Abstract
Background
Leak or stenosis following laparoscopic Roux-en-Y gastric bypass (LRYGB) can lead to a major morbidity. We aim to evaluate whether the routine use of intraoperative endoscopy (IOE) can reduce this morbidity.
Methods
All cases of LRYGB in 2009–2014 were reviewed. In all cases, we perform an IOE. If IOE shows a leak, the area of the leak is re-enforced and IOE is repeated. If the leak persisted, a feeding tube and drains are placed.
Results
During the study period, we performed 342 LRYGB cases. Primary LRYGB represented 82 % (282/342). Average BMI 48 kg/m2 (range was 35–92) and females represented 76 % (261/342). Our clinical leak rate was 3/342 (0.88 %) in LRYGB (0.4 % in primary and 3.3 % in revisional LRYGB). IOE showed a positive air leak test in six LRYGB cases (1.75 %). We were able to achieve a negative leak test after re-enforcement in 5/6 (83 %) cases, and all those patients had no clinical leak. The patient with persistent air leak test had a clinical leak after surgery. IOE was negative in 336 LRYGB cases and we had two clinical leaks in this group (0.59 %). Our stenosis rate at the gastrojejunostomy was 3/342 (0.88 %). The positive predictive value (PPV) of the performing IOE to detect leaks in LRYGB was 75 % while the negative predictive value was 99.5 %.
Conclusions
Routine IOE has led to a change in the operative strategy and could be one reason for our low leak and stenosis in laparoscopic Roux-en-Y gastric bypass.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery has been acknowledged as an acceptable long-term approach for morbid obesity, and LRYGB has been the golden standard for bariatric surgery for over 40 years [1, 2]. However, LRYGB is associated with a recognizable morbidity and mortality and carries a higher risk than laparoscopic sleeve gastrectomy (LSG) and laparoscopic adjustable gastric banding (LAGB) [3]. Since the introduction of laparoscopic surgery, the morbidity and mortality of bariatric surgery has decreased several folds [4]. In addition to performing the surgery laparoscopically, surgeons perform several other techniques to detect complications early and reduce postoperative complications. These techniques include placing drains or performing a methylene blue leak test intraoperatively, performing postoperative radiographic studies routinely, checking drain amylase level, and keeping patients on nil per os (NPO) for at least 24 h after surgery [5–9]. At BMI Abu Dhabi, we have published a comparative study of our outcomes to the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) bariatric programs. In that comparison, our bariatric surgery outcomes in resectional surgeries including LRYGB and LSG compare well to the ACS NSQIP bariatric surgery programs [10]. In addition, our sepsis after surgery signifying a leak rate and mortality were found to be lower than other ACS NSQIP bariatric surgery programs [10]. We hypothesized that the routine use of IOE to detect leaks and stenosis in LRYGB could be one of the reasons for our leak and stenosis outcomes after LRYGB.
Methods
We reviewed all our prospectively collected consecutive cases of LRYGB done between June 2009 and February 2014. This is a consecutive series including all our primary and revisional LRYGB cases, and no cases were excluded from this analysis.
Preoperative Measures
All patients received sequential compression devices, intravenous antibiotics (cefazolin), dexamethasone, metoclopramide, and subcutaneous heparin prior to induction of general anesthesia. We place an indwelling urinary catheter routinely and decompress the stomach following endotracheal intubation. All patients are endotracheally intubated in the head up (ramp) position.
