Abstract
Background
Obesity is a risk factor for female pelvic floor disorders. The study objective was to determine whether there was a difference in the subjective reporting of pelvic symptoms before and after bariatric surgery.
Methods
This was a prospective cohort study of female patients that underwent bariatric surgery. Patients completed a demographic questionnaire, the Pelvic Floor Distress Inventory-20 (PFDI-20), and the Pelvic Floor Impact Questionnaire-7 (PFIQ-7) before surgery and at 6 and 12 months following surgery. Body mass index (BMI) was compared between time points using Student’s t tests (P < 0.05 significant). Symptom and impact on quality of life prevalence were compared using McNemar’s test and questionnaire scores were compared using the Wilcoxon matched pairs test (P < 0.025 significant).
Results
At 12 months after surgery, 63 patients had completed the study. Even with significant weight loss (BMI, 43.7 kg/m2 to BMI, 29 kg/m2; P < 0.001), there was no significant difference in the prevalence of pelvic floor symptoms before and after surgery (94% to 81%, P = 0.2). Prevalence of pelvic floor symptom impact on quality of life did significantly decrease after surgery (56% to 30%; P = 0.004). Baseline PFDI-20 and PFIQ-7 scores were low; however, there was still a significant reduction in PFDI-20 and PFIQ-7 scores after surgery (P < 0.001).
Conclusions
Prevalence of pelvic floor symptoms did not vary greatly after surgery; however, significant weight reduction did improve the degree of bother and quality of life related to these symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is estimated that there are over 300 million obese adults worldwide, with the greatest rise seen in the proportion of obese females [1]. Currently, in the USA, >50% of women are classified as being overweight (body mass index (BMI) ≥25 kg/m2) or obese (BMI ≥30 kg/m2) [2, 3]. Obesity contributes to a number of chronic medical conditions, second only to tobacco-related disease in health care costs and preventable deaths, and is known to have a significant impact on overall quality of life [4, 5].
Obesity is a known risk factor for pelvic floor disorders including urinary incontinence, defecatory dysfunction, and pelvic organ prolapse (POP). The pathophysiology relating these disorders to obesity is multifactorial and specifically linked to issues of increased intra-abdominal pressure and other obesity-related conditions including abnormal nerve conduction, diabetes, and intervertebral disc herniation [6, 7]. Several studies have shown an association between obesity and urinary incontinence [8–11], with one study reporting a urinary incontinence prevalence of 67% in morbidly obese women presenting for consultation for weight loss surgery [8]. The association between obesity and fecal incontinence is less clear, although the same study demonstrated that 32% of women presenting for weight loss surgery reported symptoms of fecal incontinence [8]. Obesity and its relation to POP is also less defined; however, most of the data do suggest a positive correlation between obesity and POP [12, 13], with one study demonstrating a 2.5-fold increased risk of POP in overweight and obese women [14] and another study reporting obesity to be the strongest risk factor for POP recurrence after hysterectomy [15].
One treatment option for obese patients is bariatric surgery. This has been shown to be conclusively more effective at producing sustainable weight loss and controlling comorbidities than conservative approaches and medical treatment [16]. The effect of significant weight loss after bariatric surgery on pelvic floor disorders has been reported in a number of studies that have shown improvement in the prevalence of urinary [17–20] and bowel symptoms [19, 20].
The Pelvic Floor Distress Inventory-20 (PFDI-20) and the Pelvic Floor Impact Questionnaire-7 (PFIQ-7) are psychometrically valid and reliable questionnaires that are used together to measure the extent of female lower urinary tract, lower gastrointestinal tract, and POP symptoms and how they affect condition-specific quality of life [21]. These questionnaires are directed towards symptoms occurring in the last 3 months. The PFDI-20 has a total of 20 questions and is composed of three short-form subscales (Urinary Distress Inventory-6 (UDI-6), Colorectal–Anal Distress Inventory-8 (CRADI-8), and Pelvic Organ Prolapse Distress Inventory-6 (POPDI-6)). Each question in the PFDI-20 asks whether a symptom exists and, if the answer is “yes,” the patient is asked to quantify the degree of bother. Similarly, the PFIQ-7 has three short-form subscales each containing seven items (Incontinence Impact Questionnaire-7 (IIQ-7), Colorectal–Anal Impact Questionnaire-7 (CRAIQ-7), and Pelvic Organ Prolapse Impact Questionnaire-7 (POPIQ-7)). Each item in the PFIQ-7 asks the patient to quantify how pelvic floor symptoms affect quality of life, ranging from “not at all” to “quite a bit.”
