Abstract
Background
Eligibility criteria for bariatric surgery (BS) are based on BMI and the presence of major comorbidities. Our aim was to analyze the usefulness of body adiposity determination in establishing the indication for BS.
Methods
In order to analyze the cardiometabolic risk according to eligibility criteria for BS, four groups were studied. Morbidly obese patients with BMI ≥40 kg/m2 (n = 360), and obese subjects with BMI ≥35 kg/m2 and at least one comorbidity (n = 431), represented two groups of patients meeting original NIH criteria for BS. A third group included two cohorts of patients with a high body fat (BF)% that do not meet the original NIH eligibility criteria for BS: patients with either a BMI <35 kg/m2 or a BMI ≥35 kg/m2 without comorbidities (n = 266, NEHF). Lean subjects by BMI were the reference group (n = 140). BMI, BF% and markers of insulin sensitivity, lipid profile, and cardiovascular risk were measured.
Results
Individuals from the NEHF group exhibited increased HbA1c (P < 0.05) and decreased insulin sensitivity evidenced by a significant reduction in QUICKI (P < 0.001). Triglyceride concentrations were similarly increased (P < 0.05) in the three groups of obese patients. Uric acid concentrations were significantly elevated (P < 0.01) to a similar extent in the obese groups. Levels of the inflammatory marker CRP and hepatic enzymes were significantly increased in the three obese groups.
Conclusion
The present study provides evidence for the existence of an adverse cardiometabolic profile in subjects currently considered to be outside traditional NIH guidelines but exhibiting a highly increased adiposity. It is concluded that body composition analysis yields valuable information to be incorporated into indication criteria for BS and that adiposity may be an independent indicator for BS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of obesity is increasing dramatically worldwide [1]. This circumstance has fostered a greater understanding of the mechanisms that regulate body weight and energy homeostasis [2]. Excess adiposity increases the risk of developing type 2 diabetes [3], cardiovascular disease (CVD) [4], non-alcoholic fatty liver disease [5], sleep apnea [6], other respiratory alterations [7], and cancer [8, 9], which translates into increased health expenses [10] and leads to higher morbidity and reduced life expectancy [11]. A huge body of evidence supports that the increased dysregulated adipose tissue lies at the heart of the development of most of the cardiometabolic comorbidities in relation to the favoring of lipid accumulation as opposed to lipolysis [12–14].
When lifestyle modification and pharmacologic treatment of obesity fail, the surgical treatment should be considered [15]. Bariatric surgery is the most effective strategy for achieving significant and sustainable long-term weight loss [16] ameliorating type 2 diabetes [17–19], decreasing cardiovascular events [20], and reducing long-term mortality [16, 21]. Classically, obese patients eligible for bariatric surgery are those with a BMI ≥40 kg/m2 or with a BMI ≥35 kg/m2 accompanied by at least one life-threatening comorbid condition such as type 2 diabetes or CVD [22]. Nevertheless, the recently updated clinical practice guidelines for bariatric surgery reflect the therapeutic potential of the surgical approach also for patients with a lower BMI who have increased cardiometabolic risk factors in spite of the lower body weight [23, 24]. However, BMI is only a surrogate measure of body fatness and does not provide an accurate measure of body composition [25–28]. Noteworthy, obesity is defined medically as an excess accumulation of body fat (BF) to the extent that health may be adversely affected [29].
Therefore, the aim of the present study was to analyze the usefulness for bariatric surgery indication of adiposity determination in relation to increased cardiometabolic risk compared to BMI-based criteria.