Operative Technique
Our technique of LRYGB has been described previously [12]. In summary, we perform an antecolic antegastric gastric bypass, with a 100–150-cm Roux limb, a 30–50-cm biliopancreatic limb, and a double-layer hand sewn gastrojejunostomy. The gastric pouch volume is approximately 15–20 ml. We start our pouch creation by measuring 4 cm from the gastroesophageal (GE) junction near on the lesser curve of the stomach. Next, a window is created on the lesser curve of the stomach 4 cm from the GE junction. In primary LRYGB cases, we use blue cartridges of Echelon 60 (Ethicon J&J) for our transection and for revisional LRYGB we use green cartridges. After the first transverse transection, then we place a 34-Fr tube and we transect the pouch vertically flush to the tube avoiding to staple close to the esophagus with two staple firings to completely separate the pouch from the remnant of the stomach. The gastrojejunostomy is performed in two layers of 3–0 Vicryl suture (Ethicon J&J). The 34-Fr tube is passed through the anastomosis before completion of the last layer. Once the anastomosis is completed, then we remove the tube and we clamp the Roux limb with an atraumatic grasper and place an adult 32-Fr endoscope down to the pouch with very little insufflation (we do not use CO2). Once the endoscope is at the pouch level, then we fill the upper abdomen with saline laparoscopically while the Roux limb is clamped; we insufflate at high pressure and we traverse the gastrojejunostomy. We do not place drains routinely; and in all cases, we perform intraoperative endoscopy at the end of surgery to check for leak, bleeding or stenosis. All intraoperative endoscopies were done using an adult 32-Fr endoscope by one of our two bariatric surgeons at the end of surgery and this involves direct visualization of the anastomosis and the staple line for any evidence of bleeding and performing an air leak test. On average, it takes approximately 5 min to perform the intraoperative endoscopy. If the intraoperative endoscopy did not show evidence of bleeding, stenosis, or leak, then no drains were placed, and the patients are started on clear liquids once they are awake; we omitted doing a postoperative upper GI (UGI) study the next day after surgery. In contrast, when a persistent and not transient positive air leak test is detected either at the pouch staple line or at the gastrojejunostomy, then the area of the leak is re-enforced with sutures, an omental patch, and fibrin glue, and a drain is placed and the air leak test is repeated. All patients with a positive leak test had drains placed intraoperatively and underwent a postoperative UGI study on the first day after surgery and are kept on NPO until the upper GI study is done.
Postoperative Management
We do not place drains or perform postoperative UGI studies routinely; we allow patients to have clear liquids once they are awake. In contrast, in patients with a positive intraoperative endoscopy, a drain was placed intraoperatively and they were kept on NPO, and an UGI study was done on postoperative day 1.
Results
During the study period we performed 342 LRYGB cases. Primary LRYGB represented 82 % (282/342). Average BMI 48 kg/m2 (range was 35–92) and females represented 76 % (261/342). We were able to perform an intraoperative endoscopy in all patients. Our clinical leak rate was 3/342 (0.88 %) in LRYGB (0.4 % in primary and 3.3 % in revisional LRYGB). Our stenosis rate at the gastrojejunostomy was 3/342 (0.88 %).
In regard to detecting leaks, IOE showed a persistent positive air leak test in six LRYGB cases (1.75 %). These patients did not have a transient leak, and the leak was not through the sutures. In five of these patients, the positive leak test was from the anastomosis, and we were able to achieve a negative leak test after re-enforcement using omental patch and Fibrin sealant in 5/6 (83 %) LRYGB cases; all patients with a negative leak test following a positive leak test had no clinical leak after surgery. In the patient with persistent positive air leak test, the leak was from the pouch itself, and the tissue was very friable; drains and a gastrostomy tube were placed at the time of surgery. The patient had a clinical leak after surgery and was treated conservatively. IOE was negative in 336 LRYGB cases, and we had two clinical leaks in this group (0.59 %). Both patients needed re-operation to place drains and a gastrostomy tube and to control sepsis, and they recovered without further complications; both patients did not have a stenosis detected postoperatively and healed in less than 3 weeks after re-operation.
In regards to detecting stenosis after LRYGB, we had one patient with a stenosis intraoperatively after LRYGB. This patient was a conversion of LAGB to LRYGB, and after the completion of surgery we performed IOE. On IOE, we were not able to enter the pouch easily at the end of the surgery despite a complete laparoscopic dissection. It was noted that this patient had a kink at the lower esophagus that we did not appreciate laparoscopically and was only detected on IOE. Further dissection revealed adhesions between the edge of the liver and the esophagus. Once these adhesions were released, then we were able to enter the gastric pouch easily. Our clinical stenosis rate at the gastrojejunostomy was 3/342 (0.88 %); all these patients required endoscopic dilatation after LRYGB. Our overall length of stay in LRYGB is 2.6 days.
