Abstract
Background
Bariatric surgery has emerged as an effective and safe treatment for severe obesity and utilization rates have increased dramatically. In private health care settings, low socioeconomic status is associated with a reduced likelihood of undergoing a bariatric procedure. Whether this relationship is also present in a universally accessible, publicly funded health care system is not currently known.
Methods
A retrospective analysis of the Edmonton Weight Wise obesity program clinical registry was conducted. Patients who were unemployed, on long-term disability or receiving social assistance were classified as “low income” status. The remaining patients were categorized as “regular income” status. Multivariable logistic regression analysis was used to examine the association between low income status and approval for surgery within 1 year of program entry.
Results
Thirty-three (7%) of 419 patients were ineligible for surgery or excluded because of missing income status data. Of the remaining 386 patients, 72 (19%) were of low income status and 89 (23%) were approved for surgery. Low income patients were older, heavier, and had greater comorbidity. Compared to patients of regular income status, those with low income status were less likely to be approved for surgery (15.3% versus 24.8%; adjusted OR 0.45; 95% CI 0.22 to 0.94).
Conclusions
Within a publicly funded and universally accessible regional obesity program, lower income status patients were less likely to be approved for bariatric surgery. Further study is necessary to clarify this apparent disparity and to determine if program modifications are necessary to ensure equity across all socioeconomic strata.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Severe obesity (body mass index ≥ 40 kg/m2) affects 3% of Canadians [1] and 5% of Americans [2] and is the fastest growing obesity demographic, having risen in prevalence by 400% over the last two decades [1, 3]. It is associated with substantial increases in morbidity, premature mortality, reduced quality of life and increased health care costs [4]. Bariatric surgery has emerged as the preferred treatment option for suitable candidates with severe obesity who are refractory to nonsurgical therapy. Observational studies have demonstrated that surgery reduces weight by 33% in the early postoperative years [5] and 14–25% after 10 years [6]. Surgery is associated with remission rates of 66–88% in medical comorbidities (diabetes, hypertension, dyslipidemia, sleep apnea) [20] and significant reductions in 15-year mortality (5.0% versus 6.3%; HR 0.76; 95% CI 0.59 to 0.99) have been observed in comparison to nonsurgical matched controls [6]. Quality of life, self-esteem, and employment status are also improved [7] and surgical costs appear to be recouped within 2–4 years of operating [8].
Utilization of bariatric procedures has increased throughout the world in concordance with the expanding evidence base for surgery; in both Canada and the USA, a 10-fold rise has been reported in recent years [9, 10]. However, in the largely privatized health care system of the USA, notable differences in the utilization of bariatric surgery across sociodemographic strata have been documented. In particular, ethnic minorities and patients of lower socioeconomic status appear less likely to receive surgery despite harboring greater risk for obesity and associated comorbidities [11]. This has been attributed to a number of potential factors including differences across socioeconomic strata in insurance coverage and ability to pay for surgery, a lack of a validated triage system to prioritize access according to clinical need, and differences in patient/provider preferences and attitudes toward surgery [12].
Canada’s publicly funded health care system is intended to provide equitable and timely access for all citizens. However, access to bariatric surgery within Canada is extremely limited, with an estimated average wait time of 5 years [13] and an estimated demand that exceeds potential capacity by over 600-fold [14]. To our knowledge, the association between socioeconomic status and the probability of receiving surgery within Canada or a similar publicly funded, universally accessible health care system has not been previously reported. We retrospectively analyzed data from the Edmonton Weight Wise Clinic obesity management program in Edmonton, Canada to examine the relationship between income status and approval for bariatric surgery.
Methods
Setting and Subjects: Weight Wise Program
In 2005–2006, Capital Health was an academic-based health region that provided service to the approximately 1 million residents of greater Edmonton and an additional 600,000 residents in surrounding regions [15]. By extrapolating from contemporary Canadian obesity surveillance data (i.e., 7.8% of Canadians are moderately [BMI 35.0–39.9 kg/m2] or severely obese), we estimate that approximately 125,000 patients in the population serviced by Capital Health in 2005 had a BMI ≥ 35 kg/m2 [1].
In 2005–2006, a regional obesity program—“Weight Wise”—was developed and implemented within Capital Health. Weight Wise included a central access point, community education classes, and adult and pediatric services. The first major operational piece, the adult specialty clinic, began in December 2005 and provided medical and surgical bariatric specialty care to practitioner-referred patients with BMI of ≥35 kg/m2. All patients received guideline-concordant behavioral counseling and medical treatment delivered by a multidisciplinary team of physicians, nurses, dietitians physiotherapists, and social workers. The planned length of follow-up was typically 1 year from baseline assessment.
