Abstract
Background
Serum bile acids (BAs) are elevated after metabolic surgeries including Roux-en-Y gastric bypass (RYGB), ileal transposition (IT), and duodenal-jejunal bypass (DJB). Recently, BAs have emerged as a kind of signaling molecules, which can not only promote glucagon-like peptide-1 (GLP-1) secretion but can also regulate multiple enzymes involved in glucose metabolism. The aim of this study was to investigate whether expedited biliopancreatic juice flow to the distal gut contributes to the increased serum GLP-1 and BAs and benefits the diabetes control after DJB.
Methods
DJB, long alimentary limb DJB (LDJB), duodenal-jejunal anastomosis (DJA), and sham operation were performed in diabetic rats induced by high-fat diet (HFD) and low dose of streptozotocin (STZ). Body weight, food intake, oral glucose tolerance, insulin tolerance, glucose-stimulated insulin and GLP-1 secretion, fasting serum total bile acids (TBAs), and lipid profiles were measured at indicated time points.
Results
Compared with sham operation, DJA, DJB, and LDJB all achieved rapid and dramatic improvements in glucose tolerance and insulin sensitivity independently of food restriction and weight loss. DJB and LDJB-operated rats exhibited even better glucose tolerance, higher fasting serum TBAs, and higher glucose-stimulated GLP-1 secretion than the DJA group postoperatively. No difference was detected in insulin sensitivity and glucose-stimulated insulin secretion between DJA, DJB, and LDJB groups.
Conclusions
Expedited biliopancreatic juice flow to the distal gut was associated with augmented GLP-1 secretion and increased fasting serum TBA concentration, which may partly explain the metabolic benefits of DJB.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Duodenal-jejunal bypass (DJB) is a stomach-preserving procedure that was initially designed to explore the weight-independent anti-diabetic effects of gastric bypass surgery [1]. It has been proven effective in glycemic control in various type 2 diabetes mellitus (T2DM) rat models [1–3]. Exclusion of the proximal intestine [4], increased glucagon-like peptide-1 (GLP-1) secretion [5], and decreased SGLT1-mediated glucose absorption [3] have been suggested as possible explanations for the diabetic control after DJB. However, the underlying mechanisms are still far from completely elucidated.
Recently, bile acids (BAs) have emerged as potential glucose-lowering mediators of metabolic surgeries. Patti et al. reported that serum total bile acids (TBAs) were increased in patients with prior gastric bypass surgery, and the TBA concentration was positively correlated with peak GLP-1 levels while inversely correlated with 2-h postprandial blood glucose [6]. Cummings et al. found that elevated serum BAs after ileal transposition (IT) surgery was associated with decreased endoplasmic reticulum stress, which may further lead to improved glucose homeostasis by suppressing inflammation, improving insulin sensitivity and islets function [7]. Similarly, serum TBAs were also elevated within weeks after DJB surgery [2, 8].
As the chief constituents of bile, BAs are synthesized from cholesterol in hepatocytes. BAs were previously well-established for their important roles in dietary lipid absorption and cholesterol homeostasis, yet recently, they have emerged as signaling molecules with systemic endocrine functions [9]. By activating the farnesoid X receptor (FXR), BAs can not only suppress gluconeogenesis [10] but can also inhibit the expression of multiple lipogenetic genes [11]. Additionally, BAs are also capable of inducing GLP-1 release from enteroendocrine cells via activating the G protein-coupled receptor TGR5 located on the plasma membrane [12].