Methods
Study Population
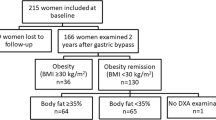
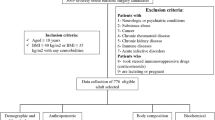
We conducted a cross-sectional analysis of 2921 Caucasian subjects (1682 females/1239 males), aged 18–70 years with similar socioeconomical characteristics including patients visiting the Department of Endocrinology and Nutrition and the Department of Surgery of the Clínica Universidad de Navarra (Pamplona, Spain) for weight loss treatment as well as hospital and University staff undergoing an annual routine health check-up with complete body composition, blood pressure, diabetic status, and lipid profile analyses between 2006 and 2012. All patients were weight-stable for the previous 3 months. In order to analyze the cardiometabolic risk in the different groups depending on eligibility criteria for bariatric surgery, four groups were established. The first two groups comprised patients eligible for bariatric surgery according to original NIH criteria [24, 30], i.e., morbidly obese subjects with BMI ≥40 kg/m2 (n = 360, 202 women and 158 men), and obese patients with BMI ≥35 kg/m2 and at least one comorbidity (n = 431, 237 women and 194 men). A third group included patients with a BMI <35 kg/m2 but with a morbidly obese adiposity (BF% > 50 % in women and >40 % in men), or individuals exhibiting a BMI ≥35 kg/m2 without comorbidities and a BF% within the obesity range (>35 % in women and >25 % in men) [n = 266, 158 women and 108 men, both classified together as the non-eligible high-fat (HF) group, NEHF]. Subjects classified as lean by BMI exhibiting a BF% lower than 35 % in women and 25 % in men (n = 140, 105 women and 35 men) were included as the reference (lean) group. The final sample encompassed 1197 individuals from the four groups (702 women and 495 men). To further analyze the influence of adiposity, we performed an additional analysis stratifying individuals with same BMI value and comparing those on the lower half vs those on the upper half of adiposity followed by correlation analysis between metabolic parameters and BF% as well as BMI in the whole sample (n = 2,921). Comorbidities were considered as having previously diagnosed type 2 diabetes or an elevated fasting plasma glucose, systolic blood pressure (SBP) ≥130 or diastolic blood pressure (DBP) ≥85 mm Hg or treatment of previously diagnosed hypertension, circulating triglyceride concentrations ≥150 mg/dL or medication for this lipid abnormality, or low HDL-cholesterol concentrations <40 mg/dL in males and <50 mg/dL in females. All subjects were non-smokers. Patients with signs of infection were excluded. The experimental design was approved, from an ethical and scientific standpoint, by the Hospital’s Ethical Committee responsible for research, and the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments. Informed consent was obtained from all individual participants included in the study.
Anthropometric Measurements
The anthropometric and body composition determinations as well as the blood extraction were performed on a single day. Height was measured to the nearest 0.1 cm with a Holtain stadiometer (Holtain Ltd., Crymych, UK), while body weight was measured with a calibrated electronic scale to the nearest 0.1 kg with subjects wearing a swimming suit and cap. Waist circumference was measured at the midpoint between the iliac crest and the rib cage on the midaxillary line. Blood pressure was measured after a 5-min rest in the semi-sitting position with a sphygmomanometer. Blood pressure was determined at least 3 times at the right upper arm, and the mean was used in the analyses. The presence of hypertension was defined by a SBP ≥130 mm Hg or DBP ≥85 mm Hg.
Body Composition
Body density was estimated by air displacement plethysmography (Bod-Pod, Life Measurements, Concord, CA, USA). Data for estimation of body fat by this plethysmographic method has been reported to agree closely with the traditional gold standard hydrodensitometry underwater weighing [26]. Percentage of body fat was estimated from body density using the Siri equation.
Laboratory Procedures
Blood samples were collected after an overnight fast in the morning in order to avoid potential confounding influences due to hormonal rhythmicity. Plasma glucose and insulin was analyzed as previously described [31]. An indirect measure of insulin sensitivity was calculated from the fasting plasma glucose and insulin concentrations by using the quantitative insulin sensitivity check index (QUICKI). HbA1c was measured by high-performance liquid chromatography in an Automatic Glycohaemoglobin Analyzer ADAMS™ A1c HA-8160 (Arkray, Kyoto, Japan). Total cholesterol and triglyceride concentrations were determined by enzymatic spectrophotometric methods (Roche, Basel, Switzerland). High-density lipoprotein (HDL-cholesterol) was quantified by a colorimetric method in a Beckman Synchron® CX analyzer (Beckman Instruments, Ltd., Bucks, UK). Low-density lipoprotein (LDL-cholesterol) was calculated by the Friedewald formula. Leptin was quantified by a double-antibody RIA method (Linco Research, Inc., St. Charles, MO, USA); intra-and inter-assay coefficients of variation were 5.0 and 4.5 %, respectively [32].
