Abstract
Background
We aimed to examine the effect of Roux-en-Y gastric bypass surgery (RYGB) on erectile dysfunction (ED), cavernosal morphological vasculopathy, and carotid wall alterations in severely obese Chinese men.
Methods
We performed a retrospective cohort study of 39 obese men with ED who underwent RYGB between 2011 and 2012. Erectile function was assessed by the International Index of Erectile Function-5 (IIEF-5) before and 1 year after surgery. Intima-media thickness of carotid and cavernosal arteries and cavernosal peak systolic velocity (PSV) were investigated by color Doppler ultrasound. Endothelial function was assessed with the L-arginine test.
Results
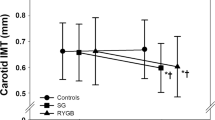
Eighteen (46.2 %) men had cavernosal vasculopathy and 21 (53.8 %) had carotid vasculopathy before surgery, and these proportions decreased to 15.4 % and 23.1 % after surgery, respectively. There was a significant improvement in carotid and cavernosal intima-media thickness postoperatively. IIEF-5 (17.3 to 23.8, P < 0.05), PSV (23 to 37, P < 0.05), and endothelial scores (6.1 to 8.2, P < 0.05) were all improved after RYGB. The increase in endothelial function scores was positively associated with changes in pre- to postoperative IIEF-5 scores (r = 0.438, P = 0.017). Younger age, being married, and lower preoperative IIEF-5 scores were independently related to greater improvement in erectile function.
Conclusions
ED can be relieved after RYGB in obese Chinese patients, accompanied by the improvement of cavernosal morphological vasculopathy and carotid wall alterations. Changes in endothelial function may contribute to this improvement, while preoperative body mass index and the amount of weight loss do not.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Erectile dysfunction (ED) is defined as the persistent inability to attain and maintain an erection that is sufficient to permit satisfactory sexual intercourse [1]. Several epidemiological studies have reported that a high prevalence of ED affected over 150 million men worldwide in 1995. This prevalence will reach 322 million by 2025 according to the Massachusetts Male Aging Study, with the largest projected increase in Africa, Asia, and South America [2].
ED is common in obese males. Obesity increases the risk of ED in individuals by 1.3 times and 79 % of the men suffering from ED are overweight [3]. Several studies have shown that development of ED is closely associated with diabetes, hyperlipidemia, hypertension, and metabolic syndrome [4–6]. ED is also significantly and independently associated with an increased risk of cardiovascular disease, coronary heart disease, stroke, and all-cause mortality, which indicates that ED is a warning sign of these diseases [4, 6–8]. Penile vascular impairment is one of the most important reasons for ED, and increased mean carotid artery intima-media thickness (IMT) is regarded as a predominant predictive factor of cardiovascular diseases and atherosclerosis [9]. A previous study suggested that patients with ED and metabolic syndrome have a higher prevalence of cavernosal vasculopathy and peripheral vascular alterations [10].
Currently, the growing consensus for treatment of ED favors bariatric surgery [11–13], which achieves substantial weight loss, significantly improves metabolic syndrome, and relieves type 2 diabetes [14, 15]. Furthermore, findings of several studies have shown that ED is reversed after gastric bypass surgery [16].
This study aimed to determine whether ED, cavernosal vasculopathy, and peripheral vascular alterations are improved after Roux-en-Y gastric bypass surgery (RYGB) in Chinese patients with ED. Furthermore, we examined which factors might contribute to the improvement of erectile function and which factors were independently related to a greater postoperative improvement in the International Index of Erectile Function-5 (IIEF-5) scores.
Materials and Methods
Participants and Procedures
Patients in our study were recruited from the Sixth People’s Hospital Affiliated to Shanghai Jiao Tong University between 2011 and 2012. A total of 121 men had RYGB during this period. They all completed the IIEF-5 questionnaire prior to RYGB.
The inclusion criteria comprised patients in the Obesity Clinic of our hospital whose IIEF-5 score was less than 21, those who were 18–65 years old, and those who were candidates for RYGB. The exclusion criteria were men with scrotal trauma, corporal fibrosis, a history of pelvic surgery, use of phosphodiesterase type-5 inhibitors, or taking hormone replacement therapy. Of 53 patients enrolled in our study, 11 refused to participate and 3 complained of sexual inactivity during the past 4 weeks. Those 14 patients were excluded from our study and 39 participants remained (Fig. 1).
