Abstract
Background
Bariatric surgery is the most effective treatment for patients suffering from obesity-related comorbidities. There is little data regarding how patients choose one particular bariatric procedure over another. This study aimed to better define the relationship between preferences of patients considering bariatric surgery and the procedure patients undergo.
Methods
A bilingual questionnaire was administered to all prospective patients seen between March 1 and August 31, 2012. The questionnaire assessed basic knowledge of bariatric surgery (based on the information seminar) as well as patient preferences of the various outcomes and complications for sleeve gastrectomy, gastric bypass, and gastric banding.
Results
One hundred seventy-two patients completed the questionnaire. Fifty-eight percent of patients chose “maximum weight loss” as the most important outcome, and 65 % chose “leak” as the most concerning complication. Subgroup analysis of patients with diabetes revealed that 58 % chose “curing diabetes” as the most important outcome. Nineteen percent of patients were either not sure which procedure they wanted or changed their decision after consultation with the surgeon.
Conclusions
The decision to choose one bariatric procedure over another is complex and is based on factors beyond absolute patient preferences. Although maximum weight loss is a commonly reported preference for patients seeking bariatric surgery, patients with diabetes are more focused on diabetes remission. Most patients have already decided which procedure to undergo prior to surgeon consultation. Patients may benefit from shared decision making, which integrates patient values and preferences along with current medical evidence to assist in the complex bariatric surgery selection process.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery has been shown to be safe and effective treatment for severe obesity [1]. The three most commonly performed procedures are the laparoscopic Roux-en-Y gastric bypass (RYGB), the laparoscopic adjustable gastric banding (LAGB), and the laparoscopic sleeve gastrectomy (LSG). Although all three have been shown to be effective, each procedure has a unique risk/benefit profile [2, 3]. Most practices (including ours) offer objective information to patients in the form of classes or information session and then let the patients select the appropriate bariatric procedure. Patients ultimately choose the procedure based on collective information obtained from the seminar as well as from friends/family, independent research, and the preoperative surgeon consultation.
The purpose of this study was to better elucidate the factors affecting this decision-making process. Specifically, we investigated patients’ preferences based on a standardized questionnaire given to patients prior to surgeon consultation and the correlation with the procedure the patients ultimately choose. We hypothesized that there may be discordance in this process and that the procedure selection process may be ideal for shared decision making.
Materials and Methods
Study Sample
A bilingual (English/Spanish) questionnaire was distributed to all new bariatric surgery patients between March 1, 2012 and August 31, 2012. The questionnaire (Fig. 1) assessed patients’ knowledge of the RYGB, LAGB, and LSG, and how patients valued various treatment-related outcomes (maximum weight loss, curing diabetes, least weight regain, and fewest appointments) and complications (gastrointestinal leak and band slip or erosion) using a five-point Likert scale. Patient-level data was also recorded including age, sex, height, weight, and body mass index (BMI). The questionnaire was distributed to patients prior to the preoperative surgeon consultation.
Educational Seminar
Our program offers RYGB, LAGB, and LSG to patients who meet the 1991 NIH criteria for weight loss surgery [4]. We do not currently offer biliopancreatic diversion with/without duodenal switch (BPD/DS). All patients attend an educational seminar that educates patients on the differences in outcomes, follow-up appointments, and complication profile of the RYGB, LAGB, and LSG. The main learning objectives for the seminar include: (1) RYGB and LSG average greater weight loss compared to the LAGB; (2) LAGB requires the greatest number of postoperative follow-up appointments (i.e., monthly for the first year); (3) RYGB and LSG have a higher rate of life-threatening complications (e.g., leak) than LAGB; (4) LAGB has long-term device-related complications (e.g., slip, erosion); (5) RYGB has the highest rate of diabetes remission; and (6) there is a lack of data beyond 5 years regarding long-term weight loss after LSG.
Data Analysis
Data were reported as mean ± standard deviation or median and interquartile range. To determine whether a difference exists with age or body mass index (BMI) between the procedures, one-way analysis of variance tests with Tukey-Kramer post hoc tests were performed. To compare the proportions for race, sex, diabetes, and the most important outcome or concerning complication patients selected, the Fisher’s exact tests were carried out while maintaining a family error rate of α = 0.05. To compare patient values of outcomes and complications reported on the Likert scale, Kruskal-Wallis tests with Dunn’s post hoc tests were used. To determine whether having diabetes affected procedure choice, a multinomial logistic regression analysis was performed. Separate subgroup analysis was performed for patients with diabetes. For all tests, a value of p < 0.05 was considered statistically significant. This study had no external funding source.
Results
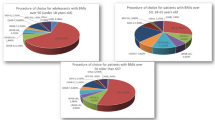
One hundred seventy-two patients completed the questionnaire. The majority of patients (81 %) were female, and average age and BMI were 40 years old and 44 kg/m2, respectively (see Table 1). The vast majority (90 %) of patients were Hispanic or non-Hispanic Black, reflecting the patient population of our urban safety-net hospital. There was no significant difference in age, BMI, diabetes status, sex, or race when patients were stratified by procedure.