Uric acid, alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), and γ-glutamyltransferase (γ-GT) were measured by enzymatic tests (Roche) in an automated analyzer (Roche/Hitachi Modular P800). High-sensitivity C-reactive protein (CRP) was measured using the Tina-quant CRP (Latex) ultrasensitive assay (Roche). Fibrinogen concentrations were determined according to the method of Clauss using a commercially available kit (Hemoliance, Instrumentation Laboratory, Barcelona, Spain). White blood cell (WBC) count was measured using an automated cell counter (Beckman Coulter, Inc., Fullerton, CA, USA).
Statistical Analysis
Data are presented as mean ± standard deviation (SD). Differences between groups were analyzed by one-way ANOVA or by two-way ANOVA, as appropriate. If an interaction in the two-way ANOVA was detected, Student’s t test was performed to detect the difference between low and high adiposity. Correlations between two variables were computed by Spearman (ρ) correlation coefficient. Differences in proportions or number of subjects with hypertension were assessed by using χ 2. CRP concentrations were logarithmically transformed, because of their non-normal distribution. The distribution of other variables was adequate for the application of parametric tests. The calculations were performed using the SPSS version 15.0.1 (SPSS, Chicago, IL, USA). A P value lower than 0.05 was considered statistically significant.
Results
As expected, subjects from the “BMI ≥40” and “BMI 35–40 comorb” groups exhibited a higher BMI than those from the NEHF group, but BF% in the latter was significantly higher (P < 0.01) than in patients from the “BMI 35–40 comorb” group (Table 1). SBP and DBP were significantly higher in the three obese groups compared to the lean one, although mean values were higher in the “BMI 35–40 comorb” and “BMI ≥40” groups. In line with this, the prevalence of hypertension were significantly higher in the NEHF group (38 and 19 % in men and women, respectively) compared to the lean group (14 and 8 %; P < 0.01 and P = 0.010 vs NEHF), being more prevalent in the “BMI 35–40 comorb” (69 and 49 %) and “BMI ≥40” (70 and 58 %) groups.
Individuals from the NEHF group showed higher HbA1c (P < 0.05) as compared to the lean subjects, while no differences were observed with the “BMI 35–40 comorb” group (Fig. 1). In addition, they exhibited features of insulin resistance. Plasma glucose levels were within the glucose intolerance range in males, insulin concentrations were almost twice the levels of those of leans in both genders, and the QUICKI index, a surrogate marker of insulin sensitivity, was significantly lower (P < 0.001) in men and women (Table 2). Triglyceride concentrations were similarly increased in all three groups of obese patients, as compared to the lean controls (Table 2 and Fig. 2). Total cholesterol levels were unchanged in men and significantly higher (P < 0.05) only in the NEHF group in women. Levels of LDL-cholesterol were not modified in men and significantly higher (P < 0.01) in the NEHF and “BMI 35–40 comorb” groups in women. Leptin concentrations were similarly raised (P < 0.01) in the NEHF and “BMI 35–40 comorb” groups, as compared to the lean controls, being further increased (P < 0.001) in the “BMI ≥40” group.