We performed a retrospective cohort study of 39 men who had completed a series of questionnaires and measurements, including clinical and ultrasound parameters before surgery and 1 year after surgery. All of the tests mentioned above were routine during the follow-up period and the results were available in hospital files.
Methods
Biochemical and hormonal parameters were evaluated by obtaining blood samples from all of the participants after an overnight fast. Samples were obtained 7 days before assessment of the IIEF-5. Biochemical parameters included plasma glucose levels, lipid profile (total cholesterol, high-density lipoprotein cholesterol, and triglyceride levels), and C-reactive protein (CRP) levels. Lipid profiles were determined by standard enzymatic methods (Hitachi 747 analyzer, Castle Hill, NSW, Australia). CRP levels were assayed by the particle-enhanced immunoturbidimetric analyzer (Roche Diagnostics, Mannheim, Germany). In addition, we measured testosterone levels by using an electrochemiluminescence immunoassay (Roche Diagnostics).
Anthropometric evaluations consisted of assessments of body weight, height, and waist circumference (WC). Weight was measured by using an electronic scale (accuracy = 0.1 kg) with the participant in barefoot and wearing light clothes. Height was determined by using a fixed wall stadiometer (accuracy = 0.5 cm). WC was measured with a standard, flexible, inelastic measuring tape (accuracy = 0.5 cm) at the level of the iliac crest. Body mass index (BMI) was calculated as weight/height2.
Five-item Version of the International Index of Erectile Function
Containing only 5 questions, each item on a 5-point scale (1–5), the IIEF-5 is an abridged IIEF, and is a useful subjective diagnostic tool for ED [9, 17]. The sum scores of all items are used to evaluate penile erectile function. A score of 0 refers to low erectile function, whereas a score of 5 indicates the best functional status. The total scores of the questionnaire survey range from 1 to 25, and the optimal cutoff of the scores for erectile function is 21. A man who scores more than 21 points is considered to have normal erectile function, otherwise, he is regarded as having ED. Based on the IIEF-5 scores, penile erectile function can be divided into 5 categories: severe ED (1–7), moderate ED (8–11), mild to moderate ED (12–16), mild ED (17–21), and normal erectile function (22–25).
Color Doppler Ultrasound Examination
All of the participants were measured by a high-resolution echo-color-Doppler (Aplio XV Toshiba, Tokyo, Japan) equipped with a multi-frequency linear probe by the same doctor who was blinded to the patients. Cavernosal peak systolic velocity (PSV), IMT, and carotid arterial IMT were measured [9]. Penile and carotid vasculopathy were classified [18].
Endothelial Function Testing
Endothelial function was evaluated by the L-arginine test, as previously described [19, 20]. Esposito designed a score in which platelet aggregation and blood pressure responses to L-arginine (3 g i.v.) are summed. This provides a score ranging from 0 to 10 points, which indicates maximal impairment of endothelial function and normal endothelial function, respectively [21].
Demographic Characteristics, History of Health, Current Medication, and Alcohol and Tobacco Consumption
Demographic data such as age, marital status, and educational level were collected via questionnaire. The Health History Checklist was used for assessing the participants’ health condition. This list included (1) whether the participants had been currently diagnosed with certain disorders (e.g., hypertension, diabetes, dyslipidemia, and metabolic syndrome), (2) whether they had experienced spinal cord injury, radical pelvic surgery, scrotal trauma, cavernous fibrosis, or prostatic disease, and (3) whether they had taken phosphodiesterase type 5 inhibitors or any other hormone replacement therapy. Finally, the names of medications, and the frequency of alcohol drinking and smoking were recorded.
Statistical Analysis
We performed statistical analysis using SPSS version 20.0. The preoperative and postoperative characteristics of obese men with ED were compared by using paired samples t tests. Changes in cavernosal or carotid vasculopathy were calculated by McNemar’s chi square test. Correlations between clinical parameters and IIEF-5 were analyzed by partial correlation analysis. Multivariate predictors of pre- to postoperative changes in IIEF-5 scores were conducted by stepwise regression analysis. Demographic (age, marital, and education status), preoperative variables (BMI and IIEF-5 score), and postoperative weight loss were entered in this procedure.
