Abstract
Background
Postoperative leaks are a dreaded complication after bariatric surgery (BS). Its treatment is based on nutritional support and sepsis control by antibiotics, collections drainage and/or prosthesis, and/or surgery.
Objectives
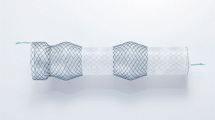
The aim of this study is to report our experience with coated self-expandable endoscopic stents (SEES) for leaks treatment.
Setting
This study was performed in a University Hospital, (censored).
Methods
We performed a retrospective analysis of our BS database from January 2007 to December 2013. All patients with leak after BS treated with SEES were included.
Results
We identified 29 patients; 17 (59 %) were women, with median age of 37 (19–65) years, and preoperative body mass index of 40 (28.7–56-6) kg/m2. Nineteen (65.5 %) patients had a sleeve gastrectomy and 10 (34.5 %) a Roux-en-Y gastric bypass. All patients had a leak in the stapler line. Median time from surgery to leak diagnosis was 7 (1–51) days, and SEES were installed 8 (0–104) days after diagnosis. Twenty-one (72 %) patients also had abdominal exploration. Median length of SEES use was 60 (1–299) days. Patients who had SEES as primary treatment (with or without simultaneous reoperation) had a shorter leak closure time (50 [6–112] vs 109 [60–352] days; p = 0.008). Twenty-eight (96.5 %) patients successfully achieved leak closure with SEES. There were 16 migrations in 10 (34 %) patients, 1 (3 %) stent fracture, 1 opening of the blind end of alimentary limb (3 %), and 5 patients (17 %) required a second stent due to leak persistence.
Conclusions
SEES is a feasible, safe, and effective management of post BS leaks, although patients may also require prosthesis revision and abdominal exploration. Primary SEES placement is associated with a shorter leak resolution time.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obesity is an epidemic disease with several related comorbidities and entails a higher risk of mortality [1] than observed in general population. Nowadays, bariatric surgery (BS) is recognized as the most effective treatment against obesity due to its good long-term weight control and high rate of remission or amelioration of comorbid diseases [2–4]. There are several surgical alternatives in the field of BS; currently, laparoscopic sleeve gastrectomy (SG) and laparoscopic Roux-en-Y gastric bypass (LRYGB) are the most frequent procedures performed around the world [5]. One of the most feared and life-threatening complications in BS are the postoperative leaks (PL), which are reported in the order of 1 to 5 % of the LRYGB and SG [6–8]. Leaks are a challenging problem because obese patients develop rapid and acute inflammatory response and they have diminished cardiopulmonary reserve. Moreover, diagnosis can be initially difficult and tachycardia may appear as the only early manifestation, thus surgeons must have a high index of suspicion for this complication [9]. Furthermore, there are no standardized protocols for leaks treatment, despite the fact that antibiotics, percutaneous drainages, or reoperation seems a reasonable approach to initially control intra-abdominal sepsis.
Coated self-expandable endoscopic stents (SEES) have been extensively used in general and oncologic surgery for treatment of esophageal obstructions, leaks, and fistulas [10–14], and its application in BS has been reported for the treatment of both acute and chronic leaks, as well as for anastomotic strictures with a high rate of success [8, 15]. Here, we report our experience with the use of coated SEES in the management of leaks after SG or LRYGB.
Materials and Methods
We performed a retrospective analysis of our prospectively collected electronic BS database from January 2007 to December 2013. All patients primarily operated in our center or referred, with a PL were included in the analysis. Demographic data, comorbid diseases, and type of BS were recorded. Leak location, determined by images as oral and iv contrast-enhanced computed tomography scan (CT) or upper gastrointestinal series (UGI), was detailed. Treatments were described in terms of the number of SEES used, need for SEES revision or replacement, and the need of surgical exploration. Only patients with an active stapler line leak demonstrated by radiological means were treated with SEES. All SEES were placed under radioscopic guidance in the operating room (OR) under general anesthesia, and an UGI series were performed one day after. If the leak was excluded, clear liquids were immediately started. All SEES were removed in the OR under sedation when the leak appeared to be healed according to surgeon’s criteria. The day after removal, UGI series were performed and if normal, soft oral feeding was started; conversely, if leak persisted, a new SEES was placed.