Levels of HbA1c are increased in obese patients from the NEHF group. Box represents interquartile range and median inside, with whiskers showing 10/90 percentiles. Differences between groups were analyzed by one-way ANOVA. * P < 0.05, ** P < 0.01, and *** P < 0.001 vs lean. †† P < 0.01 vs NEHF and ¶ P < 0.05 vs BMI 35–40 comorb. NEHF non-eligible high-fat
Cardiometabolic risk is increased in obese patients from the NEHF group. Box represents interquartile range and median inside, with whiskers showing 10/90 percentiles. Differences between groups were analyzed by one-way ANOVA followed by Scheffé’s post hoc tests. * P < 0.05, ** P < 0.01, and *** P < 0.001 vs lean. † P < 0.05 and ††† P < 0.001 vs NEHF, and ¶ P < 0.05 and ¶¶ P < 0.01 vs BMI 35–40 comorb. AST aspartate aminotransferase, ALT alanine aminotransferase. NEHF non-eligible high-fat
Uric acid concentrations were significantly elevated (P < 0.01) to the same extent in the three obese groups in men, while in women they were raised (P < 0.001) in the NEHF and “BMI 35–40 comorb” groups, being further increased (P < 0.05) in the “BMI ≥40” group (Fig. 2 and Table 3). Levels of the inflammatory marker CRP were significantly higher in all three obese groups, with the morbid obesity group exhibiting the highest levels (Fig. 2). Liver function was altered in the three obese groups in both genders with ALT concentrations being similarly increased in all obese groups in men, while in women, ALT, ALP, and γ-GT concentrations were significantly higher (P < 0.01) in the three obese groups as compared to the lean individuals but without differences among them. The AST/ALT ratio has been proven to have discriminatory capacity for the differential diagnosis of liver diseases with a ratio < 1 being suggestive of the presence of non-alcoholic fatty liver disease [33, 34]. In this sense, the AST/ALT ratio was significantly lower in the three obese groups as compared to the lean individuals.
After stratifying individuals from the whole sample within different BMI ranges and different adiposity, we found that cardiometabolic risk markers were significantly worse in the subjects with a high adiposity as compared with individuals with a low adiposity (Fig. 3). Furthermore, both BF% and BMI were significantly correlated with most of the studied variables, being the association with BF% higher than the association with BMI for several cardiometabolic risk markers such as glucose 2 h after the OGTT, fibrinogen, WBC, and ALP in men and SBP, DBP, total- and LDL-cholesterol, fibrinogen, AST, ALP, and γ-GT in women (Supplementary Table 1).
Cardiometabolic risk markers are higher in individuals in the upper half of adiposity vs the lower half of adiposity independently of BMI. With this distribution, the upper half exhibited a mean BF% of 44.0 ± 8.2 % (n = 1461), while the lower half (n = 1460) showed a mean BF% of 38.1 ± 9.6 % (P < 0.0001). Box represents interquartile range and median inside, with whiskers showing 10/90 percentiles. Differences between groups were analyzed by two-way ANOVA. If an interaction in the two-way ANOVA was detected (AST/ALT ratio), Student’s t test was performed to assess differences between individuals with low vs high adiposity. * P < 0.05 main effect of body adiposity by two-way ANOVA. QUICKI quantitative insulin sensitivity check index, CRP C-reactive protein, AST aspartate aminotransferase, ALT alanine aminotransferase
Discussion
Obesity represents a body fat excess, with the amount of this excess correlating with comorbidity development [26, 28, 29, 35]. While BMI is the most frequently used tool for the diagnosis and classification of obesity, it is only a surrogate measure of body fatness and does not provide an accurate measure of body composition [26, 27]. Importantly, BMI cannot adequately discriminate the cardiometabolic risk at the individual level and, in this sense, we have recently shown that body fat determination may be very useful for better characterizing individuals with increased cardiometabolic risk due to excess adiposity [25–27, 36].
The present study shows that, in fact, obese patients with a BMI <35 kg/m2 or with a BMI ≥35 kg/m2 without comorbidities but with a high BF% exhibit a cardiometabolic profile similar to those patients with morbid obesity (BMI ≥40 kg/m2) or a BMI between 35 and 40 kg/m2 and comorbidities. We have previously shown that excess adiposity but not excess body weight is the real culprit of many obesity-associated complications [26] and, therefore, BF% rather than BMI should be considered in the decision-making algorithm based on its relation to the adverse cardiometabolic profile. Moreover, HbA1c was similarly increased between obese subjects with a BMI <35 kg/m2 or with a BMI ≥35 kg/m2 without comorbidities but with a high BF% (NEHF group) and those patients with a BMI between 35 and 40 kg/m2 and comorbidities, suggesting that their glycemic homeostasis is equally impaired. Given that bariatric surgery improves dyslipidemia, hyperuricemia, inflammation, and liver function [31, 37], all important components of the constellation of increased risk factors accompanying obesity, these patients with a high BF% irrespective of BMI with an increased cardiometabolic risk would certainly benefit from the surgical approach. In addition, improvements in glucose and lipid metabolism following bariatric surgery have been reported to correlate with fat mass changes [38]. Moreover, since several lines of evidence suggest that BMI is of limited use for bariatric surgery prioritization and preoperative BMI does not predict the surgical effect on outcomes [39], the proven benefits on detrimental cardiometabolic risk factors should be therefore put in front given that these obese patients with high adiposity exhibit similarly deranged cardiometabolic features leading to increased risk than those that are currently eligible for bariatric/metabolic surgery.