Statistical significance was defined as P < 0.05. Data are presented as the mean value ± SD.
Results
Demographic Characteristics
The study comprised 39 obese men with ED whose mean age was 45.2 years (range, 25–65 years) and the mean initial BMI was 41.2 kg/m2 (range, 36–59 kg/m2). One year after the operation, the mean BMI decreased from 41.2 to 32.1 kg/m2 and mean waist circumference decreased from 138.4 to 102.7 cm (P < 0.05) (Table 1).
Participants were predominantly married (84.6 %) and over half (53.8 %) of them had at least a 4-year college degree. The most commonly reported health conditions preoperatively were diabetes (100 %), hypertension (76.9 %), hyperlipidemia (69.2 %), and metabolic syndrome (59 %). Slightly less than half (46.2 %) of the participants drank more than 1 alcoholic drink per week and nearly a quarter of those (25.6 %) had smoked more than 25 pack-years (Table 2).
Medication Use
Medications that were most commonly taken preoperatively were statins (74.4 %), antihypertensives (76.9 %), oral diabetes medication (43.6 %), insulin (66.7 %), antiarrhythmics (41 %), and anti-reflux medication (15.4 %) (Table 2). The data of medication use at baseline and 1 year after surgery are shown in Table 3. A total of 43.5 % of participants no longer required any class of medication 1 year after surgery, 61.5 % no longer required any class of diabetes medication 1 year after surgery, 46.6 % no longer required any class of hypertension medication 1 year after surgery, and 74.2 % no longer required any class of hyperlipidemia medication 1 year after surgery (Table 3).
Clinical and Ultrasound Parameters, and ED
Fasting blood glucose, total cholesterol, and triglyceride levels were significantly decreased after surgery compared with before surgery (P < 0.05). High-density lipoprotein cholesterol levels were markedly increased postoperatively compared with preoperatively (P < 0.05, Table 1). There was a trend for a decrease in serum CRP levels in obese men with ED postoperatively compared with preoperatively, (P = 0.329). Testosterone levels were moderately elevated after surgery compared with before surgery (P = 0.052).
Baseline IIEF-5 scores before the operation were less than 21 points. The mean postoperative IIEF-5 score increased from 17.3 points before surgery to 23.8 points after surgery (P < 0.05). PSV and endothelial function scores were significantly increased postoperatively compared with preoperatively (P < 0.05). Furthermore, cavernosal and carotid IMT were decreased (P < 0.05), as well as cavernosal and carotid vasculopathy, postoperatively compared with preoperatively (P < 0.05).
We also examined changes in the IIEF-5 score and clinical parameters pre- to postoperatively by multivariate correlation analysis (Table 4). We found that the increase in IIEF-5 scores after surgery was positively associated with the improvement of endothelial function (r = 0.438, P = 0.017).
The results of multivariate regression analysis are shown in Table 5. Being married, having younger age, and having lower preoperative IIEF-5 scores were independently correlated with a greater improvement in IIEF-5 scores postoperatively.
Discussion
The prevalence of ED in patients with metabolic syndrome is directly proportional to the number of metabolic syndrome components [22], with approximately 20, 30, and 35 % of patients with ED having 3, 4, or 5 components of metabolic syndrome, respectively. In addition, subsequent studies have indicated that WC, hypertension, high cholesterol levels, diabetes, and advanced age are all increased with the risk of ED [23, 24]. Several studies have provided evidence that bariatric surgery may play an essential role in the improvement of ED. In our study, we found that IIEF-5 scores were increased after gastric bypass surgery in obese Chinese patients with ED. Cavernosal morphological vasculopathy and carotid wall alterations were decreased after surgery. We also found that the improvement in endothelial function might have contributed to this positive effect. Additionally, younger age, being married, and lower preoperative IIEF-5 scores were independently correlated with greater postoperative improvement in IIEF-5 scores.