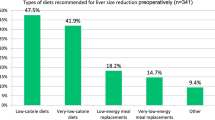
Based on the questionnaire, 62 % of the knowledge questions were answered correctly. Prior to the surgeon consultation (but after the seminar), 19 % of patients were unsure of which procedure they wanted. Most patients had already decided on the procedure prior to surgeon consultation (43 % RYGB, 41 % LSG, and 16 % LAGB; Fig. 2), reflective of the current case mix at our institution and nationwide trends in bariatric surgery [5].
Patient Preferences of Treatment-Related Outcomes
The overall median importance level for maximum weight loss and curing diabetes was 5 (IQR 5, 5) and that of least weight regain was 5 (IQR 4, 5) with no statistically significant difference between bariatric procedures. The most important outcomes for patients were maximum overall weight loss (58 %) followed by least chance of weight regain (29 %) (Table 2).
Patients who chose LSG seemed to preferentially value the decreased follow-up appointments compared to those who chose LAGB (p = 0.002). We also found that 52 % of patients choosing LAGB indicated that “maximum weight loss” was the most important, indicating a possible discordance between patient preferences and procedure selection.
Subgroup analysis of patients with diabetes revealed that most patients chose “curing diabetes” as the most important outcome, compared to “maximum weight loss” (58 vs. 33 %; Table 3). Specifically, patients who chose RYGB did so specifically for the diabetes effect of RYGB.
Patient Values of Complications
The overall median concern for gastrointestinal leak was 5 (IQR 3.25, 5) and that for band slip or erosion was 5 (IQR 3, 5). When patients were asked to select their most concerning complication overall, 65 % chose leak and 35 % slip or erosion (Table 4).
Discussion
There is very little data regarding how patients choose one bariatric procedure over another. Anecdotally, we have noticed that most patients have already selected the bariatric procedure prior to the surgeon consultation. This study was an attempt to help elucidate this decision-making process. We found that the vast majority of patients chose maximum weight loss as the most important outcome, that only 19 % of patients are unsure of what procedure they want prior to the surgeon consultation, and that patients with diabetes are more interested in diabetes remission than weight loss. Discordance likely exists between patient preferences and the procedure selected, i.e., other factors likely play a role in the decision making process.
Obese patients seeking bariatric surgery perceive obesity as a greater risk to their health compared to obese patients managed medically [6]. However, despite the fact that bariatric surgery patients seem to understand the benefits of surgery, they frequently have unrealistic expectations of weight loss [7, 8]. These baseline expectations are complicated by other factors (friends/family, internet, media, etc.) that influence the patients’ decision making process.
Since there are several reasonable options for patients seeking bariatric surgery (RYGB, LSG, and LAGB), patients should be involved in the determining the best procedure most consistent with his/her preferences and values. The preoperative educational seminar appears to be an ideal opportunity to educate patients objectively about the risks/benefits of the various bariatric procedures. Nevertheless, only 62 % of questions in this study were answered correctly, highlighting the challenges of educating a predominantly Hispanic and non-Hispanic Black population with high school education or less [9]. Video-based decision aids, which have been shown to be effective, may help address this issue [10].
On the other hand, the existing data regarding the effectiveness of the seminar is limited. A previous study evaluating the impact of the bariatric surgery education seminar on patient preferences found that only 11 % of patients changed procedure choice after attending the education seminar, implying that most patients have already decided on a procedure prior to coming to the educational seminar and preoperative surgeon visit [11]. Our study adds to this data as only 19 % of patients in our study were unsure about the procedure prior to the surgeon consultation.
Our study shows that there is discordance between what patients state is the most important outcome and the procedure that is ultimately selected. For instance, 52 % of patients who chose LAGB rated “maximum weight loss” as the most important outcome, despite the fact that most studies show RYGB and LSG have more weight loss than LAGB. There may be several reasons for this. First, the patients may not have an adequate understanding of the LAGB. However, not only are the weight loss differences emphasized in the seminar, but it is reiterated at the time of the surgeon consultation. Second, patients may be impacted by the experience of close friends or family members who had better than expected results with the LAGB. Third, and perhaps most likely, it is possible that the patients’ preference for the safety profile of the LAGB outweighed the goal of maximum weight loss [8, 12].
For instance, 65 % of LAGB patients stated leak was the most worrisome complication. This may reflect that for the patient, the safety profile of the band outweighed the risk of the leak from LSG or RYGB. On the other hand, 73 % of patients who chose LSG were most worried about leak. For these patients, the expected outcome likely outweighed their concern about leak. Similarly, patients who chose LSG may have done so to avoid dealing with the complication of band erosion. Given the nature of the questionnaire, it is not possible to discern this.
Clearly, there is a role for shared decision making in the bariatric surgery selection process. Shared decision making is a collaborative process between physicians and patients that facilitates joint decision making, taking into account current evidence as well as the patient’s values and preferences [13]. This would help counteract any patient biases and help the patient get the procedure that would be best given his/her values and preferences. Shared decision making may be more practical than a model or algorithm to determine the ideal bariatric procedure for a patient [14]. The education seminar and preoperative surgeon consultation are perhaps the best opportunities to integrate the shared decision making. However, future studies will need to assess the impact of other factors (friends/family, internet, media, etc.) on this decision making process.