The positive predictive value (PPV) of the performing IOE to detect leaks in LRYGB was 75 % while the negative predictive value was 99.5 %.
In regard to other complications after LRYGB, we had no cases of acute bowel obstruction either due to acute internal hernia or port site hernia. Our overall internal hernia rate is 0 % as well. Our risk of bleeding requiring blood transfusion is 2.3 %, and two patients (0.2 %) required re-operation for bleeding. Both patients were treated laparoscopically, and no bleeding site was found. Also, intraperitoneal hematoma was evacuated. Our venous thrombi-embolism rate was 2 %.
Discussion
The results of this study show that routine IOE at the end of LRYGB has led to a change in the operative strategy because IOE detected a persistent positive leak test or positive stenosis. In addition, we were able to perform several intraoperative maneuvers that led to a negative leak test or resolution of stenosis on repeat IOE. We believe this approach can help in lowering the leak and stenosis rates after LRYGB. We were able to perform IOE in all patients, and we have not found IOE in the supine position difficult.
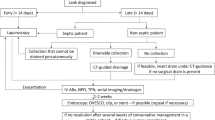
Anastomotic or staple line leaks are the most common feared complications following LRYGB and carry a high rate of morbidity and perioperative mortality between 0.5 and 1.5 % of patients. In addition, early detection of leaks may lead to a decrease in the consequences of a leak [11]. Bariatric surgeons have used many strategies to enhance the early detection of leaks including placing drains intraoperatively, checking drain amylase level, and routinely performing postoperative radiographic UGI studies [6–9]. These strategies are helpful to discover leaks in the early postoperative period but have no preventive effect on the occurrence of leaks. In addition, some strategies like UGI studies may not detect leaks and lead to a longer length of stay, and the utility of UGI studies have been challenged [6, 7, 13]. Furthermore, even when these methods detect leaks in the postoperative period, these patients might need another operation to control sepsis or establish an enteral feeding route.
Because of the complications associated with leaks can be devastating, we believe that every effort to prevent their occurrence is worthwhile. Hence, by performing an IOE and detecting leaks intraoperatively, we could change the operative strategy and potentially prevent sepsis or at least establish an enteral feeding route for those patients who are at a high risk for postoperative clinical leaks. For example, in our cases when a leak is found during LRYGB, the persistent positive leak was not through the sutures but rather at the gastrojejnostomy or the pouch staple line. In all these patients with a persistent positive leak test, we added re-enforcement sutures, drains, an omental patch, or placed a gastrostomy tube if the leak persisted. In addition, all patients with an intraoperative leak test are subjected to an UGI study on the first day after surgery and they are kept on NPO after surgery.
We feel that detecting leaks with IOE is better than methylene blue because the tissues are not stained once the leak is detected. In addition, we can repeat the IOE as many times as we need. Furthermore, there is no risk of aspiration of methylene blue with IOE. The use of IOE detects not only leaks but stenosis as well.
In general, we do not routinely perform UGI studies after surgery. Furthermore, routinely we do not place drains, and only revisional surgery patients or patients with a positive intraoperative leak test would have a drain placed. Hence, when we have a positive persistent leak test we deviate from our routine practice. This deviation includes placing a drain, possibly a gastrostomy tube, and performing an UGI study done on the first day after surgery, and these patients are kept on NPO after surgery. In our routine practice, we spare our patients from these extra steps and they are fed orally once they are awake which leads to a shorter length of stay. Our mean length of stay is 2.6 ± 1.8 days, which compares well with the published literature [10].