The objective of the present study was to determine whether there was a difference in the subjective reporting of pelvic floor symptoms by women after a significant weight loss had occurred at 6 and 12 months after bariatric surgery. Symptoms were evaluated before and after surgery using the PFDI-20 and PFIQ-7.
Materials and Methods
This was a prospective cohort study investigating pelvic floor symptoms experienced by female patients that underwent bariatric surgery between June 2008 and February 2009. The Indiana University Health Institutional Review Board approved this study.
Patient Selection and Surgical Intervention
Patients were recruited from the Indiana University Bariatric and Medical Weight Loss Center. This center is dedicated to the comprehensive evaluation and follow-up of bariatric patients and their support through the weight loss surgery process. This facility consists of examination rooms, consultation rooms, and several classrooms for educational and supportive purposes and is staffed with specialized bariatric nurses, nutritionists, psychologists, and physicians. To be included in the study, patients had to be female, >18 years of age, and fulfill the National Institute of Health criteria for bariatric surgery (a BMI ≥ 40 kg/m2 or a BMI ≥ 35 kg/m2 with at least two comorbidities and has attempted to lose weight in the past) [22]. Patients interested in the procedure were either self-referred or physician-referred for consultation. Only patients that were consented for laparoscopic gastric bypass or laparoscopic sleeve gastrectomy were included in this study. The Female Pelvic Medicine and Reconstructive Surgery division of Indiana University was not actively treating any patients included in this study.
At this center, all patients present for a preoperative visit 2 weeks prior to surgery. A research coordinator was able to screen and identify patients that were eligible for the present study at that preoperative visit. The study protocol and consent form were described to the patient both verbally and in writing. Once the patient had read and voluntarily signed the consent form, the patient was then asked to complete a demographic questionnaire, as well as the PFDI-20 and PFIQ-7 questionnaires. The demographic questionnaire identified the following baseline characteristics: age, ethnicity, menopausal status, smoking status, number of pregnancies, number of vaginal deliveries, number of cesarean sections, history of prior hysterectomy, history of incontinence surgery, history of prolapse surgery, and presence of certain obesity-associated comorbidities (osteoarthritis, diabetes, obstructive sleep apnea, and hypertension). Height, weight, and BMI were also taken and recorded.
Two weeks after the preoperative visit, study patients underwent bariatric surgery. With the laparoscopic gastric bypass, a gastric “pouch” of 15–30 cc capacity is constructed with the use of special stapling devices that staple and cut simultaneously. The pouch includes the uppermost portion of the stomach (the cardia) and is based on the lesser curve of the stomach, thereby receiving its blood supply off the left gastric artery. The pouch is completely separated from the original (native) stomach. The small intestine is then measured 50 cm from its origin, divided, and reattached to a downstream segment of the small intestine at a distance of 100–150 cm. The free end of the intestine is then attached to the gastric pouch. The entire operation is performed laparoscopically.
The sleeve gastrectomy is also performed entirely by laparoscopic techniques. Dissection is initiated 5 cm proximal to the pylorus at the greater curvature of the stomach at which point the lesser sac is entered. Once the entire greater curvature has been mobilized, an F34 bougie is introduced by the anesthesiologist and is advanced along the lesser curve of the stomach. The stomach is then longitudinally resected along the bougie with the use of serial firings of linear staplers. The resected stomach is then extricated through one of the larger trocar sites.
Patient Follow-up
At the 6- and 12-month postoperative visits, patients returned to the clinic for study follow-up. At each visit, the patient’s weight and BMI were recorded, and they were asked to repeat both the PFDI-20 and PFIQ-7 questionnaires. Questionnaires were completed in the clinic unless the patient did not return for their follow-up appointment, at which point the patient was contacted by telephone and given the choice to complete the questionnaires either over the telephone or through the mail. When this occurred, patients were asked to weigh themselves and report the weight over the telephone or record it on the questionnaires being mailed in.
