Abstract
Background
Morbidly obese (MO) patients are at increased risk for postoperative anesthesia-related complications. We evaluated the role of sugammadex versus neostigmine in the quality of recovery from profound rocuronium-induced neuromuscular blockade (NMB) in patients with morbid obesity.
Methods
We studied 40 female MO patients who received desflurane and remifentanil anesthesia for laparoscopic removal of adjustable gastric banding. NMB was achieved with rocuronium. At the end of the surgical procedure, complete reversal of NMB was obtained with sugammadex (SUG group, n = 20) or neostigmine plus atropine (NEO group, n = 20) in the presence of profound NMB.
Results
No difference in surgical time or anesthetic drugs was found between the groups. Anesthesia time was significantly greater in the NEO group than in the SUG group (95 ± 21 vs. 47.9 ± 6.4 min, p < 0.0001), which was mainly due to a longer time to reach a train-of-four ratio (TOFR) ≥ 0.9 in the NEO group (48.6 ± 18 vs. 3.1 ± 1.3 min, p < 0.0001) during reversal of profound NMB. Upon admission to the postanesthesia care unit, level of SpO2 (p = 0.018), TOFR (p < 0.0001), ability to swallow (p = 0.0027), and ability to get into bed independently (p = 0.022) were better in the SUG group than in the NEO group. Patients in the SUG group were discharged to the surgical ward earlier than patients in the NEO group were (p = 0.013).
Conclusions
Sugammadex allowed a safer and faster recovery from profound rocuronium-induced NMB than neostigmine did in patients with MO. Sugammadex may play an important role in fast-track bariatric anesthesia
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Performing bariatric surgery as a short-stay procedure is an ongoing trend in many centers [1]. For morbidly obese (MO) patients, the anesthesiological approach is based on choosing anesthetic drugs that have the least potential for accumulation. This allows a more rapid and clear-headed recovery and contributes to reduced duration of perioperative time [1, 2]. When neuromuscular blocking agents (NMBAs) are required, complete recovery from neuromuscular blockade (NMB) is crucial for fast-track discharge. Even small degrees of postoperative residual curarization (PORC) increase the incidence of critical respiratory events (CREs) in the postanesthesia care unit (PACU) [3], which is associated with delayed PACU discharge [4]. Traditionally, reversal of NMB is achieved using acetylcholinesterase (AChE) inhibitors. Sugammadex is a recently identified reversal agent that may allow quicker reversal of rocuronium-induced NMB [5]. In MO patients, sugammadex administered at the reappearance of T2 rapidly and effectively reverses rocuronium-induced NMB and prevents PORC [6]. We evaluated the role of sugammadex versus neostigmine during recovery from profound rocuronium-induced NMB in MO patients undergoing bariatric surgery.
Materials and Methods
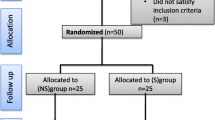
A total of 40 MO patients [body mass index (BMI) ≥ 40 kg/m2] scheduled for elective laparoscopic removal of adjustable gastric banding (AGB) under general anesthesia were evaluated. Approval from the Ethics Committee for Clinical Research (Padova Medical Hospital, Padua, Italy) and informed written consent were obtained. Inclusion criteria were age ≥18 years, scheduled laparoscopic removal of AGB under general anesthesia using rocuronium for tacheal intubation and maintenance of NMB, and presence of one to five posttetanic counts (PTCs) at the end of surgery. Exclusion criteria were American Society of Anesthesiolgists physical status >3, difficult tracheal intubation, known or suspected disorder affecting NMB, renal and/or hepatic dysfunction, malignant hyperthermia, pregnancy, breastfeeding, and allergy or contraindication to narcotics, NMBAs, sugammadex, neostigmine, or other medications used during anesthesia.
Patients were randomly assigned to reversal from NMB with either sugammadex (4 mg/kg total body weight; SUG group) or neostigmine [70 μg/kg lean body weight (LBW); total dose ≤5 mg] plus atropine (10 μg/kg; total dose ≤1 mg; NEO group) in the presence of one to five PTCs (deep NMB) at the end of the surgical procedure. Randomization was achieved using computer-generated numbers and allocation by opening a sealed opaque envelope immediately before surgery by one investigator (CO).
