Abstract
Background
The role of laparoscopic sleeve gastrectomy (LSG) has increased over the past 10 years. We present our results of patients who were 5 years out from surgery with regard to safety and long-term efficacy.
Methods
Retrospective analysis was carried out from prospectively collected data of patients who underwent LSG for morbid obesity. Bariatric Analysis and Reporting Outcome System (BAROS) and Food Tolerance Scores (FTS) were assessed. At 5 years, two lifestyle modification questions (regarding nutrition habits and physical fitness) were separately assessed.
Results
One hundred fourteen patients underwent LSG and were available for postoperative visits. Mean excess weight loss (EWL) was >65 % during the initial 3 years and declined to 45.3 % in 5 years. Of the patients, 71.92 % did not reach 50 % EWL at 60 months and were considered objective failures. BAROS and FTS scores were 7.15 and 4.32, and 23.5 and 22.5 at 30 and 60 months, respectively. Analyzing the 32 patients with EWL >50 % in the 5-year group, 26 (81.25 %) of them had scored ≥0.5 on the two lifestyle modification questions compared with 6 (18.75 %) that scored <0.5 (P < 0.001).
Conclusion
LSG is an effective bariatric surgical procedure with significant long-term (5 year) weight loss, resolution of comorbid medical conditions and significant improvement in the quality of life. The basis for this success, which must be always emphasized preoperatively by the bariatric team, is knowledge and implementation of better nutritional habits and increasing physical fitness or, in other words, in significant lifestyle modification.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of laparoscopic sleeve gastrectomy (LSG) has increased steadily over the past 10 years and is the most recently used surgical option for morbid obesity. The data emerging from studies demonstrate that LSG provides substantial weight loss and resolution of comorbidities after years of follow-up [1]. It has been shown to exhibit multiple advantages compared with other bariatric procedures. However, long-term clinical data on outcomes are limited at this time.
We aimed to review our results of patients who were 5 years out from surgery and assess the safety and long-term efficacy of LSG as a final approach for the treatment of morbidly obese patients. Besides an increased risk of morbidity and mortality, obesity often affects quality of life (QoL), and weight loss may improve health-related QoL [2]. Therefore, we also propose to determine QoL using the Bariatric Analysis and Reporting Outcome System (BAROS) score and attempt to characterize those with prolonged significant weight loss.
Methods
A retrospective chart review was completed on all patients who had undergone LSG between January 2007 and August 2008. The protocol was approved by the Institutional Review Board (IRB) of the Bnai-Zion Medical Center. All patients met the 1991 National Institutes of Health Consensus Conference guidelines for bariatric surgery with a BMI ≥ 40 kg/m2 or a BMI ≥ 35 kg/m2 with associated comorbidities. These were the same patients included in a previous study that assessed patients at 30 months after operation [3]. All patients that came to the 30-month visit were encouraged and were available for annual assessment.
All patients went through the same routine pre-bariatric examinations: blood tests, chest radiography, upper gastrointestinal (GI) series or endoscopy, electrocardiogram, abdominal ultrasound, and endocrinologic evaluation. Due to the distinctiveness of the clinic, a complete nutritional evaluation followed by consultation is performed on all patients, with the belief that one of the factors contributing to the success of the sleeve and all bariatric procedures is in implementing a healthy diet on the new stomach, and implementation is better when patients are prepared.
On their release from the surgery ward, patients received detailed medical and nutritional instructions on how to behave nutritionally and how to prepare themselves for life with their “new stomachs.”
During hospitalization and even after the patients’ release, the staff stays in close touch with all the patients who have been operated at our core. The support is 24/7 (24 h a day/7 days a week)—in web forums, internet groups, telephone and mail support, and regular clinic visits.
Surgical technique utilized a 39-French calibration bougie placed trans-orally along the lesser curvature and a stapled vertical gastrectomy performed parallel to this, starting at a minimum distance of 5 cm from the pylorus and leaving a sleeve volume of approximately 50 cm3. Staple-line reinforcement was performed by a running suture to prevent bleeding and leakage.