Median times from BS to leak diagnosis, from leak diagnosis to SEES placement, and from leak diagnosis to complete resolution were retrieved. In order to elucidate the role of the early management with SEES, patients were also subdivided in two groups: (1) those who were treated only with SEES or SEES plus concurrent surgery (primary SEES), and (2) those who were treated initially by surgery, in whom SEES was placed later (secondary SEES). Median time of leak resolution (leak diagnosis − leak resolution) was calculated and compared between groups.
Continuous variables are expressed as median (range), while categorical variables are expressed as number of cases (percentage). Statistical analysis was performed with the Statistical Package for Social Science (SPSS 20.0, Chicago, IL, USA) using the Mann–Whitney test for non-parametric variables and Fisher’s exact test for categorical ones. Statistical significance was considered when p value <0.05.
Results
Of 4746 patients who underwent LRYGB or SG in our center, 20 (0.44 %) developed a postoperative leak, without differences between procedures rates (LRYGB: 0.54 % vs SG: 0.31 %, p = 0.31). Of these patients, 17 received a covered SEES as part of leak treatment. There were also 12 referred patients who required SEES, totaling 29 cases. Demographic preoperative data is summarized in Table 1. Nineteen patients had a SG (including two conversions from lap banding) and 10 had a LRYGB. Leaks were diagnosed by UGI series or by an orally and intravenous contrast-enhanced abdominopelvic CT scan in 7 and 93 % of the cases, respectively. All leaks were located in the upper pole of the last stapler of both, LRYGB and SG.
According to the sleeve gastrectomy consensus for leak classification [16], we had 15 patients with acute leak, 13 with early leak, and only 1 patient with chronic leak.
Postoperative Leak Management
Besides the general medical management for sepsis control which included fluid resuscitation, iv wide spectrum antibiotics, intensive care unit management in some cases, and nutritional support, eight patients were treated only with SEES (5 SG and 3 LRYGB). Four patients had concurrent surgery with SEES placement (2 SG, 2 LRYGB), and 17 patients had at least one reoperation before the SEES placement (12 SG and 5 LRYGB, Table 1). Of note, no surgeries were required for collection drainage after SEES placement. In regards to stents type, all of them were fully covered. The length and diameter are detailed in Table 1.
Median time between BS and leak diagnosis was 7 (1–51) days, and median time between leak diagnosis and SEES placement was 8 (0–104) days. Median leak resolution time, measured from leak diagnosis to SEES removal, with normal UGI series confirming leak closure, was 82 (6–352) days. The median length of SEES use was 60 (1–299) days and 19 patients (65 %) had SEES in situ for more than 6 weeks, although 9 of them required prosthesis change during this period for reasons described below.
Regarding the timing of stent placement, when comparing the primary and secondary SEES installation, the primary SEES was associated with a significantly shorter leak resolution time as compared to the secondary SEES (primary: 50 [6–112] vs secondary: 109 [60–352] days, p = 0.008, Fig. 1).
Comparison of resolution time between primary and secondary SEES. SEES self-expandable endoscopic stent. Primary SEES: installed concurrently with reoperation or without it. Secondary SEES: installed after reoperation. Resolution time is expressed in median (range) of days. P value was obtained by Mann–Whitney test
Despite a long period for leak resolution in the secondary SEES group, the overall rate of resolution was 96 % for the entire series (28/29 patients). The only patient who did not resolve with SEES placement was a SG patient who initially received a SEES and healed her leak, but reopened 8 months later. She was treated with a second SEES successfully. Nevertheless, 3 years after surgery, the leak reopened again. A laparoscopic jejunostomy was performed for nutritional support and after sepsis management; a laparoscopic proximal gastrectomy with hand-sewn Roux-en-Y esophagojejunostomy was performed, with no further complications.