Though operated in different manners, Roux-en-Y gastric bypass (RYGB) [13], IT [14], DJB [1, 2], and biliopancreatic diversion (BPD) [15] could all result in dramatic alleviation of T2DM. We find that all these procedures share a common feature of enabling premature delivery of BAs to the distal ileum. The terminal ileum is not only an important location of L cells [16] but also the primary site for BA reuptake, where about 95 % of BAs are reabsorbed and then transported to the liver via portal circulation [9]. In this study, we performed duodenal-jejunal anastomosis (DJA), DJB, and long alimentary limb DJB (LDJB) on diabetic rats induced by high-fat diet (HFD) and low dose of streptozotocin (STZ). These three procedures are identical in excluding the proximal intestine and in expediting nutrient transits to the distal gut, while different in diverting the biliopancreatic juice. The aim of this design was to investigate whether expedited biliopancreatic flow to the distal gut contributes to the elevated serum GLP-1 and BAs and the diabetes control after DJB surgery.
Materials and Methods
Animals
All animal procedures were approved by the Animal Care and Utilization Committee of Shandong University. Eight-week-old male Wistar rats were purchased from Laboratory Animal Center of Shandong University (Jinan, China). The rats were housed in individual cages under constant ambient temperature and humidity in a 12-h light/dark cycle. After 1 week of acclimation, T2DM was induced as previously described [17]: The rats were firstly fed a HFD (40 % of calorie as fat, Huafukang Biotech Company, China) for 4 weeks to induce insulin resistance; then, a low dose of STZ (35 mg/kg) (Sigma, USA) was injected intraperitoneally to induce a diabetic state. Seventy-two hours after STZ injection, non-fasting blood glucose was measured in duplicate with a glucometer (Roche Diagnostics, Germany). The rats were considered diabetic if their non-fasting blood glucose exceeded 16.7 mmol/l.
Perioperative Diet Protocols
Rats undergoing operations were restricted to 10 % of Ensure (Abbott Laboratories, USA) for 2 days and then fasted overnight preoperatively. Within the first 24 h after operation, the rats could only get access to water. Then, the rats were fed 10 % of Ensure for 3 days, followed by a standard rodent chow until end of the study. The reason why we changed the feeding regime of all rats from HFD to standard rodent diet after operation is because postoperative HFD feeding could impair the improved glucose tolerance and insulin sensitivity after DJB [18]. Body weight and food intake were tracked for 12 weeks after surgery.
Surgical Procedures
Forty diabetic rats were randomly allocated into sham operation, DJA, DJB, and LDJB groups (with ten rats in each group). All surgeries were conducted under anesthesia with 10 % of chloral hydrate (3 ml/kg).
-
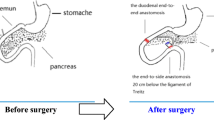
Sham operation: Duodenum was transected at 0.5 cm distal to the pylorus, and jejunum was transected at 10 cm distal to the ligament of Treitz; then, re-anastomosis was made in situ (Fig. 1a).
Fig. 1 Illustration of operations. a Sham operation. In the sham operation, duodenum is transected at 0.5 cm distal to the pylorus, and jejunum is transected at 10 cm distal to the ligament of Treitz; then, re-anastomosis is made in situ. b DJA. DJA surgery is similar to DJB and LDJB in excluding the proximal intestine and expediting ingested nutrients to the distal gut except that it does not accelerate biliopancreatic flow to the lower intestine. c DJB. DJB shortens the distance between duodenal papilla and terminal ileum by 15 cm. d LDJB. LDJB shortens the distance between duodenal papilla and terminal ileum by 30 cm
-
DJA: Duodenum was transected at 0.5 cm distal from the pylorus, and the stump was closed with a 7-0 silk suture (Ningbo Medical Needle, China). Then, the proximal duodenum was connected to the jejunum at 10 cm distal to the ligament of Treitz in an end-to-side fashion. DJA surgery does not expedite biliopancreatic flow to the terminal ileum (Fig. 1b).
-
DJB: DJB surgery was performed as previously described [19]: Duodenum was transected at 0.5 cm distal to the pylorus, and the stump was closed. Then, jejunum was transected at 10 cm distal to the ligament of Treitz, and the distal jejunum was connected to the proximal duodenum in an end-to-end fashion (duodenojejunal anastomosis). Finally, the biliopancreatic limb was anastomosed to the alimentary limb at 15 cm distal to the duodenojejunal anastomosis in a Roux-en-Y fashion. DJB shortens the distance between duodenal papilla and the terminal ileum by 15 cm (Fig. 1c).