Weight loss was expressed as percent excess weight loss (EWL) based on the Metropolitan Life Tables [4]. BMI was also used to report weight loss, expressing percentage of excess BMI loss (%EBMIL). A BMI of 25 kg/m2 was the lowest limit of overweight. Therefore, calculation of the percentage of excess BMI lost was done with the help of the following formula: [(operative BMI − follow-up BMI) / (operative BMI − 25)] × 100 [5]. The use of this relative parameter is superior, because it is more descriptive and allows for objective comparisons among series. A threshold of 50 % EWL was used to group patients for comparison; a similar definition has been used by other investigators [6].
The QoL was assessed with the updated BAROS questionnaires, which were completed by all patients during annual assessment. It included the analysis of weight loss, improvements in obesity comorbidities, and changes in QOL. This scoring system analyzes these three domains, granting each of them 3 points to a maximum score of 9. The occurrence of complications and reoperations deducts points. The final score classifies the results into five outcome groups, from failure to excellent, establishing an objective definition of success (failure, <1; fair, >1–3; good, >3–5; very good, >5–7; and excellent, >7–9).
The Food Tolerance Score (FTS) was determined and compared between both groups [7]. The FTS was calculated based on a one-page questionnaire. The single-page questionnaire was divided in to four parts: (1) an overall assessment of the patient satisfaction about the quality of his/her alimentation, (2) questions about the timing of meals and nutrient intake between meals, (3) an evaluation of tolerance of eight different types of food, and (4) an evaluation of the frequency of vomiting/regurgitation. The score can vary between 1 and 27, 27 being the maximum for an excellent food tolerance.
At the 5-year follow-up visit, patients were required to answer an additional question: “Since performing surgery, solely regarding the fields of nutrition and physical fitness—have you significantly changed your way of life?”
Statistical Analysis
Results are expressed as mean ± standard error of the mean. Statistical evaluation was performed by a t test. The independent two-sample t test was applied for comparison of statistical significance, in which a P value was set at <0.05.
Results
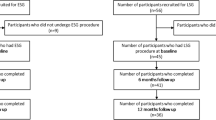
A total of 119 patients (87 female, 32 male) who underwent LSG as a first procedure and actively participated in the annual yearly postoperative follow-up visits were included for analysis (Table 1). Five patients were excluded from the study, because they underwent the second stage (biliopancreatic diversion) because of insufficient weight loss. The average age of the study group was 42.1 (range, 18–67) years, while the mean preoperative weight was 119.6 kg (range, 92.3–172.4). The average BMI was 44.1 kg/m2 (range, 35–52.3).
Weight Loss
At a follow-up point of 60 months, the mean %EWL was 45.3 ± 19.5 %. The changes in weight at follow-up periods are shown in Table 2. The mean %EWL was 65.5 % (range 25–110 %) at 12 months, 72 % (range 36–101 %) at 24 months, 76.8 % at 30 months (range 46–113 %), 68.3 % at 36 months (range 37–104 % ), 52 % at 48 months (range 25–101 %), and 45.3 % at 60 months (range 12–97 %).
Although the mean EWL was over 65 % during the initial 3 years, it declined to 45.3 % in 5 years. Eighty-two (71.92 %) patients did not reach to 50 % excess weight loss at the 60-month follow-up points, which, according to the Reinhold criteria, were considered objective failures [8]. The overall success rate (patients with %EWL > 50) was 74.56 % after 12 months, 68.42 % after 24 months, 70.17 % after 30 months, 57.01 % after 36 months, 44.73 % after 48 months, and 28.07 % after 60 months.
Weight loss as reported in Table 3 shows an important reduction of BMI observed in most patients at the 30- and 60-month follow-up. The %EBMIL at 30 months was 78.9 (±14.2) after 30 months and 49.1 (±19.6) at 60 months (P < 0.01). The BAROS scores for QoL were 7.15 and 4.32 at 30 and 60 months, respectively (P < 0.001). The FTS scores were 23.5 and 22.5 at the 30- and 60-month visits, respectively (P = N.S.).
Analysis of the distribution of the three parts in the final BAROS score is shown in Table 4. The median scores for weight loss were 2 and 1, medical conditions were 3 and 2, and quality of life were 2.1 and 1.5 at the 30- and 60-month visits, respectively.