Statistical Analyses
For both the PFDI-20 and the PFIQ-7, each subscale is scored from 0 (least distress) to 100 (greatest distress) with the total score for both questionnaires ranging from 0 to 300. A change of 45 points (15%) or more in the total score of the PFDI-20 and a change of 36 points (12%) or more in the total score of the PFIQ-7 are considered to be clinically important [21]. The PFDI-20 score was used to calculate the necessary sample size for the present study. It was expected that the mean preoperative score would be approximately 200 (on a scale of 0–300). Assuming a mean decrease of 45 points at 6 months postsurgery would be considered significant, and assuming the standard deviation of the changes would be 100, 55 subjects would provide a 90% power to detect this difference using a two-sided paired test with a significance level α = 0.05. Allowing for a possible 20% dropout rate, a minimum of 70 subjects was found to be necessary to see such a difference.
Descriptive statistics were used to analyze the baseline demographic variables. Continuous variables were summarized using means and standard deviations, and categorical variables were summarized using counts and percentages.
BMI was also described as the means (±standard deviations) and were compared between baseline and 6 and 12 months using Student’s t tests (P < 0.05 considered statistically significant).
At the baseline, 6-month, and 12-month visits, the prevalence of symptoms (as indicated by a “yes” versus “no” answer to any question in the entire PFDI-20 and within each of the individual subscales) and the prevalence of impact on quality of life (as indicated by recording “not at all,” meaning impact on quality of life was not present, versus “somewhat,” “moderately,” or “quite a bit,” meaning impact on quality of life was present, in the entire PFIQ-7 and within each of the individual subscales) were recorded from the questionnaires. Prevalence rates were compared between baseline and 6 months, as well as between 6 and 12 months using McNemar’s test for nonparametric data. Since two tests were performed in this comparison, the significance level was adjusted using a Bonferroni correction, whereby P values of <0.025 were considered significant. Questionnaire scores were used to assess the degree of bother of symptoms (PFDI-20) and the degree of bother of the symptoms impact on quality of life (PFIQ-7). Scores were described using medians with minimum and maximum ranges and were compared between baseline and 6 months and between 6 and 12 months using the Wilcoxon matched pairs test for nonparametric data. Once again, since two tests were performed in this comparison, a Bonferroni correction was used and P values <0.025 were considered significant. A Spearman’s rank correlation coefficient was calculated between BMI and PFDI-20 scores at each time point to determine the strength of association between the two variables (P < 0.05 considered statistically significant).
Results
Initially, 83 patients were consented for the procedure, 19 of which did not go through with the surgery as planned, leaving 64 patients eligible for follow-up. Of these 64 patients, 58 patients underwent laparoscopic gastric bypass surgery (55 primary surgeries, 1 previous Nissen fundoplication, and 2 previous vertical banded gastroplasty) and 6 had laparoscopic sleeve gastrectomy (all primary surgeries). At 6 months follow-up, complete data were collected from 61 patients, and at 12 months, complete data were collected from 63 patients.
Baseline demographic information is reported in Table 1. Within this cohort, the mean age was 48 years (range, 23 to 69 years) with almost half of the patients being postmenopausal (47%). Most patients were Caucasian (83%), nonsmokers (97%), and had one or more vaginal deliveries (66%). A history of prior hysterectomy was common (36%), although prior incontinence (5%) and prolapse surgery (3%) were rare.
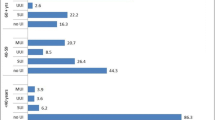
Weight, BMI, and questionnaire scores at baseline, 6 months, and 12 months, as well as the statistical comparisons between the time points are reported in Table 2. Patients showed a significant reduction in weight and BMI at both 6 and 12 months after bariatric surgery.
The prevalence of symptoms, as indicated by any “yes” answer on the PFDI-20, was high (>80%) without any significant difference seen before or after surgery (P > 0.025). When looking at the prevalence of symptoms within each of the PFDI-20 subscales, bladder and bowel symptoms appeared to be more prevalent than POP symptoms. The prevalence of impact on quality of life, as indicated by answering any degree on the PFIQ-7, was significantly lower at 6 months after surgery (56% versus 34%, P = 0.004) and this lower prevalence rate continued at 12 months after surgery (30%). Once again, when looking at each of the three subscales of the PFIQ, the prevalence of impact on quality of life was higher for bowel and bladder symptoms than POP symptoms.
Baseline PFDI-20 and, in particular, PFIQ-7 scores were relatively low (median scores <100). Despite the small baseline scores, there were significant reductions in PFDI-20 and PFIQ-7 scores at 6 months after surgery (P values <0.001). These reduced scores were maintained at 12 months after surgery, as shown by no significant change in values between 6 and 12 months (P values >0.025).