Patients were premedicated with intravenous administration of midazolam 0.05 mg/kg (ideal body weight, IBW) and ranitidine 50 mg. Monitoring and ventilation were established by using the Datex-Ohmeda Aisys workstation (Aisys GE Healthcare, Datex-Ohmeda, Milan, Italy). Neuromuscular function was monitored by acceleromyography (AMG; TOF-Watch®SX, Organon Teknik, Ireland) at the adductor pollicis muscle starting after induction of anesthesia (before rocuronium administration) with calibration and stabilization of the signal as recommended by the manufacturer, which continued at least until recovery of the train-of-four ratio (TOFR) ≥ 0.9. The arm with AMG was fixed to an armboard and the thumb was allowed to move freely without preload. Patients were preoxygenated for 3 min. Anesthesia was induced intravenously with fentanyl 3.5 μg/kg (LBW) and propofol 3 mg/kg (LBW) and was mantained with desflurane and remifentanil 0.05–0.1 μg/kg/min titrated to a target state entropy value of 35 ± 5. Tracheal intubation was achieved for each patient after receiving rocuronium 0.9 mg/kg (IBW). IBW was determined by the methods of Matsuzawa et al. and Lemmens et al. with slight modifications [7]. Maintenance doses of rocuronium 0.15 mg/kg were given as required during surgery. PTC stimulation was started after the T1 response disappeared on the TOF stimulation mode. Spontaneous recovery was allowed to progress until the reappearance of one to five PTCs at the end of surgery. TOF stimulation mode was re-established at ≥6 PTCs. Patients received only rocuronium for NMB and a single dose of either neostigmine or sugammadex for reversal. Remifentanil was stopped after the end of carboperitoneum, and ondansetron 4 mg, dexamethasone 4 mg, and ketoprofen 100 mg were given intravenously to reduce postoperative nausea and vomiting (PONV) and limit the use of narcotics for postoperative pain management. Ventilatory support and anesthesia were maintained until recovery of neuromuscular function to TOFR ≥0.9 and when the anesthesiologist judged the patient as ready for tracheal extubation.
After tracheal extubation, patients were placed in 60° upright position and transferred to the PACU within 10 min. Respiratory rate and pulse oximetry were monitored continuously until discharge to the surgical ward. Patients were assessed every 5 min for level of consciousness (awake and oriented, arousable with minimal stimulation, or responsive only to tactile stimulation), general muscle weakness (head tilting and hand squeezing, ability to independently transfer from surgery table to bed), clinical evidence of PORC or reoccurrence of NMB (muscle weakness, inability to swallow 20 ml water, oxygen desaturation, CREs), and pain and incidence of PONV with visual analog scale pain/nausea scores (0 = no pain/nausea, 10 = worst possible pain/nausea). An acceleromyographic low stimulation current (30 mA) was applied to evaluate TOFR at PACU admission to check the degree of residual NMB. If CREs related to residual NMB occurred, a rescue dose of sugammadex (2 mg/kg) was given. Patients who reported a pain score >3 received rescue analgesics (paracetamol, 1 g intravenously). Patients who suffered PONV received a rescue dose of ondansetron 4 mg intravenously.
Surgery duration was calculated as the time from skin incision to the placement of the last stitch. Anesthesiology times were calculated as follows: (1) anesthesia: time from preoxygenation of patient to tracheal extubation, (2) induction: time from the end of preoxygenation to tracheal intubation, (3) maintenance: time from tracheal intubation to the beginning of reversal of NMB, (4) reversal: time from reversal of drug administration to TOFR ≥ 0.9, and (5) extubation: time from cessation of desflurane after recovery from NMB to tracheal extubation.