Resolution of Comorbidities
During follow-up, there was significant improvement in the patients’ comorbidities (Table 5). Anti-diabetic medication was reduced or discontinued in 81.96 % of the patients, and 79.16 % of the patients no longer required or decreased antihypertensive agents. Eighty percent of the patients with sleep apnea withdrew from use of the continuous positive airway pressure (CPAP) mask and had marked decrease of apnea episodes. Other comorbidities such as joint pain and dyslipidemia exhibited the same significant results. Also to mention are GERD symptoms, which improved or resolved in 41 of 49 patients (83.67 %) at the 30-month visit, decreasing to 37 of 49 patients (67.34 %) at the 60-month visit.
At the 5-year visit, two questions from the BAROS questionnaire were separately assessed, and those were as follows: “The way I approach food is” with scores ranging from “I live to eat” till “I eat to live,” and the other question was “I enjoy physical activities” with scores ranging from “not at all” till “very much” with replies ranging on a scale from −0.5 to 0.5. These items were separated because they depict the basics of a healthy lifestyle. The other BAROS questions of “feeling good about myself,” “satisfactory social contacts,” “ability to work,” and “pleasure from sex” are much less relevant. We evaluated the group to which both these questions had a sum of ≥0.5 (termed lifestyle modification score).
This cutoff point exhibited significant correlation to the question we presented to all patients at the 5-year mark: “Since performing surgery, solely regarding the fields of nutrition and physical fitness—have you significantly changed your way of life?” All patients answering “yes” to this question had scored ≥0.5 on the BAROS questionnaire. Figure 1 clearly shows the significant changes of the lifestyle modification score during the yearly follow-up visits.
Analyzing the 32 patients with EWL > 50 % at 5-years, 26 (81.25 %) of them had scored ≥0.5 on those two questions compared with 6 (18.75 %) that scored <0.5 (P < 0.001). None of the patients from the EWL <50% group had scored ≥5 in the lifestyle modification score.
Discussion
In this study, we report on a 5-year follow-up of 114 patients after sleeve gastrectomy. These are the first 114 patients undergoing LSG in our center. Other bariatric procedures performed were mainly primary biliopancreatic diversion, without the same follow-up period. No gastric bandings are performed in our center. The Bariatric Gastroenterology Clinic under the auspices of a specialist in gastroenterology and nutrition is fully committed to the ongoing care and follow-up of all bariatric patients in our medical center. This unique clinic encompasses the areas of bariatric complications, nutritional assessment and follow-up, and other gastrointestinal disorders.
The aim of the current study was to assess the long-term efficacy and safety of laparoscopic sleeve gastrectomy as the intended first (and final) surgical intervention in patients with morbid obesity. Significant weight regain was noted in our patient population after 5 years of follow-up evaluation. This has been described in other papers; to note is the comment to the paper by Himpens et al. which concluded that overall objective failure rates of laparoscopic sleeve gastrectomy were 47 and 64 % at years 3 and 6, respectively [6, 9]. This trend was also noted by Strain et al., showing that mean BMI was 35 ± 7.6 kg/m2 at 3 years and 40 ± 8.1 kg/m2 at 5 years [10]. EWL was 70 % during the initial 3 years (mean follow-up rate 90.5 %), with a gradual decline to 57.6 % by 5 years [11].
The 3rd International Summit for LSG, reporting on the results of 19,605 SG procedures, published that the mean %EWL at 5 years was 60 % from noncontrolled reports [12]. In an additional study reviewing cases after 6 years, EWL had dropped to 57.3 % [6], and the most recent paper concluded that mean percentage excess weight loss was 71.96 ± 21.30 % at 3 years and 63.71 ± 20.08 % at 5 years [13].
Possible reasons for weight regain tendency are sleeve dilation [14] and the complex neurohormonal changes post SG that are not fully understood [15]. Others attributed it to the loss of appetite suppression that occurs after surgery. The removal of the ghrelin-secreting gastric fundus [16] and afterwards that suppression is eventually overcome by hyperactivation of previously silent ghrelin-producing cells distributed throughout the gastrointestinal tract [17].