One interesting finding of this study was that severely obese patients with diabetes mellitus displayed a different preference order for outcomes compared to those without diabetes: 58 % indicated diabetes remission was the most important outcome (compared to 33 % who indicated maximum weight loss was the most important). In particular, it appears that patients with diabetes who chose RYGB did so specifically for the diabetes effect of RYGB. This finding may help inform future research studies focusing on surgical treatment of diabetes.
There were several limitations to this study. The questionnaires were distributed after the educational seminar and before the surgeon consultation. Therefore, we were unable to objectively determine the impact of the seminar itself on the decision making process. We did not include BPD/DS in this study. Although BPD/DS is the most effective procedure for weight loss, it represents <1 % of bariatric procedures in the USA [15, 16]. Clearly, there are extraneous factors that affect the decision making process (family/friends, internet, media, etc.) We were unable to account for this. Future studies should incorporate these factors. Furthermore, although we were able to collect data about patients treatment-related preferences, we were unable to integrate these values (specifically outcomes and complications) to rationalize the procedure choice by the patient. Shared decision making would be ideal to incorporate these patient preferences with the existing medical literature to better deliver patient-centered care.
Conclusion
The decision to choose one bariatric procedure over another is complex and is based on factors beyond absolute patient preferences. This leads to discordance in the decision making process. Although maximum weight loss is a commonly reported preference for patients seeking bariatric surgery, patients with diabetes are more focused on diabetes improvement or resolution. The vast majority of patients have already decided which procedure to undergo prior to the surgeon consultation. Prospective bariatric surgery patients and physicians may benefit from shared decision making, which integrates patient values and preferences, along with current medical evidence, to assist in the complex bariatric surgery selection process.
References
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37.
Hutter MM, Schirmer BD, Jones D, et al. First report from the American College of Surgeons Bariatric Surgery Center Network: laparoscopic sleeve gastrectomy has morbidity and effectiveness positioned between the band and the bypass. Ann Surg. 2011;254(3):410–20.
Tice J, Karliner L, Walsh J, et al. Gastric banding or bypass? A systematic review comparing the two most popular bariatric procedures. Am J Med. 2008;121:885–93.
Gastrointestinal Surgery for Severe Obesity. NIH Consensus Statement, March 25–27, 9 (1991), pp. 1–20.
Nguyen N, Nguyen B, Gebhart A, et al. Changes in the makeup of bariatric surgery: a national increase in the use of laparoscopic sleeve gastrectomy. J Am Coll Surg. 2013;216:252–7.
Prasad C, Batsis J, Lopez-Jimenez F et al. Risk perception of obesity and bariatric surgery in patients seeking treatment for obesity. Eur J Prev Cardiol 2012 Nov 2.
Kaly P, Orellana S, Torrella T, et al. Unrealistic weight loss expectations in candidates for bariatric surgery. Surg Obes Relat Dis. 2008;4:6–10.
Apovian C, Huskey K, Chiodi S, et al. Patient factors associated with undergoing laparoscopic adjustable gastric banding vs. Roux-en-Y gastric bypass for weight loss. J Am Coll Surg. 2013;217:1118–25.
Parikh M, Dasari M, McMacken M, et al. Does a preoperative medically supervised weight loss program improve bariatric surgery outcomes? A pilot randomized study. Surg Endosc. 2012;26:853–61.
Arterburn D, Westbrok E, Bogart T, et al. Randomized trial of a video-based patient decision aid for bariatric surgery. Obesity. 2011;19:1669–75.
Taddeucci R, Madan A, Tichansky D. Band versus bypass: influence of an educational seminar and surgeon visit on patient preference. Surg Obes Rel Dis 2007;452-455.
Ren CJ, Cabrera I, Bajaram K, et al. Factors influencing patient choice for bariatric operation. Obes Surg. 2005;15:202–6.
Barry M, Edgman-Levitan S. Shared decision making—the pinnacle of patient-centered care. N Engl J Med. 2012;366:780–1.
Buchwald H. A bariatric surgery algorithm. Obes Surg. 2002;12:733–46.
Nelson D, Blair K, Martin M. Analysis of obesity-related outcomes and bariatric failure rates with the duodenal switch vs. gastric bypass for morbid obesity. Arch Surg. 2012;147:847–54.
DeMaria E, Pate V, Warthen M, et al. Baseline data from American Society for Metabolic and Bariatric Surgery Centers of Excellence using the bariatric outcomes longitudinal database. Surg Obes Relat Dis. 2010;6:347–55.
Acknowledgments
The authors would like to acknowledge Ashish Shaha, Research Data Associate, for his assistance with survey administration.
Conflict of interest disclosure statements
Weinstein, Marascalchi, Spiegel, Saunders, Fagerlin, and Parikh have no conflicts to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Weinstein, A.L., Marascalchi, B.J., Spiegel, M.A. et al. Patient Preferences and Bariatric Surgery Procedure Selection; the Need for Shared Decision-Making. OBES SURG 24, 1933–1939 (2014). https://doi.org/10.1007/s11695-014-1270-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-014-1270-6