Spearman correlation coefficients between BMI and PFDI-20 scores were the following: 0.2 at baseline (P = 0.07), 0.15 at 6 months (P = 0.3), and 0.2 at 12 months (P = 0.07).
Discussion
The present study evaluated the effect of significant weight loss after bariatric surgery on pelvic floor symptoms reported by women using two condition-specific validated questionnaires, the PFDI-20 and PFIQ-7. This study also attempted to determine whether a correlation existed between BMI and PFDI-20 score before and after surgery.
Prior to surgery, the baseline prevalence of pelvic floor symptoms was high (94%), although the degree of bother from these symptoms was relatively low, as indicated by the median PFDI-20 score of 62. Within the PFDI-20, the UDI-6 and CRADI-8 subscales appeared to have higher prevalence rates than the POPDI-6 subscale; however, the UDI-6 had a higher median score than the CRADI-8 and POPDI-6, indicating that urinary symptoms were more bothersome in this group of obese women. The baseline prevalence of impact on quality of life was lower (56%) and the overall degree of bother from this impact was very low, as indicated by the median PFIQ-7 score of 5. Prior to surgery and weight loss, the IIQ-7 had a higher prevalence rate than the CRAIQ-7 and POPIQ-7. The IIQ-7 was the only subscale with a recordable median score, indicating that only urinary symptoms caused any reportable bother from their impact on quality of life and bowel and POP symptoms were not significant issues for this group of obese women. These findings at baseline are similar to those reported elsewhere in the literature. Chen et al. reported a pelvic floor disorder prevalence rate of 75% in obese patients enquiring about bariatric surgery with significantly higher rates of urinary and anal incontinence symptoms but comparable rates of prolapse symptoms when compared to controls [23]. Whitcomb el al. reported only a 46% prevalence rate of pelvic floor symptoms in 1,155 obese women [24]. Wasserberg et al. studied 400 morbidly obese patients enrolled in a bariatric program and assessed pelvic floor disorder symptoms using the PFDI-20 and PFIQ-7 prior to surgery [25]. The results were very similar to the baseline rates of the present study. They reported a high pelvic floor disorder prevalence rate of 91% and a lower PFDI-20 mean score of 67.5. They also demonstrated a lower impact on quality of life prevalence rate of 53%, as well as a low PFIQ-7 mean score of 32.6.
The present study determined that a significant weight loss seen at 6 and 12 months after bariatric surgery did not significantly change the prevalence of overall pelvic floor disorders (94% to 81%, P = 0.2). Although not statistically significant, there was a notable decrease in the prevalence of urinary (86% to 59%) and POP symptoms (72% to 38%), with persistence in bowel symptoms (80% to 75%). Despite the lack of change in overall prevalence, the degree of bother from these symptoms did significantly improve after surgery, as indicated by the overall PFDI-20 score (62 to 22, P < 0.001). Specifically, degree of bother from urinary symptoms showed the largest improvement at both 6 and 12 months postsurgery. These results are consistent with other reports in the literature [19, 20]. Wasserberg et al. did a follow-up study with results very similar to the present study [20]. This group compared pelvic floor symptoms before and after bariatric surgery in only those patients that achieved >50% excess body weight loss. The reported prevalence of pelvic floor disorders as assessed by the PFDI-20 was 87% prior to surgery and 65% after surgery (P = 0.02). This reduction was primarily due to the decrease in urinary symptoms from 71% to 39% (P = 0.003). The degree of bother identified by the PFDI-20 scores also significantly decreased from 45 before and 35 after surgery, primarily due to the differences in UDI-6 scores (P = 0.015).