-
LDJB: LDJB was identical to DJB except that the biliopancreatic limb was anastomosed to the alimentary limb at 30 cm distal to the duodenojejunal anastomosis. LDJB shortens the distance between duodenal papilla and the terminal ileum by 30 cm (Fig. 1d).
Oral Glucose Tolerance Test (OGTT)
OGTT was performed preoperatively and at 2 and 12 weeks postoperatively. After an overnight fast, blood glucose was measured at 0, 15, 30, 60, 120, and 180 min after oral glucose administration (1 g/kg).
Insulin Tolerance Test (ITT)
ITT was conducted to evaluate systemic insulin sensitivity preoperatively and at 2 and 12 weeks after operation. After overnight fasting, blood glucose was measured in conscious rats at 0, 30, 60, 120, and 180 min after intraperitoneal injection of human insulin (0.5 IU/kg).
Serum Insulin, GLP-1, TBAs, and Lipid Profiles
At 2 and 12 weeks postoperatively, the rats were fasted overnight and then orally administrated with 20 % of glucose (1 g/kg). At baseline, 15, 30, 60, and 120 min after glucose gavage, blood samples were collected from the retrobulbar venous plexus of sedative rats into chilled EDTA tubes containing a dipeptidyl peptidase IV inhibitor. After centrifugation (3000 rpm) at 4 °C for 15 min, the supernatant was immediately collected.
Aliquots of fasting serum samples were immediately analyzed for TBAs and lipid profiles using an automatic biochemical analyzer (Hitachi, Japan). The rest samples were stored at −80 °C for future analysis. Serum insulin and total GLP-1 concentration in response to oral glucose administration were measured by enzyme-linked immunosorbent methods (Millipore, USA).
Statistical Analysis
All quantitative data were reported as mean ± standard deviation (SD). Areas under the curves (AUC) for OGTT (AUCOGTT) and ITT (AUCITT) were calculated by trapezoidal integration. To test for the differences between groups at a specific time point, one-way analysis of variance (ANOVA) followed by Bonferroni post hoc comparisons was used; To compare the global insulin and GLP-1 concentration after glucose gavage between groups, mixed model ANOVA followed by Bonferroni post hoc comparisons was used. All statistical calculations were performed using SPSS version 19.0, and P < 0.05 indicates significant difference.
Results
There were ten rats in each experimental group preoperatively. When the study was ended at 12 weeks after operation, the number of rats alive in sham, DJA, DJB, and LDJB groups were 9, 8, 8, and 9, respectively. The causes of death included diabetes complications (n = 1), anastomotic leakage (n = 4), and intestinal obstruction (n = 1).
Body Weight and Food Intake
As shown in Fig. 2, there was no significant difference in body weight and daily food intake between the four groups both preoperatively and postoperatively. Because of perioperative food restriction and surgical and anesthetic stresses, the body weight of all groups minimized at 1 week postoperatively and almost restored to their preoperative values at 2 weeks postoperatively (Fig. 2a).
Body weight and food intake of rats. a Body weight of rats before and after operation. b Daily food intake of rats before and after operation. No significant difference was detected in both body weight and daily food intake between sham, DJA, DJB, and LDJB groups preoperatively and at any measured time points postoperatively
Effects of Surgeries on Glucose Homeostasis
There was no significant difference in AUCOGTT between groups preoperatively. DJA, DJB, and LDJB groups all exhibited better glucose tolerance than the sham group postoperatively. Notably, the AUCOGTT of DJB and LDJB groups were both statistically lower than that of DJA group after operation. Though LDJB further shortened the distance between duodenal papilla and terminal ileum by 15 cm in comparison with DJB, we observed no difference in AUCOGTT between the two groups (Fig. 3a).