Ethnicity is regarded as a factor that affects sexual function [25, 26]. However, previous studies that reported a positive effect of bariatric surgery on erectile function were primarily conducted in Western individuals [27–29]. Whether these results are also present in Chinese patients is unknown. This study has provided preliminary evidence that indicates that there are similar improvements in Chinese men with ED after surgery.
Penile vascular impairment, which is the predominant reason for ED, is diagnosed by PSV and cavernosal arterial morphology (IMT ≥0.3 mm or presence of plaques) [30], which are directly related to peripheral vasculopathy and the severity of cardiovascular risk factors [31]. Furthermore, an increased mean carotid artery IMT is a good predictive parameter of generalized atherosclerosis and cardiovascular disease, and does correlate with erectile function [9]. There is a higher prevalence of cavernosal vasculopathy or plaques in patients with ED and metabolic syndrome compared with ED patients without metabolic syndrome. Our study found that with the improvement of ED and metabolic syndrome, the incidence of cavernosal morphological vasculopathy and carotid wall alterations decreased and PSV improved.
Several studies have shown that sexual function can be improved after gastric bypass surgery. Dallal et al. found that half of ED patients no longer required treatment with medications, which might have a close relationship with the improvement of obesity-related ED [29]. Moreover, Reis et al. pointed out that surgery-induced weight loss and increased testosterone levels could justify an improvement of erectile function [27]. However, in our study, we found that improved endothelial function might have a close correlation with reversed ED. Multifactorial mechanisms may be involved in surgery-associated improvement of ED.
Endothelial dysfunction and abnormalities of the vasodilator system play an important part in the pathophysiology of ED. Vascular disease of penile arteries is the most common cause of ED, accounting for up to 80 % of cases [32, 33]. Endothelial dysfunction prevents the smooth muscle cells lining the arterioles from relaxing, which inhibits vasodilatation [34]. In addition, impairment of endothelial-dependent vasodilatation, which causes atherosclerosis of arteries, leads to flow-limiting stenosis of the penile artery. Adequate cavernous flow is indispensable to achieve an erection, while flow-limiting stenosis of the penile artery may prevent an adequate arterial supply, thus causing ED. In our study, we found an improvement in PSV and endothelial function scores in patients with ED after surgery, which might explain the reversal of ED.
Interestingly, our findings indicated that the improvement of ED in Chinese men undergoing bariatric surgery may be independent of BMI and weight loss. Therefore, further studies are needed to evaluate the extent of postoperative changes in correlated variables, including neurogenic endocrinological and psychogenic factors, which may account for these improvements. Additionally, drugs, including antihypertensives, antiarrhythmics, and statins, are frequently associated with ED [24, 35]. There was a high rate of frequent use of medication in our study. Medication use decreased and 43.5 % of the patients completely stopped taking drugs postoperatively (Table 3). Therefore, further investigation in larger samples is required to examine the effects of discontinued use of medication after surgery.
Several studies have shown that the development of ED is closely associated with diabetes, hyperlipidemia, hypertension, and metabolic syndrome [4–6]. In our patients, there was a high prevalence of diabetes, hypertension, dyslipidemia, and metabolic syndrome before the operation. After surgery, 61.5 % of diabetic patients, 46.6 % of hypertensive patients, and 74.2 % of dyslipidemia patients no longer required treatment. Whether short-term remission of these long-standing comorbidities postoperatively can improve erectile function is still unclear.
Findings from recent studies have indicated that lifestyle significantly affects ED [36], including smoking and alcohol use. Guay et al. reported that cessation of smoking can considerably and rapidly improve erectile function in individuals with a smoking history of at least 30 pack-years [37]. In addition, a 2011 meta-analysis suggested that lifestyle changes and a reduction in cardiovascular risk factors could greatly contribute to the improvement of erectile function [38]. In our study, almost half of the patients had a history of tobacco and alcohol abuse. Some people succeeded in quitting smoking and drinking, but others renewed tobacco and alcohol use postoperatively. Controlling these two factors is difficult. Therefore, we did not take these two factors into account in our statistical model. More comprehensive studies regarding the influence of lifestyle modifications on ED are required.
While ED was improved after RYGB, as well as cavernosal and carotid vasculopathy, the statistical power was limited by the small number of RYGB individuals. As noted above, a more comprehensive study of predictors of the improvement in ED in the Chinese population is required. Information is also required on whether short-term remission of comorbidities and lifestyle modifications after RYGB might account for these improvements. Consequently, future studies need to examine whether these improvements persist over time after stabilizing or regaining weight.