In our series, we had three patients with clinical leaks following LRYGB, two after revisional LRYGB, and one after primary LRYGB (0.4 % in primary and 3.3 % in revisional LRYGB). The first leak was a patient after conversion from LAGB to RYGB, the second was primary RYGB in a diabetic male patient, and the third was following conversion from Nissen fundoplication to LRYGB. Two of these patients had a negative IOE; these two leaks were not detected during IOE. Both patients presented these leaks within the first week after surgery and needed re-operation laparoscopically to place a gastrostomy feeding tube and drainage of the abdomen; they recovered without complications. The third patient with a clinical leak following conversion of a Nissen fundoplication to RYGB had a positive IOE with a persistent leak from the pouch and had friable gastric tissues.
We only place a gastrostomy feeding tube if there is a persistent leak on IOE despite intraoperative maneuvers similar to one of our clinical leak cases. It will not be reasonable or justifiable to place a gastrostomy feeding tube in all LRYGB cases due to the morbidity of the gastrostomy tubes themselves. In contrast, detecting which patients have an intraoperative leak test helps in tailoring the intraoperative and postoperative course for this particular high-risk group of patients and allows the surgical team to be more selective in placing enteral feeding tubes, placing drains, and ordering postoperative UGI studies.
The technique we used when we are faced with a positive persistent leak on IOE of over sewing with an omental patch using Fibrin sealant is similar to that used by others. Sapala et al. and others have shown that the clinical leak rate in resectional bariatric surgery can be reduced by certain intraoperative strategies like using Fibrin glue prophylactically at the time of gastrojejunostomy creation, buttressing material for the endoscopic staplers, or using omental patch to treat perforated ulcers after LRYGB have been described [14, 15].
Our leak rates after LRYGB compares well to the bariatric surgery programs of the American College of Surgeons National Surgical Quality Improvement Programs [3], and other published leak rates following LRYGB of 1.1 % [16]. In addition, Hadad et al., Champion et al., and others have shown similar results of lower leak rates after LRYGB by using IOE and changing the intraoperative strategy once a leak test is detected. One study looked into the role of routine intraoperative endoscopy in laparoscopic bariatric surgery and yielded successful results of identifying 34 correctable technical errors in a series of 825 laparoscopic bariatric procedures, 97 % of which were repaired successfully. Similarly, a couple of studies have shown the value of intraoperative endoscopy in LRYGB cases. Hadad et al. evaluated 2311 LRYGB cases and detected an intraoperative leak in 3.2 % of cases and after strategies to repair the leak the clinical leak rate was only 0.2 % [17–19].
Despite performing IOE, we did not detect two leak cases following LRYGB. In total, we had 336 negative leak tests on IOE. This is compatible with another series of IOE by Hadad et al. which showed that despite performing IOE and detecting leaks, one might still miss some patients who present with leak after surgery while they had a negative leak test. We cannot explain why these patients had a negative intraoperative leak test, but went on to have a clinical leak test. One explanation is that these were not technical leaks. For example, both these two patients needed re-operation for control of sepsis and to establish an enteral feeding by placing a gastrostomy tube. The positive predictive value (PPV) of the performing IOE to detect leaks in LRYGB was 75 % while the negative predictive value was 99.5 %.
In regard to detecting strictures or stenosis by IOE, we were able to achieve a low stenosis rate after LRYGB (3/342) 0.88 %. Our stenosis rate after LYRGB is comparable to the published rates of stenosis after LRYGB [21–25]. We believe that these results are in part due to the routine use of IOE and surgical technique. We were able to achieve these results by having an active strategy at the end of surgery to look for any evidence of stricture or stenosis in LRYGB. This active strategy allowed us to detect a kink due to adhesions from a previous LAGB near the esophagus in a revisional LRYGB. The kink was not appreciated laparoscopically and was only detected on IOE at the end of the surgery because we were not able to enter the LRYGB pouch easily. Detecting this finding intraoperatively and releasing the adhesions which allowed an easy passage of the endoscope into the LRYGB pouch on IOE allowed this patient to have a normal postoperative course.