Self-Expandable Endoscopic Stent Performance
In this series, SEES achieved a high rate of leak resolution. Nevertheless, SEES were not exempt of complications. In fact, 16 patients required additional procedures besides SEES placing during their evolution. There were 16 migrations in 10 patients (34 %), 7 of which were treated with repositioning, 5 with installation of a second SEES and in 4 cases, prosthesis were removed without repositioning or replacement due to leak closure. There were five additional SEES replacement due to leak persistence after removal. Two patients required reoperation exclusively due to SEES complications: one SG patient had a prosthesis fracture and required a laparoscopic removal of the distal segment of the prosthesis that migrated to the jejunum, and one RYGB patient in whom the distal edge of the prosthesis opened the stapler line of the blind end of the alimentary limb. Prosthesis was removed by laparoscopy, the open limb was closed using silk stitches, and drains were placed near the leak and the alimentary blind end. Complications associated with SEES in each patient are detailed in Table 1.
Discussion
Currently, BS is recognized as the most effective treatment against obesity and its related comorbidities. Nevertheless, BS is not exempt of postoperative problems and leaks are one of the most feared and life-threatening complications. Despite the improvement in surgical devices such as laparoscopic staplers to perform safer BS and despite the experience gained through years, no surgeon is free of having a leak [17]. Probably the most important step in leak management is its early recognition and treatment, in order to prevent severe systemic inflammation [17, 18]. As mentioned above, there are no standardized protocols to treat this complication; therefore, besides the medical control of sepsis and the nutritional support, treatments are usually performed according to local experiences and what seems to be reasonable for each patient. This includes the non-surgical management, percutaneous image-guided drainage [19], endoscopic stents, reoperations, drains placement for collections management [20], and different combinations of them.
In our center, we do not routinely perform intraoperative nor postoperative leak assessment, since no study has demonstrated the usefulness of this practice [17, 21]. As widely known, leak diagnosis is based primarily on clinical signs as tachycardia, abdominal pain, and fever [22]. In these cases, we perform an orally and intravenous contrast-enhanced abdominopelvic CT scan, which has proven to be a very useful test for leak diagnosis [9], since besides demonstrating the leak itself, also can show the presence of intra-abdominal collections, which are generally indirect sign of leaks. We reserve UGI series, which sensitivity has been reported to vary between 22 and 75 % [23, 24], to patients with high suspicion of leak and a negative CT scan. It must be noted that both UGI and CT may be limited by patient positioning and inability to ingest oral contrast, and could result in false-negative results in one third of cases [17, 23]; therefore, high suspicion is the cornerstone when diagnosing this complication.
Endoscopic stents have been largely used in general and oncologic surgery for treatment of leaks and strictures [12, 13, 20, 25] and recently, SEES are also being increasingly used for treatment of post BS leaks [10, 11, 18, 26] with good results in terms of leak resolution. Here, we show our experience in the use of coated SEES in leaks treatment after SG and LRYGB. Nevertheless, the major flaw of our study is the absence of defined length of time for SEES use. In our series, each surgeon according to personal clinical judgment decided when to remove the prosthesis. Therefore, we are not able to make a recommendation regarding how long the prosthesis should be in situ. Fortunately, we had a high rate of leak resolution after SEES placement, without mortality related to leak per se or prosthesis complication. Notably, there was a significant shorter time of leak resolution when SEES was placed as the first choice of treatment (primary group).
As described above, endoscopic stents together with the simultaneous treatment of sepsis are becoming an attractive option in the management of post BS leaks due to its minimally invasive placement, low injury to patient, and early restoration of oral feeding. In our series, we observed 6 out of 29 patients who required a second SEES, 5 of them immediately after SEES removal, due to leak persistence, and 1 patient because of leak recurrence 8 months after SEES removal. Here, we show that placing a second SEES when leak persistence is found after removal is effective to achieve leak closure.