The effectiveness of bariatric surgery in the context of the management of obese patients not only for weight loss but, beyond that, also for the resolution or improvement of obesity-associated comorbidities has changed tremendously the view of the potential application of the surgical approach in recent years [40]. However, eligibility criteria for both bariatric and metabolic surgery are still BMI-based. Our study provides evidence for the benefit of incorporating body fat determination to better identify those obese patients which would benefit from the weight loss and metabolic changes following bariatric/metabolic surgery.
The large body of knowledge gained so far on the highly significant, reproducible, and long-lasting improvement or remission of metabolic alterations following the surgical approach comparing bariatric surgery with non-surgical interventions [17–19, 40, 41] supports taking management decisions focused more on functional determinations informing about the cardiometabolic risk rather than heavily relying on BMI-centric recommendations. Moreover, the metabolic improvement takes place via the activation of physiological mechanisms that go beyond weight loss [42]. In this sense, several studies have reported a safe and effective improvement or resolution of diabetes in type 2 diabetes obese patients with a BMI between 30 and 35 kg/m2 [43–46]. Furthermore, bariatric surgery exhibits notable beneficial effects not only on the resolution of type 2 diabetes but also in the amelioration of other life-threatening comorbidities associated with obesity. Importantly, bariatric surgery is also effective for the improvement or resolution of other relevant obesity-related comorbidities such as dyslipidemia, hypertension, or sleep apnea in subjects not meeting the original NIH eligibility criteria for bariatric surgery [30, 47]. Accordingly, in a recent update of clinical practice guidelines for bariatric surgery, it is indicated that patients with BMI of 30–34.9 kg/m2 with type 2 diabetes or metabolic syndrome may also be offered a bariatric procedure [23]. However, the actual cardiometabolic risk factor profile of these patients has not been considered in detail.
One potential limitation of our study pertains to the generalizability to other populations. This study was conducted in Caucasian subjects and needs to be extended to other populations to determine whether race differences yield different correlations to the cardiometabolic risk factors. However, it is expected that in both Asiatic and African-American individuals, similar findings are obtained, especially taking into consideration the higher visceral adiposity observed in these populations for a given BMI [48].
In summary, the present study provides evidence for the existence of a similar adverse cardiometabolic profile in subjects with a BMI <35 kg/m2 or with a BMI ≥35 kg/m2 without comorbidities but with a high adiposity compared to morbid obese patients. Since excess adiposity is the main culprit of many obesity-associated complications, these patients at an increased cardiometabolic risk would also benefit from the positive effects of the surgical approach. It is our belief that these novel findings are of clinical relevance in the management of non-morbidly obese individuals who already exhibit derangements in glucose and lipid metabolism which increase their cardiometabolic risk and struggle to reduce their weight and control their risk profile via conventional means. It is concluded that body composition analysis yields valuable information to be incorporated into bariatric/metabolic surgery selection algorithms more in line with evaluating the cardiometabolic risk profile of the patient.
References
Frühbeck G, Toplak H, Woodward E, et al. Obesity: the gateway to ill health—an EASO position statement on a rising public health, clinical and scientific challenge in Europe. Obes Facts. 2013;6:117–20.
Frühbeck G, Gómez-Ambrosi J. Control of body weight: a physiologic and transgenic perspective. Diabetologia. 2003;46:143–72.
Kahn SE, Cooper ME, Del Prato S. Pathophysiology and treatment of type 2 diabetes: perspectives on the past, present, and future. Lancet. 2014;383:1068–83.
Apovian CM, Gokce N. Obesity and cardiovascular disease. Circulation. 2012;125:1178–82.