Effects of surgeries on glucose tolerance and insulin tolerance. a AUCOGTT of rats preoperatively and at 2 and 12 weeks postoperatively. b AUCITT of rats preoperatively and at 2 and 12 weeks postoperatively. *P < 0.05 vs. sham group by one-way ANOVA; #P < 0.05 vs. DJA group by one-way ANOVA. AUC OGTT area under the curve for OGTT test, AUC ITT area under the curve for ITT test
As shown in Fig. 3b, the values of AUCITT were similar between groups preoperatively. At 2 and 12 weeks postoperatively, DJA, DJB, and LDJB groups all exhibited lower values of AUCITT than the sham group, indicating improved systemic insulin resistance. Unlike the differential improvements in glucose tolerance, DJA, DJB, and LDJB groups showed comparable values of AUCITT postoperatively.
Effects of Surgeries on Glucose-Stimulated Insulin and GLP-1 Secretion
In order to verify whether augmented insulin secretion contributes to the improved glucose tolerance after surgeries, we measured the serum insulin concentration after an oral glucose load at 2 and 12 weeks postoperatively. Although DJA, DJB, and LDJB groups experienced better glucose control than the sham group, we did not detect significantly increased serum insulin in these three groups (Fig. 4a, b).
Serum insulin and GLP-1 secretion in response to oral glucose gavage. a, b Serum insulin concentration after an oral glucose administration (1 g/kg) at 2 and 12 weeks after operation. c, d Serum GLP-1 concentration after an oral glucose administration (1 g/kg) at 2 and 12 weeks postoperatively. The illustrations in the rectangles indicate significant differences in global GLP-1 concentration between groups by mixed model ANOVA. *P < 0.05 vs. sham group by one-way ANOVA; #P < 0.05 vs. DJA group by one-way ANOVA
At 2 weeks postoperatively, the LDJB group exhibited markedly higher global and peak GLP-1 concentration than the sham and DJA groups. And, the DJB group showed higher GLP-1 than the two groups at 15 min after glucose gavage. As a procedure not changing biliopancreatic flow, DJA did not result in elevated serum GLP-1 (Fig. 4c).
At 12 weeks postoperatively, the DJB group exhibited statistically higher global GLP-1 concentration than the sham group and higher peak GLP-1 concentration than the sham and DJA groups. The LDJB group displayed both higher global and peak GLP-1 concentration than the sham and DJA groups. GLP-1 also trended to increase in the DJA group; however, it did not reach statistical difference (Fig. 4d). We detected no statistical difference in GLP-1 concentration between DJB and LDJB groups at both 2 and 12 weeks postoperatively (Fig. 4c, d).
Effects of Surgeries on Fasting Serum TBAs
At 2 and 12 weeks after operation, the DJA group displayed similar fasting serum TBAs to the sham group, while DJB and LDJB groups exhibited significantly higher fasting serum TBAs than both sham and DJA groups (Fig. 5).
Effects of Surgeries on Fasting Serum Lipid Profiles
Fasting serum lipid profiles were tested at 12 weeks after operation. The LDJB group demonstrated statistically lower serum cholesterol (CHO) than the sham group. DJA, DJB, and LDJB groups all displayed decreased fasting serum triglycerides (TGs) and free fatty acids (FFAs) compared with the sham group (Fig. 6).
Discussion
Gastric bypass surgeries could achieve profound amelioration of T2DM [20, 21]. The anti-diabetic mechanisms not only include postoperative calorie restriction and weight loss but also involve weight-independent effects exerted by anatomical and physiological alterations of small intestine postoperatively [22]. “Foregut hypothesis” and “hindgut hypothesis” are two prevailing theories to elucidate the weight-independent anti-diabetic mechanisms. The foregut hypothesis suggests that exclusion of proximal intestine from contact with ingested nutrients prevents the secretion of an undefined signal that promotes insulin resistance and diabetes [4]. While the hindgut hypothesis posits that expedited nutrient transits to the distal gut may benefit glucose homeostasis by increasing GLP-1 secretion [23]. In this study, we established DJA and LDJB on the basis of DJB to alter the drainage path of biliopancreatic juice. These three procedures excluded the same length of proximal intestine and identically expedited nutrients flow to the distal gut. This design enabled us to investigate the additional roles of biliopancreatic juice diversion in diabetes control after DJB beyond the classical foregut hypothesis and hindgut hypothesis.