Active participation in follow-up visits and loss of continuous support is likely to play an important role in weight regain as well [3, 6]. Using the lifestyle modification score, we have demonstrated in our study that sufficient weight loss at the 5-year mark was associated with successful change in patient’s life style. Weight regain, resulting in a gradual decline of the percentage of EWL in our series, was mainly attributed to the two main factors: bad nutrition habits and lack of exercise in later years after the procedure. Further analysis of patients with insufficient 5-year weight loss revealed two groups. There are patients that after surgery adhered to the necessary changes and, with time, ceased to do so and therefore primarily lost and then gained weight, and the other group, which did not make any of the changes at first and therefore exhibited insufficient weight loss. For long-term success, all patients should be strongly advised to alter their lifestyle patterns for life.
As stated, only 28.07 % of patients had lost over 50 % of the EWL at 5 years. Compared to nonsurgical options, LSG is still the best option for successful treatment of morbid obesity without going into the field of malabsorptive surgery. LSG is a good tool for people really wanting to change their way of lives and lose weight in a healthy manner.
The remaining 72 % have the option of performing a duodenal switch or select a healthier option of adhering to lifestyle modification without a second surgery, something they have failed before and therefore primarily went for operation. However, chances of success after the 5-year mark without surgery are not very high.
Statistically significant improvement in pre-existing obesity-related comorbidities was achieved in our study, comparable with that described in other series [18, 19]. We noticed a good resolution of main commodities even at the 60-month follow-up period, although there was a tendency for fewer patients in remission when comparing the 30- and 60-month data.
The BAROS score summarizes weight loss, correction of comorbidities, improvement of QoL, and complications. The QoL improved dramatically in the first years which compares favorably with most other bariatric procedures, but at the 5-year point, it declined. The mean BAROS score was 7.15 ± 0.8 at 2.5 years and 4.32 ± 0.9 at 5 years. We noted that the main reason for this decline was the long-term weight gain.
Our unique clinic emphasizes the importance of follow-up and constant online contact as one of the main factors leading to the success of the sleeve. For all of the 114 patients, there were data for the 30- and 60-month visits. When patients could not come to clinic visits, we were able to reach them by phone, and their weights, BAROS, and FTS assessment were based on self-reports. The International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) published guidelines for the safety, quality, and excellence in bariatric surgery [20]. It stated that along with the surgical issues, the centers of excellence of a bariatric institution should provide lifetime follow-up for the majority of all the patients undergoing bariatric surgery. A recent paper addressing the issues of health behavior, food tolerance, and satisfaction after laparoscopic sleeve gastrectomy underlines the importance of long-term maintenance programs [21]. We take this one step further in providing round-the-clock support to whatever outcome might arise. If patients do not have this appropriate round-the-clock professional support, then the sleeve and its success are at risk. The high percentage of patients with follow-up data emphasizes this effect.
Our study is limited by its retrospective nature and small sample size. Although data was not obtained from a prospective trial, all patients included were available for reporting purposes. Most other studies showed a low number of patients followed up at over 5 years, some with only 23 patients (27.7 %) reaching the 6-year follow-up point [15, 22, 23]. Our large percentage of follow-up data emphasizes the Bariatric Gastroenterology Clinic which is fully committed to the ongoing care and follow-up of all bariatric patients in our medical center, and diligent about contacting patients who do not follow-up call them to reestablish care.
Conclusion
LSG is an effective bariatric surgical procedure with significant long-term (5 year) weight loss, resolution of comorbid medical conditions and improvement in QoL. The basis for this success, which must be always emphasized preoperatively by the bariatric team, is knowledge and implementation of better nutritional habits and increasing physical fitness or, in other words, in significant lifestyle modification.
References
James PT, Rigby N, Leach R. International Obesity Task Force—the obesity epidemic, metabolic syndrome and future prevention strategies. Eur J Cardiovasc Prev Rehabil. 2004;11(1):3–8.
Dymek MP, Le Grange D, Neven K, et al. Quality of life and psychosocial adjustment in patients after Roux-en-Y gastric bypass: a brief report. Obes Surg. 2001;11(1):32–9.
Keren D, Matter I, Rainis T, et al. Getting the most from the sleeve: the importance of post operative follow-up. Obes Surg. 2011;21:1887–93.