Our stricture rate following LRYGB could be attributed to our surgical technique of hand sewn gastrojejunostomy and performing IOE at the end of surgery. Hand sewn anastomosis has a learning curve and is not commonly performed. In a survey done for all surgeons in Michigan by Fink et al. showed that hand sewn anastomosis was performed by only 18 % of surgeons while circular anastomosis was the most commonly performed technique by 66 % of surgeons [20]. The technique of gastrojejunostomy is an important factor in the incidence of postoperative stenosis following LRYGB. Circular stapled anastomosis, especially with 21 mm, has a higher stenosis rate than circular stapled gastrojejunal anastomosis with 25 mm. Linear, hand sewn, and circular gastrojejunostomy anastomosis with 25 mm EEA have comparable stenosis rates [21–25].
There was no significant added operational cost for performing IOE in our study. We started by sharing an endoscope from the endoscopy suites, and as we increased the volume of LRYGB cases performed, we started keeping the endoscope in the operating room at all times. In addition, we train our fellow and residents in performing IOE, and they gain experience during their training. Currently, our operating room is equipped with a mobile endoscopy tower so the endoscope and the expertise were available for our bariatric surgery team. In addition, on average, the intraoperative endoscopy takes approximately 5 min. Furthermore, we were able to perform intraoperative endoscopy in all our patients.
Our study has several limitations; it is a retrospective review of a prospectively maintained database single-center study. In addition, endoscopy is highly operator dependent and the expertise needs to be available within the surgical team to allow for flexibility in performing IOE, and the surgeon performing the endoscopy needs to be familiar with the anatomy of LRYGB. Furthermore, not all bariatric surgeons perform endoscopy at the end of surgery and many do not have the training or the availability of an endoscope in the operating room. Unless the surgeon performs the endoscopy, then a gastroenterologist needs to be available at the end of surgery, which might not be practical or possible at all times. The additional need of an expert from another specialty and the potential addition of equipment and costs may be limiting factors. To prove definitely the real value of performing IOE in LRYGB, another group of patients without IOE would be ideal. In addition, a randomized study with or without IOE including a large number of patients would be ideal.
Conclusion
The routine use of intraoperative endoscopy in laparoscopic Roux-en-Y gastric bypass (LRYGB) maybe one of the reasons for our low leak and stenosis rate. The cost and time spent in doing intra-operative endoscopy is justified to reduce rates of leak and stenosis and to reduce the length of stay after LRYGB.
References
Sjöström L, Narbro K, Sjöström CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357(8):741–52.
Adams TD, Gress RE, Smith SC, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357(8):753–61.
Hutter MM, Schirmer BD, Jones DB, et al. First report from the American College of Surgeons–Bariatric Surgery Center Network: laparoscopic sleeve gastrectomy has morbidity and effectiveness positioned between the band and the bypass. Ann Surg. 2011;254(3):410.
Nguyen NT, Masoomi H, Magno CP, et al. Trends in use of bariatric surgery, 2003–2008. J Am Coll Surg. 2011;213(2):261–6.
Maher JW, Martin Hawver L, Pucci A, et al. Four hundred fifty consecutive laparoscopic Roux-en-Y gastric bypasses with no mortality and declining leak rates and lengths of stay in a bariatric training program. J Am Coll Surg. 2008;206(5):940–4.
Sims TL, Mullican MA, Hamilton EC, et al. Routine upper gastrointestinal Gastrografin® swallow after laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2003;13(1):66–72.
Quartararo G, Facchiano E, Scaring S, et al. Upper gastrointestinal series after Roux en Y gastric bypass for morbid obesity: effectiveness in leakage detection. A Systematic Review of the Literature. Obes Surg. 2014 May 11.
Maher JW, Bakhos W, Nahmias N, et al. Drain amylase levels are an adjunct in detection of gastrojejunostomy leaks after Roux-en-Y gastric bypass. J Am Coll Surg. 2009;208(5):881–4.
Sensenig D, Jurgeleit H. The use of methylene blue solution to test for leaks in gastric bypass operations for morbid obesity. J Maine Med Assoc. 1980;71(8):234.
Nimeri A, Mohamed A, el Hassan E, et al. Are results of bariatric surgery different in the Middle East? Early experience of an international bariatric surgery program and an ACS NSQIP outcomes comparison. J Am Coll Surg. 2013;216(6):1082–8.