Eligibility for Surgery
Patients with BMI ≥ 35–39.9 kg/m2 and a major medical comorbidity or BMI ≥ 40 kg/m2 were considered potential candidates for surgery. The decision to proceed with surgery was typically made within the first 6–9 months of presentation to the clinic. Although the bariatric surgeon made the final decision regarding approval for surgery, a team-based process was used to discuss surgical candidacy. Contraindications to surgery in 2005–2006 included pregnancy, uncontrolled psychiatric disease, active substance abuse or smoking (patients were required to quit prior to surgery), an active eating disorder (anorexia or bulimia), age over 60 years, and high-risk medical status (e.g., severe coronary artery disease). Importantly, patients with a perceived lack of commitment or compliance with recommendations for lifestyle modification were generally not considered surgical candidates. This approach is based on the presumption that long-term outcomes are dependent upon some degree of lifestyle modification. Compliance was based on weight stabilization, adherence to clinic follow-up appointments, and commitment to self-monitoring (journals, pedometers).
Data Collection
We retrospectively analyzed a prospectively collected clinical database encompassing the first 419 Albertans assessed in the Weight Wise Adult Specialty Clinic in 2005–2006. The vast majority of patients seen in 2005–2006 were drawn from an existing wait list of over 600 patients who had been referred to bariatric surgeons within the region in 2005 or prior for consideration of bariatric surgery. Therefore, even though the level of interest in surgery was not explicitly documented for each patient, it is highly likely that nearly all patients seen within the first year were interested in bariatric surgery. Data included age, sex, BMI level, income status, approval for surgery within 1 year of presentation, the date of approval for surgery (if applicable), and the presence or absence of obesity-related comorbidities. The University of Alberta Research Ethics Board approved the study.
Definition of Income Status and Exclusions
A priori, income status was dichotomized into a binary variable, based upon our observations that the most socioeconomically disadvantaged patients in the clinic were those who were unemployed, receiving long-term disability or dependent upon social assistance (including Assured Income for the Severely Handicapped) via the Government of Alberta. These three groups were categorized as “low” income status. All other patients, including full-time workers, part-time workers, retirees, students, and homemakers were considered to be of “average” or “high” income status and are labeled hereafter as “regular income status” for the sake of brevity. Although students and homemakers typically generate little income per se, income supplementation is usually available from ancillary sources (student loans, other family members, etc.). If these individuals were receiving social assistance, they were classified in the low income category. Patients with unknown income status were excluded from further analyses. Also excluded were patients who did not meet standard NIH and local criteria for surgery, including those over 60 years of age or with BMI levels less than 35 kg/m2 [16]. All patients with BMI levels of 35 kg/m2 that were included in the study had at least one obesity-related comorbidity, and therefore, met current eligibility requirements for surgery.
Statistical Analyses
Multivariable logistic regression analysis was performed using SAS®, version 9.1 (SAS Institute, Cary, NC, USA) to examine the association between baseline income status and approval for bariatric surgery within 1 year of the baseline visit. Potential covariates included age (modeled using increments of 5 kg/m2, which exhibited a greater linear relationship to income status compared to increments of 1 kg/m2), gender, BMI, smoking status, and the following baseline obesity-related comorbidities (coded as binary variables): type 2 diabetes mellitus, gastroesophageal reflux disease, thyroid disease, obstructive sleep apnea, hypertension, mental illness (depression, anxiety, or psychoses), osteoarthritis, cerebrovascular disease, congestive heart failure, and malignancy. Age, gender, BMI, income status, and any covariate achieving a p value of <0.30 on univariable analysis were included in the final model.
Additional analyses were performed to ascertain whether follow-up times differed according to baseline income status. We hypothesized that a lower probability for surgical approval in lower income patients might be present in conjunction with a higher premature program dropout rate. In other words, if low income patients were more likely to leave the program early, they may be less likely to have a chance to be approved for surgery. We compared the proportion of patients failing to keep at least one follow-up appointment between low and regular income groups. In addition, using survival analysis stratified by income status, we examined time-to-program discontinuation in those patients that returned for at least one follow-up appointment. Mean time-to-program discontinuation was compared between low and regular income groups both graphically and numerically using a logrank test, with a p value of 0.05 considered statistically significant.
Results
Baseline Characteristics
Of the 419 patients eligible for study, 33 were excluded from analysis: 12 patients had unknown income status, 16 patients were over 60 years of age, and five patients had a BMI less than 35 kg/m2. Of the remaining 386 patients, 72 and 314 were of low and regular income status, respectively (Table 1). The 72 low income patients included 39 receiving social assistance, 26 unemployed, and seven receiving disability benefits. Low income patients were older, heavier, and had higher levels of comorbidity, including mental illness, diabetes, hypertension, and arthritis compared to regular income patients. Smoking rates were similar between the two groups.
Low Income Status as a Predictor of Approval for Surgery
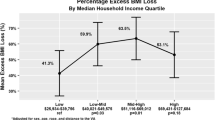
Of the 386 patients, 89 were approved for surgery, including 11 (15.3%) low income patients and 78 (24.8%) regular income patients. On univariable analysis, compared to regular income status, low income status was associated with a reduced chance for surgical approval (OR 0.55; 95% CI 0.27 to 1.1), which was not statistically significant (p = 0.09).