The main flaw of SEES is its high migration rate and need of prosthesis revision. Large series of leaks management with prosthesis after bariatric surgery have shown migration rates from 11 to 58 % [15, 27, 28], and other complications such as bleeding and prosthesis kinking. Here, we show a rate of 34 % of prosthesis migration, which is similar to previously reported data [9]. Recently, endoscopic stent anchoring with stitches or clips have been employed resulting in lesser migration rates [27, 29]. We have not anchored any SEES but certainly, it seems a promising alternative to prevent stent migration. Finally, adding two patients who required reoperation (stent fracture and opening of the blind end of the alimentary limb), we had a 41 % of total complications, a rate that is similar to others described in literature [15, 27, 28]. Regarding how long SEES must be in situ, several studies have suggested that they should not be placed longer than 6 weeks [9]. However, despite a long SEES use time in some cases (68 % of patients had the stent more than 6 weeks), we had no long-term esophageal strictures, and endoscopic removal was successfully achieved in all cases.
Conclusions
In summary, here, we show a large series of coated SEES for acute and early leak treatment after BS with good results in terms of leak resolution and morbidity rate similar to previously reported by other groups. Notably, the primary use of SEES was associated with a shorter length of leak resolution. Therefore, after prompt leak recognition in association with appropriate sepsis treatment with antibiotics, nutritional support, and collection drain, early SEES placement should be considered as a useful treatment for this complication.
References
Sjöström L, Narbro K, Sjöström CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357(8):741–52.
Sjöström L, Lindroos A-K, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351(26):2683–93.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes—3-year outcomes. N Engl J Med. 2014;370(21):2002–13.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013;23(4):427–36.
Lee S, Carmody B, Wolfe L, et al. Effect of location and speed of diagnosis on anastomotic leak outcomes in 3828 gastric bypass cases. J Gastrointest Surg. 2007;11(6):708–13.
Maher JW, Martin Hawver L, Pucci A, et al. Four hundred fifty consecutive laparoscopic Roux-en-Y gastric bypasses with no mortality and declining leak rates and lengths of stay in a bariatric training program. J Am Coll Surg. 2008;206(5):940–4. discussion 944–945.
Sakran N, Goitein D, Raziel A, et al. Gastric leaks after sleeve gastrectomy: a multicenter experience with 2,834 patients. Surg Endosc. 2013;27(1):240–5.
De Aretxabala X, Leon J, Wiedmaier G, et al. Gastric leak after sleeve gastrectomy: analysis of its management. Obes Surg. 2011;21(8):1232–7.
Spyropoulos C, Argentou M-I, Petsas T, et al. Management of gastrointestinal leaks after surgery for clinically severe obesity. Surg Obes Relat Dis Off J Am Soc Bariatr Surg. 2012;8(5):609–15.
Yimcharoen P, Heneghan HM, Tariq N, et al. Endoscopic stent management of leaks and anastomotic strictures after foregut surgery. Surg Obes Relat Dis Off J Am Soc Bariatr Surg. 2011;7(5):628–36.
Rajan PS, Bansal S, Balaji NS, et al. Role of endoscopic stents and selective minimal access drainage in oesophageal leaks: feasibility and outcome. Surg Endosc. 2014;28(8):2368–73.
Nguyen NT, Rudersdorf PD, Smith BR, et al. Management of gastrointestinal leaks after minimally invasive esophagectomy: conventional treatments vs. endoscopic stenting. J Gastrointest Surg Off J Soc Surg Aliment Tract. 2011;15(11):1952–60.
Sharma P, Kozarek R, Practice Parameters Committee of American College of Gastroenterology. Role of esophageal stents in benign and malignant diseases. Am J Gastroenterol. 2010;105(2):258–73. quiz 274.