The primary endopoint was the difference in anesthesia time between the groups. The secondary endpoints included differences in oxygen saturation levels and TOFR upon PACU admission and ability to swallow after extubation. We based the sample size calculation on the primary and secondary endopoints as clinical signs of adequate or inadequate recovery from NMB. Based on a previous ten MO patients, we calculated (α = 0.05 and β = 0.10) that three patients for the primary endpoint and 17 patients for the secondary endpoints were required for each group to detect a significant intergroup difference. To account for possible dropouts, 20 patients for each group were included. Patients were also assessed for clinical evidence of residual and/or recurrence of NMB based on neuromuscular monitoring and clinical assessment. Postoperative complications, analgesic and antiemetic requirements, ability to get into bed independently, and time to discharge from PACU were also considered. The safety assessor (SV) was not involved in the randomization process and was not present during anesthesia. Anesthesia was performed by a single anesthetist (MC) and the surgeon was the same for all surgical procedures (MF).
Continuous data were reported as median ± standard deviation and compared using Student's t-test. Categorical data were reported as the absolute number with percentages and compared with χ 2 test or Fisher's exact test. Kaplan–Meier estimate-of-survival curve was used to determine the cumulative probability of TOFR < 0.9 after administration of reversal drugs in the following 90 min and to discharge the patient from the PACU within 2 h. Curves between the two groups were compared using the log-rank test. A P value <0.05 was considered statistically significant. Analyses were performed using SAS 9.2 statistical software (SAS Institute Inc., Cary, NC, USA).
Results
Of the 40 patients recruited in the study, 20 patients were allocated to the NEO group and 20 patients to the SUG group. Patients' demographic characteristics are reported in Table 1. Anesthetic drug dosages, surgical and anesthesiology times, and characteristics of recovery are shown in Table 2. Maintenence doses of rocuronium were admistered to four patients in the SUG group and three patients in the NEO group. No differences were observed for drug dosage, depth of anesthesia, or duration of surgery. However, the anesthesia time was significantly greater in the NEO group than the SUG group (p < 0.0001), which was mainly due to a longer time to reach TOFR ≥ 0.9 in the NEO group (p < 0.0001). All patients in the SUG group recovered to TOFR ≥ 0.9 within 6 min of administration of sugammadex. In contrast, 75 % of patients in the NEO group recovered between 30 and 60 min after administration of neostigmine, with 20 % requiring more than 60 min to recover to TOFR ≥ 0.9. The cumulative probability of TOFR < 0.9 after administration of reversal drug in the following 90 min was greater in the NEO group than in the SUG group (p < 0.0001; Fig. 1). At PACU admission, level of SpO2 (p = 0.018), TOFR (p < 0.0001), and ability to swallow after extubation (p = 0.0027) were better in the SUG group than in the NEO group (Table 3). Patients in the SUG group were able to independently get into bed quicker than patients in the NEO group (p < 0.0001; Table 3). The cumulative probability to discharge to the surgical ward greater than 2 h after the beginning of anesthesia was significantly higher for the NEO group than for the SUG group (p < 0.0001; Fig. 2). In the NEO group, four patients received a second dose of atropine for a heart rate <50 beats/min after reversal of anesthesia.
Eight patients in the NEO group and two patients in the SUG group had a decrease of >4 % of SpO2 versus baseline (SpO2 > 90 %), and three patients in the NEO group required transitory oxygen supplementation and a rescue dose of sugammadex for CREs after extubation. No differences were observed for pain scores and the use of rescue drugs for postoperative pain between the groups; however, the NEO group had a higher PONV score (p = 0.015; Table 3).
Discussion
We observed that sugammadex provided a faster and safer recovery from profound NMB than neostigmine in MO patients did. This effect was primarily mediated by the reduced duration of anesthesia times and postoperative monitoring after desflurane anesthesia.