Cusi K. Role of obesity and lipotoxicity in the development of nonalcoholic steatohepatitis: pathophysiology and clinical implications. Gastroenterology. 2012;142:711–25 e6.
Jordan AS, McSharry DG, Malhotra A. Adult obstructive sleep apnoea. Lancet. 2014;383:736–47.
Campo A, Frühbeck G, Zulueta JJ, et al. Hyperleptinaemia, respiratory drive and hypercapnic response in obese patients. Eur Respir J. 2007;30:223–31.
Catalán V, Gómez-Ambrosi J, Rodríguez A, et al. Adipose tissue immunity and cancer. Front Physiol. 2013;4:275.
Bhaskaran K, Douglas I, Forbes H, et al. Body-mass index and risk of 22 specific cancers: a population-based cohort study of 5.24 million UK adults. Lancet. 2014;384:755–65.
Withrow D, Alter DA. The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obes Rev. 2011;12:131–41.
Tobias DK, Pan A, Jackson CL, et al. Body-mass index and mortality among adults with incident type 2 diabetes. N Engl J Med. 2014;370:233–44.
Frühbeck G, Gómez Ambrosi J, Salvador J. Leptin-induced lipolysis opposes the tonic inhibition of endogenous adenosine in white adipocytes. FASEB J. 2001;15:333–40.
Frühbeck G. Overview of adipose tissue and its role in obesity and metabolic disorders. Methods Mol Biol. 2008;456:1–22.
Poulain-Godefroy O, Lecoeur C, Pattou F, et al. Inflammation is associated with a decrease of lipogenic factors in omental fat in women. Am J Physiol Regul Integr Comp Physiol. 2008;295:R1–7.
Vest AR, Heneghan HM, Schauer PR, et al. Surgical management of obesity and the relationship to cardiovascular disease. Circulation. 2013;127:945–59.
Sjöström L, Narbro K, Sjöström CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741–52.
Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012;366:1577–85.
Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366:1567–76.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes—3-year outcomes. N Engl J Med. 2014;370:2002–13.
Sjöström L, Peltonen M, Jacobson P, et al. Bariatric surgery and long-term cardiovascular events. JAMA. 2012;307:56–65.
Pontiroli AE, Morabito A. Long-term prevention of mortality in morbid obesity through bariatric surgery. A systematic review and meta-analysis of trials performed with gastric banding and gastric bypass. Ann Surg. 2011;253:484–7.
Neff KJ, le Roux CW. Bariatric surgery: a best practice article. J Clin Pathol. 2013;66:90–8.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American association of clinical endocrinologists, the obesity society, and American society for metabolic & bariatric surgery. Obesity. 2013;21 Suppl 1:S1–27.
Fried M, Yumuk V, Oppert JM, et al. Interdisciplinary European guidelines on metabolic and bariatric surgery. Obes Surg. 2014;24:42–55.
Gómez-Ambrosi J, Silva C, Galofré JC, et al. Body adiposity and type 2 diabetes: increased risk with a high body fat percentage even having a normal BMI. Obesity. 2011;19:1439–44.
Gómez-Ambrosi J, Silva C, Galofré JC, et al. Body mass index classification misses subjects with increased cardiometabolic risk factors related to elevated adiposity. Int J Obes. 2012;36:286–94.
Gómez-Ambrosi J, Silva C, Catalán V, et al. Clinical usefulness of a new equation for estimating body fat. Diabetes Care. 2012;35:383–8.
Blundell JE, Dulloo AG, Salvador J, et al. Beyond BMI—phenotyping the obesities. Obes Facts. 2014;7:322–8.
Frühbeck G. Obesity: screening for the evident in obesity. Nat Rev Endocrinol. 2012;8:570–2.
Gastrointestinal surgery for severe obesity: National Institutes of Health Consensus Development Conference Statement. Am J Clin Nutr. 1992;55:615S-9S.
Gómez-Ambrosi J, Salvador J, Rotellar F, et al. Increased serum amyloid A concentrations in morbid obesity decrease after gastric bypass. Obes Surg. 2006;16:262–9.
Muruzábal FJ, Frühbeck G, Gómez-Ambrosi J, et al. Immunocytochemical detection of leptin in non-mammalian vertebrate stomach. Gen Comp Endocrinol. 2002;128:149–52.