Fernandez Jr A, DeMaria E, Tichansky D, et al. Experience with over 3,000 open and laparoscopic bariatric procedures: multivariate analysis of factors related to leak and resultant mortality. Surg Endosc Interv Tech. 2004;18(2):193–7.
Dallal RM, Bailey L, Nahmias N. Back to basics—clinical diagnosis in bariatric surgery. Routine drains and upper GI series are unnecessary. Surg Endosc. 2007;21(12):2268–71.
Madan A, Stoecklein H, Ternovits C, et al. Predictive value of upper gastrointestinal studies versus clinical signs for gastrointestinal leaks after laparoscopic gastric bypass. Surg Endosc. 2007;21(2):194–6.
Sapala JA, Wood MH, Schunhkencht MP. Anastomotic leak prophylaxis using a vapor heated fibrin sealant: report on 738 gastric bypass patients. Obes Surg. 2004;14(1):35–42.
Wendling MR, Linn JG, Keplinger KM, et al. Omental patch repair effectively treats perforated marginal ulcer following Roux en Y gatric bypass. Surg Endosc. 2013;27(2):384–9.
Jacobsen HJ, Nergard BJ, Leifsson BG, et al. Management of suspected anastomotic leak after bariatric laparoscopic Roux en gastric bypass. Br J Surg. 2014;101(4):417–23.
Haddad A, Tapazoglou N, Singh K, et al. Role of intraoperative esophagogastroenteroscopy in minimizing gastrojejunostomy-related morbidity: experience with 2,311 laparoscopic gastric bypasses with linear stapler anastomosis. Obes Surg. 2012;22(12):1928–33.
Champion J, Hunt T, DeLisle N. Role of routine intraoperative endoscopy in laparoscopic bariatric surgery. Surg Endosc Interv Tech. 2002;16(12):1663–5.
Ramanathan R, Ikramuddin D, Gourash W, et al. The value of intraoperative endoscopy during laparoscopic Roux-en-Y gastric bypass for morbid obesity. Surg Endosc. 2000;14:212.
Finks JF, Carlin A, Share D, et al. Michigan bariatric surgery collaborative. Effects of surgical technique on clinical outcomes after laparoscopic gastric bypass—results of the Michigan bariatric surgery collaborative. Surg Obes Relat Dis. 2011;7(3):284–9. doi:10.1016/j.soard.2010.10.004.
Alasfar F, Sabnis AA, Liu RC, et al. Stricture rate after laparoscopic Roux-en-Y gastric bypass with a 21-mm circular stapler: the Cleveland Clinic experience. Med Princ Pract. 2009;18(5):364–7.
Dolce CJ, Dunnican WJ, Kushnir L, et al. Gastrojejunal strictures after Roux-en-Y gastric bypass with a 21-mm circular stapler. JSLS J Soc Laparoendosc Surg. 2009;13(3):306–11.
Giordano S, Tolonen P, Victorzon M. Comparision of linear versus circular stapling techniques in laparoscopic gastric bypass surgery—a pilot study. Scand J Surg: SJS: Off Organ Finn Surg Soc Scand Surg Soc. 2009;99(3):127–31.
Go MR, Muscarella P, Needleman BJ, et al. Endoscopic management of stomal stenosis after Roux en Y gastric bypass. Surg Endosc. 2004;18(1):56–9.
Gonzalez R, Lin E, Venkatesh KR, et al. Gastrojejunostomy during laparoscopic gastric bypass: analysis of 3 techniques. Arch Surg. 2003;138(2):181–4.
Conflict of Interest
Drs. Al Hadad, Dehni, Elamin, Ibrahim, Ghabra, and Nimeri have no conflicts of interest or financial ties to disclose. For this type of study, a formal consent is not required.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Al Hadad, M., Dehni, N., Elamin, D. et al. Intraoperative Endoscopy Decreases Postoperative Complications in Laparoscopic Roux-en-Y Gastric Bypass. OBES SURG 25, 1711–1715 (2015). https://doi.org/10.1007/s11695-015-1604-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-015-1604-z