Sugammadex produces a significantly more rapid recovery from rocuronium-induced profound NMB than neostigmine does [5, 8]. Neostigmine acts by inactivating the enzyme AChE in the synaptic cleft of the neuromuscular junction (NMJ) [8], allowing ACh to accumulate and displace rocuronium from its nicotinic receptor binding sites [8]. However, in the presence of high concentrations of rocuronium, increased ACh concentrations are insufficient to displace enough rocuronium to reverse NMB [5, 8–10]. Even if administered at high doses (70 μg/kg), neostigmine cannot completely reverse profound NMB [8–10]. Furthermore, the reversing effects of neostigmine appear within 1–2 min of administration and reach a maximum effect within 6–10 min [10, 11]. Subsequently, decreased concentrations of neostigmine occur through redistribution, metabolism, and excretion, allowing AChE activity to return to normal levels and reducing Ach concentrations [8–10] when rocuronium is still present in the synaptic cleft of the NMJ [9, 10]. If neostigmine fails to bring about a recovery of TOFR to >0.9 within 10 min, it is necessary to wait for a spontaneous recovery from NMB [8–10], which can be delayed by several factors, including obesity, individual genetic differences, female gender, age, organ dysfunction, and use of inhalation anesthesia. [10, 12, 13]. Sugammadex acts by encapsulating and inactivating unbound rocuronium and forming tight 1:1 complexes, providing a rapid and complete reversal of rocuronium-induced NMB independent of the agent used for maintenance anesthesia. [5, 13–15].
Postoperative recovery of TOFR to 0.9 does not exclude an impairment of neuromuscular transmission [16] and may also be associated with muscle weakness [16], inhibition of the hypoxic–ventilatory response [17], and upper airway [18] or pharyngeal dysfunction [19]. All of these aspects may have occurred in patients of the NEO group despite recovery of TOFR ≥ 0.9 as detected by AMG [3, 20]. Indeed a baseline TOFR measured by AMG is usually higher than 1.0 and varies widely among patients [21]. If normalized by the baseline value, the TOFR observed upon PACU admission in some patients in the NEO group may not have represented an adequate recovery of neuromuscular function, and residual paralysis may still have been present after recovery from profound NMB with neostigmine [20, 21]. Furthermore, neostigmine has a shorter half-life than rocuronium does, such that the rocuronium molecule may bind again to the nicotinic receptors [6]. Consequently, sugammadex represents a better pharmacological approach to quickly reach the threshold TOFR of 1.0 when AMG is used before proceeding with tracheal extubation in MO patients and to reduce the risk of PORC [21–23].
In general, the effect of residual NMB may be increased during early recovery after general anesthesia [24]. Desflurane has been suggested as the preferred inhaled anesthetic in MO patients because of its more rapid and consistent recovery profile [25–27]. This advantage of desflurane is associated with reduced incidence of desaturation [25, 26], faster recovery of protective airway reflexes [28], and improvement in patient mobility in the postoperative period [25, 26]. Increasing the BMI and the duration of anesthesia may impair such an uneventful recovery [28]. In fact, after ceasing its administration, desfurane levels decrease rapidly within 5 min, but a tail of desflurane levels may persist [27], the degree of which is proportional to the duration of anesthetic exposure [27–29]. Desflurane is a general anesthetic with affinity for nicotinic receptors [30]. Even in seemingly awake patients, small minimum alveolar concentration fractions of anesthetic can blunt the hypoxic–ventilatory response and impair vital protective functions during early recovery, thereby increasing the risk of CREs (i.e., severe desaturation, airway obstruction, hypoventilation, and pulmonary aspiration) [28]. Thus, reducing anesthesia time by means of a more rapid and complete reversal of profound NMB allows for shortened anesthetic exposure and a smaller tail after extubation [27–29].
Optimal management of pain and PONV after laparoscopic surgical procedures is a prerequisite for fast discharge of MO patients [31]. The recourse to nonsteroidal antinflammatory analgesics alone or in combination with other nonopioid analgesics is strongly recommended for pain relief and reduction of opioid consumption, thus alleviating the opioid-related adverse effect of respiratory depression in MO patients [32]. Minimizing intraoperative and postoperative use of opioids and the multi-model treatment approach to PONV are also recommended, particularly in case of inhalational anesthesia [33]. High doses of neostigmine should be avoided to the extent possible because neostigmine increases PONV and use of antiemetic drugs during the first 6 h after administration [34, 35].
