clinical pathway for laparoscopic gastric bypass. Obes Surg. 2007;17(12):1584–7.
Olsen MF, Wennberg E. Fast-track concepts in major open upper abdominal and thoracoabdominal surgery: a review. World J Surg. 2011;35(12):2586–93.
Delaney CP, Zutshi M, Senagore AJ, et al. Prospective, randomized, controlled trial between a pathway of controlled rehabilitation with early ambulation and diet and traditional postoperative care after laparotomy and intestinal resection. Dis Colon Rectum. 2003;46(7):851–9.
Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health: a systematic review. JAMA. 2007;298(19):2296–304.
Kang M, Marshall SJ, Barreira TV, et al. Effect of pedometer-based physical activity interventions: a meta-analysis. Res Q Exerc Sport. 2009;80(3):648–55.
Locke EA, Latham GP. Building a practically useful theory of goal setting and task motivation. A 35-year odyssey. Am Psychol. 2002;57(9):705–17.
Wasowicz-Kemps DK, Slootmaker SM, Kemps HM, et al. Resumption of daily physical activity after day-case laparoscopic cholecystectomy. Surg Endosc. 2009;23(9):2034–40.
Wiklund M, Cider Å, Olsén MF. Accuracy of a pedometer and an accelerometer in women with obesity. Open Obes J. 2012;4(1):11–7.
Allvin R, Ehnfors M, Rawal N, et al. Development of a questionnaire to measure patient-reported postoperative recovery: content validity and intra-patient reliability. J Eval Clin Pract. 2009;15(3):411–9.
Wiklund M, Olsén MF, Willén C. Physical activity as viewed by adults with severe obesity, awaiting gastric bypass surgery. Physiother Res Int. 2011;16(3):179–86.
Iovino P, Chiarioni G, Bilancio G, et al. New onset of constipation during long-term physical inactivity: a proof-of-concept study on the immobility-induced bowel changes. PLoS One. 2013;8(8):72608.
Liu F, Kondo T, Toda Y. Brief physical inactivity prolongs colonic transit time in elderly active men. Int J Sports Med. 1993;14(8):465–7.
Dishman RK, Vandenberg RJ, Motl RW, et al. Dose relations between goal setting, theory-based correlates of goal setting and increases in physical activity during a workplace trial. Health Educ Res. 2010;25(4):620–31.
Acknowledgments
The work reported in this article was carried out with grant support from The Local Research and Development Board for Gothenburg and Södra Bohuslän.
Statement of Human Rights
All procedures were performed in accordance with the ethical standards of the regional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of Interest
The authors declare that they have no competing interests.
Statement of Informed Consent
Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wiklund, M., Sundqvist, E. & Fagevik Olsén, M. Physical Activity in the Immediate Postoperative Phase in Patients Undergoing Roux-en-Y Gastric Bypass—a Randomized Controlled Trial. OBES SURG 25, 2245–2250 (2015). https://doi.org/10.1007/s11695-015-1690-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-015-1690-y