Compared with sham operation, DJA, DJB, and LDJB surgeries all dramatically improved glucose tolerance in the diabetic rats independently of weight loss and food restriction. Rubino et al. once performed a procedure similar to DJA to verify the foregut hypothesis and proved it effective in glycemic control [4]. And, our study provided further evidence that the glucose-lowering effect of DJA was preserved but mildly attenuated in comparison with DJB and LDJB. Though LDJB further expedited biliopancreatic flow to the distal gut than DJB, we found no difference in AUCOGTT between the two groups. However, if LDJB was performed by anastomosing the biliopancreatic limb to the alimentary limb at 10 cm proximal to the ileocecal valve, it would produce better anti-diabetic effects than the conventional DJB [24]. Based on the above findings, we hypothesize that expedited transits of biliopancreatic juice to the lower intestine might partly contribute to the metabolic outcomes of DJB.
GLP-1 is an incretin hormone secreted from intestinal endocrine L cells, which are mainly located in the epithelium of distal ileum and colon [25]. GLP-1 regulates glucose homeostasis via multiple ways, such as stimulating insulin secretion, suppressing glucagon secretion, and promoting proliferation and inhibiting apoptosis of β cells [26]. Nutrient ingestion has been regarded as the primary physiologic stimulus for GLP-1 secretion [27]. While recently, BAs are also proved capable of stimulating GLP-1 secretion by activating the TGR5 receptors [12, 28]. And, intrajejunal taurocholic acid infusion could increase plasma GLP-1 response via a glucose-dependent manner [29]. Kohli et al. found that diverting bile from common bile duct to jejunum with an artificial catheter increased postprandial GLP-1 concentration in diet-induced obese rats [30]. Consistent with their findings, our study demonstrated that DJB and LDJB-operated animals displayed higher glucose-stimulated GLP-1 concentration than the sham and DJA groups postoperatively. Because of the anatomical changes after DJB and LDJB, a portion of bile might progress down the biliopancreatic limb to the lower intestine before mixed with ingested nutrients, thus leading to increased availability of undiluted BAs in the distal intestine lumen with the potential to stimulate GLP-1 release [31]. Other segments of intestine might also mediate the GLP-1 elevation after surgeries, as L cells are widely distributed throughout the gastrointestinal tract [25]. Though DJA did not alter BA flow, GLP-1 still trended to increase in that group at 12 weeks after operation, which might be attributed to premature delivery of ingested nutrients to the distal intestine. Taken together, we hypothesize that accelerated transits of both BAs and nutrients to the distal gut may synergistically contribute to the increased GLP-1 after DJB.
In DJB and LDJB groups, elevated serum GLP-1 was not paralleled by increased insulin secretion. Likewise, in Goto-Kakizaki (GK) diabetic rats, serum insulin was also unchanged shortly after DJB [19, 32, 33] but was markedly increased at 24 weeks after operation [19]. On the contrary, DJB-operated obese Zucker rats exhibited increased GLP-1 while decreased serum insulin at 1 month after operation [2]. These findings suggest that insulin changes after DJB are confusing, which may vary in different rat models or at different postoperative periods, and are not necessarily paralleled with serum GLP-1 levels. In our study, DJA, DJB, and LDJB groups all displayed comparable insulin levels to the sham group postoperatively, which has two implications: First, the glycemic control early after these surgeries was not dependent on augmented insulin secretion but dependent on improved insulin sensitivity, as evidenced by lower values of AUCITT; second, altered biliopancreatic juice flow may not contribute to the improved insulin resistance after surgeries. Possible explanations why DJA, DJB, and LDJB comparably improved insulin sensitivity might include that they resulted in similar postoperative FFA concentration, they excluded the same length of foregut, and/or they identically expedited nutrient flow to the distal gut.