In the present study, the improved degree of bother seen in the PFDI-20 score was likely due to the reduced prevalence of urinary and prolapse symptoms. The overall prevalence was not significantly changed as the bowel symptoms persisted postoperatively. Persistent and de novo bowel symptoms are a common complaint resulting from the bariatric procedure itself. Up to 15% of bariatric patients can develop long-term issues of dumping syndrome with symptoms of nausea, vomiting, pain, and diarrhea [26]. This side effect may have impacted the reported bowel symptoms captured in the PFDI-20. When comparing bowel symptoms before and after bariatric surgery, Burgio et al. reported a significant reduction in loss of liquid and solid stool from 19.2% before surgery to 8.6% after surgery [19]. However, there was a significant increase in the prevalence of incontinence to flatus after surgery (12.9% to 30.1%) and an increase in overall fecal incontinence symptoms when solid stools, liquid stools, and flatus were combined. Wasserberg et al. also showed no significant improvement in colorectal distress/impact scores or prevalence after weight loss when using the PFDI-20 questionnaire before and after bariatric surgery [20]. Alternatively, multiple studies have shown that surgically induced weight loss does improve urinary symptoms [8–11]. Bump et al. evaluated obese women with urinary incontinence and found a significant improvement in urinary incontinence after surgically induced weight loss [17]. They showed that a reduction in bladder pressure and waist circumference were independent predictors of postoperative improvement in urinary incontinence. Reduction in symptoms of POP has also been previously demonstrated after weight reduction surgery and may be related to a decrease in abdominal pressure that can lead to muscle and/or fascial weakness or pudendal nerve stretch injury that can contribute to symptoms of pelvic pressure and descent [20].
With regard to impact on quality of life, this study showed a significant improvement in both prevalence (56% to 30%, P = 0.004) and degree of bother (score 5 to 0, P < 0.001) at 6 and 12 months after surgery. Once again, the change in bladder symptoms was the contributing factor to this significant change seen after surgery. Wasserberg et al. also showed that the effect on quality of life significantly improved, as shown by the PFIQ-7 before (score = 17) and after surgery (score = 3, P = 0.002) [20]. These scores were significantly better as a result of the differences in both the IIQ-7 and POPIQ-7 scores.
The PFIQ-7 looks at whether or not bladder, bowel, and prolapse symptoms affect ones’ ability to perform various activities of daily living (i.e., household chores, physical activity, entertainment activities, social activities, ability to travel, and emotional health). While the questionnaire specifically asks the patient to relate their pelvic floor symptoms to these activities, the surgically induced weight loss may have made these activities more achievable despite the presence or absence of various pelvic floor symptoms. This may have been a contributing factor to the improved PFIQ-7 scores seen after surgery.
Interestingly, the present study failed to identify a correlation between BMI and PFDI-20 score before or after surgery, indicating that PFDI-20 scores were not necessarily dependent on or influenced by patient BMI. This is similar to other reports in the pelvic floor/bariatric literature [20, 25].
Strengths of the present study include a significant sample size, good patient follow-up and compliance, and the use of reliable and validated condition-specific quality of life questionnaires. Although this cohort of patients was notably heterogeneous in age and parity, this sample of patients likely represents a typical bariatric population. Therefore, this heterogeneity is likely a strength of the study as it makes the results generalizable and applicable to other patients seeking bariatric care.
There were also several limitations to the present study. Although most of the questionnaires were self-administered, a small percentage was completed over the telephone with study personnel. This difference in administration may have affected the true outcome of the follow-up questionnaires. In addition, this study incorporated no objective measures of pelvic floor disorder. Future studies investigating pelvic floor issues in bariatric patients before and after surgery should include subjective symptom assessment with validated questionnaires, as well as objective measures such as bladder and bowel diaries, POP quantification measurements, urodynamic studies, and pelvic floor strength.
Conclusion
The present study showed that significant weight loss seen at 6 and 12 months after bariatric surgery does not have a significant effect on pelvic floor symptom prevalence; however, the degree of bother from these symptoms and their impact on quality of life was significantly improved, as demonstrated by the PFDI-20 and PFIQ-7 scores, respectively. The majority of this improvement was seen in the urinary subscales of these questionnaires. This study also demonstrated that patient BMI did not influence PFDI-20 scores.
References
World Health Organization Office of Health Communications and Public Relations. Obesity and overweight. Geneva: World Health Organization; 2006.
Mokdad AH, Serdula MK, Dietz WH, et al. The spread of the obesity epidemic in the United States, 1991–1998. JAMA. 1999;282:1519–22.
Must A, Spadano J, Coakley EH, et al. The disease burden associated with overweight and obesity. JAMA. 1999;282:1523–9.
Allison DB, Fontaine KR, Manson JE, et al. Annual deaths attributable to obesity in the United States. JAMA. 1999;282:1530–8.
Pender JR, Pories WJ. Epidemiology of obesity in the United States. Gastroenterol Clin North Am. 2005;34:1–7.