In summary, our study was the first to examine changes in ED in obese Chinese men with ED after gastric bypass surgery. This study shows that IIEF-5 scores, cavernosal morphological vasculopathy, and carotid wall alterations are improved after RYGB. The improvement in endothelial function might explain the reversed ED. In addition, younger age, being married, and lower preoperative IIEF-5 scores are independently related to greater postoperative improvement in IIEF-5 scores. A more comprehensive study is required to determine whether physiological, medical, lifestyle, and psychosocial elements play an important role, and if these improvements are sustained over time.
References
Wespes W, Amar E, Eardley I. EAU guidelines on male sexual dysfunction: erectile dysfunction and premature ejaculation. European Association of Urology Web site; 2009.
Aytac I, McKinlay J, Krane R. The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequences. BJU Int. 1999;84:50–6.
Bacon CG, Mittleman MA, Kawachi I, et al. Sexual function in men older than 50 years of age: results from the health professionals’ follow-up study. Ann Intern Med. 2003;139:161–8.
Clark NG, Fox KM, Grandy S. Symptoms of diabetes and their association with the risk and presence of diabetes findings from the study to help improve early evaluation and management of risk factors leading to diabetes (SHIELD). Diabetes Care. 2007;30:2868–73.
Ponholzer A, Temml C, Obermayr R, et al. Is erectile dysfunction an indicator for increased risk of coronary heart disease and stroke? Eur Urol. 2005;48:512–8.
Chung SD, Chen YK, Lin HC, et al. Increased risk of stroke among men with erectile dysfunction: a nationwide population‐based study. J Sex Med. 2011;8:240–6.
Inman BA, St Sauver JL, Jacobson DJ, et al. A population-based, longitudinal study of erectile dysfunction and future coronary artery disease. Mayo Clinic Proceedings. Elsevier; 2009, pp 108–13.
Dong J-Y, Zhang Y-H, Qin L-Q. Erectile dysfunction and risk of cardiovascular disease meta-analysis of prospective cohort studies. J Am Coll Cardiol. 2011;58:1378–85.
Caretta N, Palego P, Roverato A, et al. Age-matched cavernous peak systolic velocity: a highly sensitive parameter in the diagnosis of arteriogenic erectile dysfunction. Int J Impot Res. 2005;18:306–10.
Schipilliti M, Caretta N, Palego P, et al. Metabolic syndrome and erectile dysfunction. The ultrasound evaluation of cavernosal atherosclerosis. Diabetes Care. 2011;34:1875–7.
Prevention I, TYPE DO. Standards of medical care in diabetes—2011. Diabetes Care. 2011;34:S11.
Dixon J, Zimmet P, Alberti K, et al. Bariatric surgery: an IDF statement for obese type 2 diabetes. Diabet Med. 2011;28:628–42.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient–2013 update: cosponsored by american association of clinical endocrinologists, the obesity society, and american society for metabolic & bariatric surgery. Surg Obes Relat Dis. 2013.
Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012;366:1577–85.
Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366:1567–76.
Reis L, Favaro W, Barreiro G, et al. Erectile dysfunction and hormonal imbalance in morbidly obese male is reversed after gastric bypass surgery: a prospective randomized controlled trial. Int J Androl. 2010;33:736–44.
Rhoden E, Teloken C, Sogari P, et al. The use of the simplified International Index of Erectile Function (IIEF-5) as a diagnostic tool to study the prevalence of erectile dysfunction. Int J Impot Res. 2002;14:245–50.
Foresta C, Palego P, Schipilliti M, et al. Asymmetric development of peripheral atherosclerosis in patients with erectile dysfunction: an ultrasonographic study. Atherosclerosis. 2008;197:889–95.
Giugliano D, Marfella R, Verrazzo G, et al. L-arginine for testing endothelium-dependent vascular functions in health and disease. Am J Physiol Endocrinol Metab. 1997;36:E606–12.
Esposito K, Nappo F, Giugliano F, et al. Effect of dietary antioxidants on postprandial endothelial dysfunction induced by a high-fat meal in healthy subjects. Am J Clin Nutr. 2003;77:139–43.