Our study demonstrated that BAs were increased after DJB and LDJB while not after DJA. Elevated BAs were also observed after other kinds of metabolic surgeries including RYGB [6, 34] and IT [7, 35]. More recently, accumulating evidences point to an important role of BAs in mediating systemic glucose, lipid, and energy homeostasis. Specifically, BAs could inhibit the expression of multiple genes involved in gluconeogenesis [10], decrease serum triglycerides and prevent hepatic fat accumulation [11], and increase energy expenditure in brown adipose tissues [36]. So, the higher circulating BAs might partly explain why DJB and LDJB surgeries showed better anti-diabetic effects than DJA. Though BAs are also capable of preventing diet-induced weight gain [36], the higher serum BA concentration was not accompanied by corresponding lower body weight in DJB and LDJB-operated rats.
BAs are synthesized from cholesterol in hepatocytes, upon secreted into intestine lumen, about 95 % of BAs are reabsorbed at the terminal ileum and then transported to liver [9]. Incomplete clearance by the liver would result in spillover of small amounts of BAs into the systemic circulation [37], and the circulating BA concentration is well correlated with that in the portal vein [38]. The fact that BAs were elevated after DJB and LDJB while not after DJA implies a link between altered biliopancreatic flow and increased serum BAs. Animal studies on IT surgery provided surrogate evidence that premature delivery of bile to the interposed ileum resulted in early reabsorption of BAs and short-circuited enterohepatic BA recycling [35]. In addition, postoperative changes in gut motility and intestinal flora might also contribute to increased BA reuptake [6]. And, the elevated serum BAs after metabolic surgeries might not result from increased BA production, as the genes responsible for BA biosynthesis including Cyp7α1, Cyp8β1, Cyp27α1, and Cyp7β1 are all downregulated after IT surgery [39].
We have to admit that our study has some limitations. First, based on our results, we can only speculate that expedited biliopancreatic flow to the distal gut contributed to the diabetes control after DJB, while we cannot figure out whether it was merely mediated by BAs or also mediated by other constituents in the biliopancreatic juice. Second, this study did not provide detailed information on the intrinsic mechanisms responsible for the elevated serum BAs after DJB, which will be investigated in our future studies.
In summary, our study demonstrated that DJA, DJB, and LDJB surgeries could all achieve rapid and dramatic improvements in glucose tolerance and insulin sensitivity independently of weight loss and food restriction. As procedures that can expedite biliopancreatic flow to the lower intestine, DJB and LDJB surgeries resulted in better glucose tolerance, higher fasting serum TBAs, and higher postprandial GLP-1 than the DJA operation. DJA, DJB, and LDJB surgeries did not differ from each other in alleviating systemic insulin resistance and regulating insulin secretion. Our study suggests that expedited biliopancreatic flow to the distal gut may benefit the glycemic control after DJB by increasing serum GLP-1 and TBAs.
References
Rubino F, Marescaux J. Effect of duodenal-jejunal exclusion in a non-obese animal model of type 2 diabetes: a new perspective for an old disease. Ann Surg. 2004;239(1):1–11.
Jiao J, Bae EJ, Bandyopadhyay G, et al. Restoration of euglycemia after duodenal bypass surgery is reliant on central and peripheral inputs in Zucker fa/fa rats. Diabetes. 2013;62(4):1074–83.
Jurowich CF, Rikkala PR, Thalheimer A, et al. Duodenal-jejunal bypass improves glycemia and decreases SGLT1-mediated glucose absorption in rats with streptozotocin-induced type 2 diabetes. Ann Surg. 2013;258(1):89–97.
Rubino F, Forgione A, Cummings DE, et al. The mechanism of diabetes control after gastrointestinal bypass surgery reveals a role of the proximal small intestine in the pathophysiology of type 2 diabetes. Ann Surg. 2006;244(5):741–9.