Noblett KL, Jensen JK, Ostergard DR. The relationship of body mass index to intra-abdominal pressure as measured by multichannel cystometry. Int Urogynecol J Pelvic Floor Dysfunct. 1997;8:323–6.
Cummings JM, Rodning CB. Urinary stress incontinence among obese women: review of pathophysiology therapy. Int Urogynecol J Pelvic Floor Dysfunct. 2000;11:41–4.
Richter HE, Burgio KL, Clements RH, et al. Urinary and anal incontinence in morbidly obese women considering weight loss surgery. Obstet Gynecol. 2005;106:1272–7.
Richter HE, Burgio KL, Brubaker L, et al. Factors associated with incontinence frequency in a surgical cohort of stress incontinent women. Am J Obstet Gynecol. 2005;193:2088–93.
Hannestad YS, Rortveit G, Daltveit AK, et al. Are smoking and other lifestyle factors associated with female urinary incontinence? The Norwegian EPINCONT Study. BJOG. 2003;110:247–54.
Dwyer PL, Lee ET, Hay DM. Obesity and urinary incontinence in women. Br J Obstet Gynaecol. 1988;95:91–6.
Uustal Fornell E, Wingren G, Kjolhede P. Factors associated with pelvic floor dysfunction with emphasis on urinary and fecal incontinence and genital prolapse: an epidemiological study. Acta Obstet Gynecol Scand. 2004;83:383–9.
Jelovsek JE, Maher C, Barber MD. Pelvic organ prolapse. Lancet. 2007;369:1027–38.
Hendrix SL, Clark A, Nygaard I, et al. Pelvic organ prolapse in the Women’s Health Initiative: gravity and gravidity. Am J Obstet Gynecol. 2002;186:1160–6.
Marchionni M, Bracco GL, Checcucci V, et al. True incidence of vaginal vault prolapse. Thirteen years of experience. J Reprod Med. 1999;44:679–84.
Sjostrom L, Narbro K, Sjostrom CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741–52.
Bump RC, Sugerman HJ, Fantl JA, et al. Obesity and lower urinary tract function in women: effect of surgically induced weight loss. Am J Obstet Gynecol. 1992;167:392–7. discussion 397–99.
Sugerman H, Windsor A, Bessos M, et al. Effects of surgically induced weight loss on urinary bladder pressure, sagittal abdominal diameter and obesity co-morbidity. Int J Obes Relat Metab Disord. 1998;22:230–5.
Burgio KL, Richter HE, Clements RH, et al. Changes in urinary and fecal incontinence symptoms with weight loss surgery in morbidly obese women. Obstet Gynecol. 2007;110:1034–40.
Wasserberg N, Petrone P, Haney M, et al. Effect of surgically induced weight loss on pelvic floor disorders in morbidly obese women. Ann Surg. 2009;249:72–6.
Barber MD, Walters MD, Bump RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol. 2005;193:103–13.
NIH conference. Gastrointestinal surgery for severe obesity. Consensus Development Conference Panel. Ann Intern Med. 1991;115:956–61.
Chen CC, Gatmaitan P, Koepp S, et al. Obesity is associated with increased prevalence and severity of pelvic floor disorders in women considering bariatric surgery. Surg Obes Relat Dis. 2009;5:411–5.
Whitcomb EL, Lukacz ES, Lawrence JM, et al. Prevalence and degree of bother from pelvic floor disorders in obese women. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:289–94.
Wasserberg N, Haney M, Petrone P, et al. Morbid obesity adversely impacts pelvic floor function in females seeking attention for weight loss surgery. Dis Colon Rectum. 2007;50:2096–103.
Abell TL, Minocha A. Gastrointestinal complications of bariatric surgery: diagnosis and therapy. Am J Med Sci. 2006;331:214–8.
Conflict of Interest Statement
Colleen D. McDermott, Colin L. Terry, and Samer G. Mattar have no conflicts of interest to declare. Douglass S. Hale is a consultant for Women’s Health and Urology/Ethicon (Somerville, NJ, USA) and is a clinical investigator for Allergan (Irvine, CA, USA).
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was completed in Indianapolis, IN, USA.
Rights and permissions
About this article
Cite this article
McDermott, C.D., Terry, C.L., Mattar, S.G. et al. Female Pelvic Floor Symptoms Before and After Bariatric Surgery. OBES SURG 22, 1244–1250 (2012). https://doi.org/10.1007/s11695-012-0592-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-012-0592-5