Deitel M, Gawdat K, Melissas J. Reporting weight loss. Obes Surg. 2007;17:565–8.
Deitel M, Greenstein RJ. Recommendations for reporting weight loss. Obes Surg. 2003;13:159–60.
Himpens J, Dobbeleir J, Peeters G. Long-term results of laparoscopic. Ann Surg. 2010;252:319–24.
Suter M, Calmes JM, Paroz A, et al. A new questionnaire for quick assessment of food tolerance after bariatric surgery. Obes Surg. 2007;17:2–8.
Reinhold RB. Critical analysis of long-term weight loss following gastric bypass. Surg Gynecol Obstet. 1982;155:385–94.
Heath V. Laparoscopic sleeve gastrectomy as the first-line surgical option for morbid obesity. Nat Rev Endocrinol. 2010;6(10):534.
Strain GW, Saif T, Gagner M, et al. Cross-sectional review of effects of laparoscopic sleeve gastrectomy at 1, 3, and 5 years. Surg Obes Relat Dis. 2011;7(6):714–9.
Kehagias I, Spyropoulos C, Karamanakos S, et al. Efficacy of sleeve gastrectomy as sole procedure in patients with clinically severe obesity (BMI ≤50 kg/m(2)). Surg Obes Relat Dis. 2013;9(3):363–9.
Deitel M, Gagner M, Erickson AL, et al. Third International Summit: current status of sleeve gastrectomy. Surg Obes Relat Dis. 2011;7:749–59.
Zachariah SK, Chang PC, Ooi AS, et al. Laparoscopic sleeve gastrectomy for morbid obesity: 5 years experience from an Asian center of excellence. Obes Surg. 2013;23(7):939–46.
Langer FB, Bohdjalian A, Felberbauer FX, et al. Does gastric dilatation limit the success of sleeve gastrectomy as a sole operation for morbid obesity? Obes Surg. 2006;16(2):166–71.
D’Hondt M, Vanneste S, Pottel H, et al. Laparoscopic sleeve gastrectomy as a single-stage procedure for the treatment of morbid obesity and the resulting quality of life, resolution of comorbidities, food tolerance, and 6-year weight loss. Surg Endosc. 2011;25(8):2498–504.
Wang Y, Liu J. Plasma ghrelin modulation in gastric band operation. Obes Surg. 2009;19:357–62.
Karamanakos SN, Vagenas K, Kalfarentzos F, et al. Weight loss, appetite suppression, and changes in fasting and postprandial ghrelin and peptide-YY levels after Roux-en-Y gastric bypass and sleeve gastrectomy: a prospective, double blind study. Ann Surg. 2008;247(3):401–7.
Frezza EE, Chiriva-Internati M, Wachtel MS. Analysis of the results of sleeve gastrectomy for morbid obesity and the role of ghrelin. Surg Today. 2008;38(6):481–3.
Gumbs AA, Gagner M, Dakin G, et al. Sleeve gastrectomy for morbid obesity. Obes Surg. 2007;17(7):962–9.
Melissas J. IFSO Guidelines for safety, quality, and excellence in bariatric surgery. Obes Surg. 2008;18:497–500.
Kafri N, Valfer R, Nativ O, et al. Health behavior, food tolerance, and satisfaction after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2011;7(1):82–8.
Sarela AI, Dexter SP, O’Kane M, et al. Long-term follow-up after laparoscopic sleeve gastrectomy: 8-9-year results. Surg Obes Relat Dis. 2012;8(6):679–84.
Bohdjalian A, Langer FB, Shakeri-Leidenmühler S, et al. Sleeve gastrectomy as sole and definitive bariatric procedure: 5-year results for weight loss and ghrelin. Obes Surg. 2010;20(5):535–40.
Conflict of Interest
Dr. Dean Keren, Dr. Ibrahim Matter, and Prof. Alexandra Lavy have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare no support from any organization for the submitted work, no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years, and no other relationships or activities that could appear to have influenced the submitted work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Keren, D., Matter, I. & Lavy, A. Lifestyle Modification Parallels to Sleeve Success. OBES SURG 24, 735–740 (2014). https://doi.org/10.1007/s11695-013-1145-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-013-1145-2