Kindel TL, Yoder SM, Seeley RJ, et al. Duodenal-jejunal exclusion improves glucose tolerance in the diabetic, Goto-Kakizaki rat by a GLP-1 receptor-mediated mechanism. J Gastrointest Surg. 2009;13(10):1762–72.
Patti ME, Houten SM, Bianco AC, et al. Serum bile acids are higher in humans with prior gastric bypass: potential contribution to improved glucose and lipid metabolism. Obesity (Silver Spring). 2009;17(9):1671–7.
Cummings BP, Bettaieb A, Graham JL, et al. Bile-acid-mediated decrease in endoplasmic reticulum stress: a potential contributor to the metabolic benefits of ileal interposition surgery in UCD-T2DM rats. Dis Model Mech. 2013;6(2):443–56.
Han H, Hu C, Wang L, et al. Duodenal-jejunal bypass surgery suppresses hepatic de novo lipogenesis and alleviates liver fat accumulation in a diabetic rat model. Obes Surg. 2014;24(12):2152–60.
Houten SM, Watanabe M, Auwerx J. Endocrine functions of bile acids. EMBO J. 2006;25(7):1419–25.
Ma K, Saha PK, Chan L, et al. Farnesoid X receptor is essential for normal glucose homeostasis. J Clin Invest. 2006;116(4):1102–9.
Watanabe M, Houten SM, Wang L, et al. Bile acids lower triglyceride levels via a pathway involving FXR, SHP, and SREBP-1c. J Clin Invest. 2004;113(10):1408–18.
Thomas C, Gioiello A, Noriega L, et al. TGR5-mediated bile acid sensing controls glucose homeostasis. Cell Metab. 2009;10(3):167–77.
Schauer PR, Burguera B, Ikramuddin S, et al. Effect of laparoscopic Roux-en Y gastric bypass on type 2 diabetes mellitus. Ann Surg. 2003;238(4):467–84. discussion 84–5.
Wang TT, Hu SY, Gao HD, et al. Ileal transposition controls diabetes as well as modified duodenal jejunal bypass with better lipid lowering in a nonobese rat model of type II diabetes by increasing GLP-1. Ann Surg. 2008;247(6):968–75.
Buchwald H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122(3):248–56. 3.
Eissele R, Goke R, Willemer S, et al. Glucagon-like peptide-1 cells in the gastrointestinal tract and pancreas of rat, pig and man. Eur J Clin Investig. 1992;22(4):283–91.
Srinivasan K, Viswanad B, Asrat L, et al. Combination of high-fat diet-fed and low-dose streptozotocin-treated rat: a model for type 2 diabetes and pharmacological screening. Pharmacol Res. 2005;52(4):313–20.
Liu SZ, Sun D, Zhang GY, et al. A high-fat diet reverses improvement in glucose tolerance induced by duodenal-jejunal bypass in type 2 diabetic rats. Chin Med J. 2012;125(5):912–9.
Liu S, Zhang G, Wang L, et al. The entire small intestine mediates the changes in glucose homeostasis after intestinal surgery in Goto-Kakizaki rats. Ann Surg. 2012;256(6):1049–58.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
Pories WJ, Swanson MS, MacDonald KG, et al. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg. 1995;222(3):339–50. discussion 50–2.
Thaler JP, Cummings DE. Minireview: hormonal and metabolic mechanisms of diabetes remission after gastrointestinal surgery. Endocrinology. 2009;150(6):2518–25.
Knop FK. Resolution of type 2 diabetes following gastric bypass surgery: involvement of gut-derived glucagon and glucagonotropic signalling? Diabetologia. 2009;52(11):2270–6.
Zhang SY, Sun XJ, Zheng JB, et al. Preserve common limb in duodenal-jejunal bypass surgery benefits rats with type 2-like diabetes. Obes Surg. 2014;24(3):405–11.