Esposito K, Marfella R, Ciotola M, et al. Effect of a Mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome. J Am Med Assoc. 2004;292:1440–6.
Esposito K, Giugliano F, Martedì E, et al. High proportions of erectile dysfunction in men with the metabolic syndrome. Diabetes Care. 2005;28:1201–3.
Lewis RW, Fugl-Meyer KS, Bosch R, et al. Epidemiology/risk factors of sexual dysfunction. J Sex Med. 2004;1:35–9.
Shamloul R, Ghanem H. Erectile dysfunction. Lancet. 2013;381:153–65.
Masumori N, Tsukamoto T, Kumamoto Y, et al. Decline of sexual function with age in Japanese men compared with American men—results of two community-based studies. Urology. 1999;54:335–44.
Laumann EO, West S, Glasser D, et al. Prevalence and correlates of erectile dysfunction by race and ethnicity among men aged 40 or older in the United States: from the male attitudes regarding sexual health survey. J Sex Med. 2007;4:57–65.
Reis LO, Favaro WJ, Barreiro GC, et al. Erectile dysfunction and hormonal imbalance in morbidly obese male is reversed after gastric bypass surgery: a prospective randomized controlled trial. Int J Androl. 2010;33:736–44.
Hammoud A, Gibson M, Hunt SC, et al. Effect of Roux-en-Y gastric bypass surgery on the sex steroids and quality of life in obese men. J Clin Endocrinol Metab. 2009;94:1329–32.
Dallal RM, Chernoff A, O’Leary MP, et al. Sexual dysfunction is common in the morbidly obese male and improves after gastric bypass surgery. J Am Coll Surg. 2008;207:859–64.
Jackson G, Montorsi P, Adams MA, et al. Cardiovascular aspects of sexual medicine. J Sex Med. 2008;7:1608–26.
Caretta N, Palego P, Schipilliti M, et al. Cavernous artery intima-media thickness: a new parameter in the diagnosis of vascular erectile dysfunction. J Sex Med. 2009;6:1117–26.
Virag R, Bouilly P, Frydman D. Is impotence an arterial disorder?: a study of arterial risk factors in 440 impotent men. Lancet. 1985;325:181–4.
O’Kane P, Jackson G. Erectile dysfunction: is there silent obstructive coronary artery disease? Int J Clin Pract. 2001;55:219–20.
Kaiser DR, Billups K, Mason C, et al. Impaired brachial artery endothelium-dependent and -independent vasodilation in men with erectile dysfunction and no other clinical cardiovascular disease. J Am Coll Cardiol. 2004;43:179–84.
Rizvi K, Hampson JP, Harvey JN. Do lipid-lowering drugs cause erectile dysfunction? A systematic review. Fam Pract. 2002;19:95–8.
Rosen RC, Wing R, Schneider S, et al. Epidemiology of erectile dysfunction: the role of medical comorbidities and lifestyle factors. Urol Clin N Am. 2005;32:403–17.
Guay M, FACE, André T, et al. Cessation of smoking rapidly decreases erectile dysfunction. Endocr Pract. 1998;4:23–6.
Gupta BP, Murad MH, Clifton MM, et al. The effect of lifestyle modification and cardiovascular risk factor reduction on erectile dysfunction. A systematic review and meta-analysis. Arch Intern Med. 2011;171:1797–803.
Acknowledgments
We thank the staff of the Hospital Information Center of The Sixth People’s Hospital Affiliated to Shanghai Jiao Tong University for abstracting patients’ data from medical records.
Funding
This work did not receive any specific grant from any funding agency in the public, commercial or not for-profit sector.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethical Approval
For this type of study (retrospective study) formal consent is not required.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Li Kun and Zhang Pin contributed equally to this work.
Rights and permissions
About this article
Cite this article
Kun, L., Pin, Z., Jianzhong, D. et al. Significant Improvement of Erectile Function after Roux-en-Y Gastric Bypass Surgery in Obese Chinese Men with Erectile Dysfunction. OBES SURG 25, 838–844 (2015). https://doi.org/10.1007/s11695-014-1465-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-014-1465-x