Eubanks S, Edwards CA, Fearing NM, et al. Use of endoscopic stents to treat anastomotic complications after bariatric surgery. J Am Coll Surg. 2008;206(5):935–8. discussion 938–939.
Rosenthal RJ, International Sleeve Gastrectomy Expert Panel, Diaz AA, et al. International sleeve gastrectomy expert panel consensus statement: best practice guidelines based on experience of >12,000 cases. Surg Obes Relat Dis Off J Am Soc Bariatr Surg. 2012;8(1):8–19.
Clinical Issues Committee ASMBS. ASMBS guideline on the prevention and detection of gastrointestinal leak after gastric bypass including the role of imaging and surgical exploration. Surg Obes Relat Dis Off J Am Soc Bariatr Surg. 2009;5(3):293–6.
Simon F, Siciliano I, Gillet A, et al. Gastric leak after laparoscopic sleeve gastrectomy: early covered self-expandable stent reduces healing time. Obes Surg. 2013;23(5):687–92.
Pequignot A, Fuks D, Verhaeghe P, et al. Is there a place for pigtail drains in the management of gastric leaks after laparoscopic sleeve gastrectomy? Obes Surg. 2012;22(5):712–20.
Tan JT, Kariyawasam S, Wijeratne T, et al. Diagnosis and management of gastric leaks after laparoscopic sleeve gastrectomy for morbid obesity. Obes Surg. 2010;20(4):403–9.
Lee SD, Khouzam MN, Kellum JM, et al. Selective, versus routine, upper gastrointestinal series leads to equal morbidity and reduced hospital stay in laparoscopic gastric bypass patients. Surg Obes Relat Dis Off J Am Soc Bariatr Surg. 2007;3(4):413–6.
Csendes A, Braghetto I, León P, et al. Management of leaks after laparoscopic sleeve gastrectomy in patients with obesity. J Gastrointest Surg Off J Soc Surg Aliment Tract. 2010;14(9):1343–8.
Gonzalez R, Sarr MG, Smith CD, et al. Diagnosis and contemporary management of anastomotic leaks after gastric bypass for obesity. J Am Coll Surg. 2007;204(1):47–55.
Madan AK, Stoecklein HH, Ternovits CA, et al. Predictive value of upper gastrointestinal studies versus clinical signs for gastrointestinal leaks after laparoscopic gastric bypass. Surg Endosc. 2007;21(2):194–6.
Babor R, Talbot M, Tyndal A. Treatment of upper gastrointestinal leaks with a removable, covered, self-expanding metallic stent. Surg Laparosc Endosc Percutan Tech. 2009;19(1):e1–4.
El Mourad H, Himpens J, Verhofstadt J. Stent treatment for fistula after obesity surgery: results in 47 consecutive patients. Surg Endosc. 2013;27(3):808–16.
Swinnen J, Eisendrath P, Rigaux J, et al. Self-expandable metal stents for the treatment of benign upper GI leaks and perforations. Gastrointest Endosc. 2011;73(5):890–9.
Iqbal A, Miedema B, Ramaswamy A, et al. Long-term outcome after endoscopic stent therapy for complications after bariatric surgery. Surg Endosc. 2011;25(2):515–20.
Sharaiha RZ, Kumta NA, Doukides TP, et al. Esophageal Stenting With Sutures: Time to Redefine our Standards? J Clin Gastroenterol. 2014.
Conflict of Interest
The authors declare that they have no conflict of interest. For this type of study, formal consent is not required.
Funding
There are no funding sources involved.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Quezada, N., Maiz, C., Daroch, D. et al. Effect of Early Use of Covered Self-Expandable Endoscopic Stent on the Treatment of Postoperative Stapler Line Leaks. OBES SURG 25, 1816–1821 (2015). https://doi.org/10.1007/s11695-015-1622-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-015-1622-x