Baggio LL, Drucker DJ. Biology of incretins: GLP-1 and GIP. Gastroenterology. 2007;132(6):2131–57.
Drucker DJ. The role of gut hormones in glucose homeostasis. J Clin Invest. 2007;117(1):24–32.
Brubaker PL. The glucagon-like peptides: pleiotropic regulators of nutrient homeostasis. Ann N Y Acad Sci. 2006;1070:10–26.
Parker HE, Wallis K, le Roux CW, et al. Molecular mechanisms underlying bile acid-stimulated glucagon-like peptide-1 secretion. Br J Pharmacol. 2012;165(2):414–23.
Wu T, Bound MJ, Standfield SD, et al. Effects of taurocholic acid on glycemic, glucagon-like peptide-1, and insulin responses to small intestinal glucose infusion in healthy humans. J Clin Endocrinol Metab. 2013;98(4):E718–22.
Kohli R, Setchell KD, Kirby M, et al. A surgical model in male obese rats uncovers protective effects of bile acids post-bariatric surgery. Endocrinology. 2013;154(7):2341–51.
Pournaras DJ, Glicksman C, Vincent RP, et al. The role of bile after Roux-en-Y gastric bypass in promoting weight loss and improving glycaemic control. Endocrinology. 2012;153(8):3613–9.
Salinari S, le Roux CW, Bertuzzi A, et al. Duodenal-jejunal bypass and jejunectomy improve insulin sensitivity in Goto-Kakizaki diabetic rats without changes in incretins or insulin secretion. Diabetes. 2014;63(3):1069–78.
Speck M, Cho YM, Asadi A, et al. Duodenal-jejunal bypass protects GK rats from {beta}-cell loss and aggravation of hyperglycemia and increases enteroendocrine cells coexpressing GIP and GLP-1. Am J Physiol Endocrinol Metab. 2011;300(5):E923–32.
Steinert RE, Peterli R, Keller S, et al. Bile acids and gut peptide secretion after bariatric surgery: a 1-year prospective randomized pilot trial. Obesity (Silver Spring). 2013;21(12):E660–8.
Kohli R, Kirby M, Setchell KD, et al. Intestinal adaptation after ileal interposition surgery increases bile acid recycling and protects against obesity-related comorbidities. Am J Physiol Gastrointest Liver Physiol. 2010;299(3):G652–60.
Watanabe M, Houten SM, Mataki C, et al. Bile acids induce energy expenditure by promoting intracellular thyroid hormone activation. Nature. 2006;439(7075):484–9.
Kuipers F, Groen AK. FXR: the key to benefits in bariatric surgery? Nat Med. 2014;20(4):337–8.
Angelin B, Bjorkhem I, Einarsson K, et al. Hepatic uptake of bile acids in man. Fasting and postprandial concentrations of individual bile acids in portal venous and systemic blood serum. J Clin Investig. 1982;70(4):724–31.
Mencarelli A, Renga B, D’Amore C, et al. Dissociation of intestinal and hepatic activities of FXR and LXRα supports metabolic effects of terminal ileum interposition in rodents. Diabetes. 2013;62(10):3384–93.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (no. 81270888/H0713, no. 81370496/H0308, no. 81300286/H0308), Natural Science Foundation of Shandong Province grants (no. ZR2009CM051), and the Taishan Scholar Foundation.
Conflict of Interest
We declare that all authors have no conflict of interest.
Statement of Informed Consent
Does not apply.
Statement of Human and Animal Rights
All applicable institutional and national guidelines for the care and use of animals were followed.
Author information
Authors and Affiliations
Corresponding author
Additional information
Haifeng Han and Lei Wang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Han, H., Wang, L., Du, H. et al. Expedited Biliopancreatic Juice Flow to the Distal Gut Benefits the Diabetes Control After Duodenal-Jejunal Bypass. OBES SURG 25, 1802–1809 (2015). https://doi.org/10.1007/s11695-015-1633-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-015-1633-7