Sorbi D, Boynton J, Lindor KD. The ratio of aspartate aminotransferase to alanine aminotransferase: potential value in differentiating nonalcoholic steatohepatitis from alcoholic liver disease. Am J Gastroenterol. 1999;94:1018–22.
Kotronen A, Peltonen M, Hakkarainen A, et al. Prediction of non-alcoholic fatty liver disease and liver fat using metabolic and genetic factors. Gastroenterology. 2009;137:865–72.
Prentice AM, Jebb SA. Beyond body mass index. Obes Rev. 2001;2:141–7.
Gómez-Ambrosi J, Salvador J, Frühbeck G. Letter by Gómez-Ambrosi et al. regarding article, “Clinical assessment and management of adult obesity”. Circulation. 2013;128:e39.
Gómez-Ambrosi J, Catalán V, Rodríguez A, et al. Involvement of serum vascular endothelial growth factor family members in the development of obesity in mice and humans. J Nutr Biochem. 2010;21:774–80.
Frige F, Laneri M, Veronelli A, et al. Bariatric surgery in obesity: changes of glucose and lipid metabolism correlate with changes of fat mass. Nutr Metab Cardiovasc Dis. 2009;19:198–204.
Sjöström L. Review of the key results from the Swedish obese subjects (SOS) trial—a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013;273:219–34.
Miras AD, le Roux CW. Metabolic surgery: shifting the focus from glycaemia and weight to end-organ health. Lancet Diabetes Endocrinol. 2014;2:141–51.
Gómez-Ambrosi J, Pastor C, Salvador J, et al. Influence of waist circumference on the metabolic risk associated with impaired fasting glucose: effect of weight loss after gastric bypass. Obes Surg. 2007;17:585–91.
Cummings DE. Metabolic surgery for type 2 diabetes. Nat Med. 2012;18:656–8.
Li Q, Chen L, Yang Z, et al. Metabolic effects of bariatric surgery in type 2 diabetic patients with body mass index < 35 kg/m2. Diabetes Obes Metab. 2012;14:262–70.
Cohen RV, Pinheiro JC, Schiavon CA, et al. Effects of gastric bypass surgery in patients with type 2 diabetes and only mild obesity. Diabetes Care. 2012;35:1420–8.
Kashyap SR, Bhatt DL, Wolski K, et al. Metabolic effects of bariatric surgery in patients with moderate obesity and type 2 diabetes: Analysis of a randomized control trial comparing surgery with intensive medical treatment. Diabetes Care. 2013;36:2175–82.
Ikramuddin S, Korner J, Lee WJ, et al. Roux-en-Y gastric bypass vs intensive medical management for the control of type 2 diabetes, hypertension, and hyperlipidemia: the Diabetes Surgery Study randomized clinical trial. JAMA. 2013;309:2240–9.
Sjöholm K, Anveden A, Peltonen M, et al. Evaluation of current eligibility criteria for bariatric surgery: diabetes prevention and risk factor changes in the Swedish obese subjects (SOS) study. Diabetes Care. 2013;36:1335–40.
Expert WHO. Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63.
Acknowledgments
The authors thank all of the members of the Nutrition Unit of the Department of Endocrinology & Nutrition (Clínica Universidad de Navarra, Pamplona, Spain) for their technical help.
Funding
The study was supported by grants from the ISCIII (PI09/91029, PI11/02681 and PI12/00515), the Department of Health (31/2009) of the Gobierno de Navarra, Fundación Caja Navarra (20–2014) and by the ISCIII, Centro de Investigación Biomédica en Red Fisiopatología de la Obesidad y Nutrición, CIBERobn, Spain.
Conflict of Interest
All authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Table 1
(DOC 137 kb)
Rights and permissions
About this article
Cite this article
Gómez-Ambrosi, J., Moncada, R., Valentí, V. et al. Cardiometabolic Profile Related to Body Adiposity Identifies Patients Eligible for Bariatric Surgery More Accurately than BMI. OBES SURG 25, 1594–1603 (2015). https://doi.org/10.1007/s11695-014-1566-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-014-1566-6