In conclusion, sugammadex facilitates a rapid and complete recovery from profound NMB, minimizes the risk of PORC, and allows quicker return to mobility for MO patients. In associaton with rapid short-acting volatile anesthetics and opioids, sugammadex facilitates bariatric fast-track surgery.
References
Raeder J. Bariatric procedures as day/short stay surgery: is it possible and reasonable? Curr Opin Anaesthesiol. 2007;20(6):508–12.
Servin F. Ambulatory anesthesia for the obese patient. Curr Opin Anaesthesiol. 2006;19(6):597–9.
Murphy GS, Szokol JW, Marymont JH, et al. Residual neuromuscular blockade and critical respiratory events in the postanesthesia care unit. Anesth Analg. 2008;107(1):130–7.
Butterly A, Bittner EA, George E, et al. Postoperative residual curarization from intermediate-acting neuromuscular blocking agents delays recovery room discharge. Br J Anaesth. 2010;105(3):304–9.
Jones RK, Caldwell JE, Brull SJ, et al. Reversal of profound rocuronium-induced blockade with sugammadex: a randomized comparison with neostigmine. Anesthesiology. 2008;109(5):816–24.
Gaszynski T, Szewczyk T, Gaszynski W. Randomized comparison of sugammadex and neostigmine for reversal of rocuronium-induced muscle relaxation in morbidly obese undergoing general anaesthesia. Br J Anaesth. 2012;108(2):236–9.
Carron M, Guzzinati S, Ori C. Simplified estimation of ideal and lean body weights in morbidly obese patients. Br J Anaesth. 2012;109(5):829–30.
Bartkowski RR. Incomplete reversal of pancuronium neuromuscular blockade by neostigmine, pyridostigmine, and edrophonium. Anesth Analg. 1987;66(7):594–8.
Kopman AF. Neostigmine versus sugammadex: which, when, and how much? Anesthesiology. 2010;113(5):1010–1.
Suzuki T, Masaki G, Ogawa S. Neostigmine-induced reversal of vecuronium in normal weight, overweight and obese female patients. Br J Anaesth. 2006;97(2):160–3.
Leykin Y, Miotto L, Pellis T. Pharmacokinetic considerations in the obese. Best Pract Res Clin Anaesthesiol. 2011;25(1):27–36.
Debaene B, Plaud B, Dilly MP, et al. Residual paralysis in the PACU after a single intubating dose of nondepolarizing muscle relaxant with an intermediate duration of action. Anesthesiology. 2003;98(5):1042–8.
Carron M, Parotto E, Ori C. Prolonged neuromuscular block associated to non-alcoholic steatohepatitis in morbidly obese patient: neostigmine versus sugammadex. Minerva Anestesiol. 2012;78(1):112–3.
Vanacker BF, Vermeyen KM, Struys MM, et al. Reversal of rocuronium-induced neuromuscular block with the novel drug sugammadex is equally effective under maintenance anesthesia with propofol or sevoflurane. Anesth Analg. 2007;104(3):563–8.
Duvaldestin P, Kuizenga K, Saldien V, et al. A randomized, dose-response study of sugammadex given for the reversal of deep rocuronium- or vecuronium-induced neuromuscular blockade under sevoflurane anesthesia. Anesth Analg. 2010;110(1):74–82.
Eikermann M, Gerwig M, Hasselmann C, et al. Impaired neuromuscular transmission after recovery of the train-of-four ratio. Acta Anaesthesiol Scand. 2007;51(2):226–34.
Igarashi A, Amagasa S, Horikawa H, et al. Vecuronium directly inhibits hypoxic neurotransmission of the rat carotid body. Anesth Analg. 2002;94(1):117–22.
Eikermann M, Vogt FM, Herbstreit F, et al. The predisposition to inspiratory upper airway collapse during partial neuromuscular blockade. Am J Respir Crit Care Med. 2007;175(1):9–15.
Eriksson LI, Sundman E, Olsson R, et al. Functional assessment of the pharynx at rest and during swallowing in partially paralyzed humans: simultaneous videomanometry and mechanomyography of awake human volunteers. Anesthesiology. 1997;87(5):1035–43.
Carron M, Freo U, Ori C. Sugammadex for treatment of postoperative residual curarization in a morbidly obese patient. Can J Anaesth. 2012;59(8):813–4.
Suzuki T, Fukano N, Kitajima O, et al. Normalization of acceleromyographic train-of-four ratio by baseline value for detecting residual neuromuscular block. Br J Anaesth. 2006;96(1):44–7.
Plaud B, Debaene B, Donati F, et al. Residual paralysis after emergence from anesthesia. Anesthesiology. 2010;112(4):1013–22.
Carron M, Parotto E, Ori C. The use of sugammadex in obese patients. Can J Anaesth. 2012;59(3):321–2.
Freo U, Carron M, Innocente F, et al. Effects of A-line Autoregression Index (AAI) monitoring on recovery after sevoflurane anesthesia for bariatric surgery. Obes Surg. 2011;21(7):850–7.
Juvin P, Vadam C, Malek L, et al. Postoperative recovery after desflurane, propofol, or isoflurane anesthesia among morbidly obese patients: a prospective, randomized study. Anesth Analg. 2000;91(3):714–9.
Strum EM, Szenohradszki J, Kaufman WA, et al. Emergence and recovery characteristics of desflurane versus sevoflurane in morbidly obese adult surgical patients: a prospective, randomized study. Anesth Analg. 2004;99(6):1848–53.
La Colla L, Albertin A, La Colla G, et al. Faster wash-out and recovery for desflurane vs sevoflurane in morbidly obese patients when no premedication is used. Br J Anaesth. 2007;99(3):353–8.
McKay RE, Malhotra A, Cakmakkaya OS, et al. Effect of increased body mass index and anaesthetic duration on recovery of protective airway reflexes after sevoflurane vs desflurane. Br J Anaesth. 2010;104(2):175–82.
Bailey JM. Context-sensitive half-times and other decrement times of inhaled anesthetics. Anesth Analg. 1997;85(3):681–6.
Paul M, Fokt RM, Kindler CH, et al. Characterization of the interactions between volatile anesthetics and neuromuscular blockers at the muscle nicotinic acetylcholine receptor. Anesth Analg. 2002;95(2):362–7.
Douglas WW, Kehlet H. Management of patients in fast track surgery. BMJ. 2001;322(7284):473–6.
Chung SA, Yuan H, Chung F. A systemic review of obstructive sleep apnea and its implications for anesthesiologists. Anesth Analg. 2008;107(5):1543–63.
Gan TJ, Meyer T, Apfel CC, et al. Consensus guidelines for managing postoperative nausea and vomiting. Anesth Analg. 2003;97(1):62–71.
Paraskeva A, Papilas K, Fassoulaki A, et al. Physostigmine does not antagonize sevoflurane anesthesia assessed by bispectral index or enhances recovery. Anesth Analg. 2002;94(3):569–72.
Løvstad RZ, Thagaard KS, Berner NS, et al. Neostigmine 50 microg kg(−1) with glycopyrrolate increases postoperative nausea in women after laparoscopic gynaecological surgery. Acta Anaesthesiol Scand. 2001;45(4):495–500.
Grant Information
The authors are supported by departmental funds only.
Implication
Findings from this study were presented as a poster at the 2012 International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) in New Delhi, India [Obes Surg 2012; 22: 1315-1419 (P034)].
Conflict of Interest
Michele Carron has received a payment for lecture from MSD; Mirto Foletto has received a payment for consultancy from Johnson & Johnson Medical; Carlo Ori has received payments and travel fundings for lectures and as a member of MSD Advisory Board.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Carron, M., Veronese, S., Foletto, M. et al. Sugammadex Allows Fast-Track Bariatric Surgery. OBES SURG 23, 1558–1563 (2013). https://doi.org/10.1007/s11695-013-0926-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-013-0926-y