Covariates included in the final multivariable logistic regression model were age, BMI, gender, diabetes, history of cardiac disease, dyslipidemia, gastroesophageal disease, and thyroid disease. Mental illness was not a significant predictor of approval for surgery on univariable analysis (p = 0.91) and was not included in the final model. Low income status was associated with a significantly lower covariate-adjusted odds of surgical approval (OR 0.45; 95% CI 0.22 to 0.94). Female gender, higher age, and higher BMI level were also significant predictors of surgery approval (Table 2).
Follow-Up Rates of Regular and Low Income Groups
Of the original 386 patients eligible for surgery, 176 had discontinued follow-up by 3 months and 225 by 6 months. The number of patients who failed to show for at least one follow-up appointment (n = 65) was similar between groups [14/72 (19%) for low income patients and 51/314 (16%) for regular income patients].
In the remaining 321 patients with at least one follow-up visit, mean follow-up rates were similar both numerically and graphically (data not shown) between low income and regular income groups (9.2 months versus 9.7 months, respectively; p = 0.40)
Discussion
In the first year of a publicly funded regional obesity program, low income status was associated with significantly lower covariate-adjusted odds of approval for bariatric surgery. Premature program termination was not significantly different between patients of low and regular income status and is not an explanation for the observed findings. Our findings are similar to data from the USA demonstrating a reduced rate of utilization of bariatric surgery in the socioeconomically disadvantaged [12].
It is possible that unmeasured or unaccounted factors may explain our findings. Obese patients of lower socioeconomic status may experience a greater number of barriers to successful weight management, including a lack of money to purchase healthy foods, difficulties with travel to clinic visits, limited access to safe exercise facilities, and a greater social acceptance of excess body weight [16–19]. It is also possible that additional barriers, such as a lack of motivation or readiness-to-change [21], may be more prevalent in those of lower socioeconomic status and this may lead to patient or provider reluctance to consider surgery as an appropriate option. Low income patients may be less likely to demonstrate adherence and commitment to the preoperative program, a major precondition for surgical approval in the Weight Wise program.
Approximately 90% of patients undergoing bariatric surgery in Canada are free of cardiovascular comorbidity, which indicates a preference by surgeons to operate on relatively uncomplicated patients [9]. Because obesity-related comorbidity was higher in Weight Wise patients of lower income status, one might expect that this higher burden of illness could account for the reduced chance of surgical approval. However, the inverse association between low income status and approval for surgery was actually stronger after adjustment for comorbidities, suggesting that the presence of a higher burden of illness did not negatively affect approval for surgery. Although mental illness was more common in patients of lower income status, it was not predictive of approval for surgery. This is not surprising because the management and stabilization of mental illness is required prior to proceeding with surgery.
Only 23% (89/386) of eligible patients were approved for surgery, which appears low at first glance. However, this must be interpreted in the context of the large number of premature program terminations. Because only 161 of 386 patients (40%) remained in the program at the 6-month mark, a large number of patients did not access surgery because of program withdrawal. Although we did not formally document additional reasons for not accessing surgery, we suspect that many of the remaining patients either had a contraindication to surgery (including being unable or unwilling to quit smoking) or were more appropriately managed with nonsurgical treatments.
There are several limitations of this study including: the retrospective nature of the data collection and the lack of a direct method for the assessment of income and socioeconomic status. However, given our accumulated and collective experience with the clinic population in the Weight Wise program from 2005 to present, we are confident that the three categories used to represent low income status (unemployed, disability, and social assistance) accurately reflect the lowest socioeconomic bracket of our patient population. Even though income status data were missing for 12 patients, repeating the analysis while assuming all of these patients were first of low income status and then of regular income status did not change the results. Although information on ethnicity was not formally collected, any theoretical ethnic-specific differences in attitudes toward bariatric surgery are unlikely to have had a major impact on our findings because the vast majority of our clinic population is Caucasian. An additional limitation is that, while we feel that these data can be broadly generalized to similar programs and health care settings, only a single regional program in Canada was studied and these findings may not be completely representative of other sites within Canada or countries with similar health care systems.
In conclusion, low income patients within a publicly funded, regional obesity program were less likely to be approved for bariatric surgery. The factors underlying the lower rates of utilization in patients of lower socioeconomic status require further delineation. As these factors are identified, obesity management programs can be modified to best manage low income status patients and equalize access to the surgical management of obesity. Programs must ensure equitable access to obesity management across socioeconomic strata even in the face of current limitations of these important resources.
References
Tjepkema M. Measured obesity. Adult obesity in Canada: measured height and weight. 2008. In: Nutrition: findings from the Canadian Community Health Survey 2004; issue I (cat no 82-620-MWE2005001). Accessed March 13, 2010 at www.statcan.ca/english/research/82-620-MIE/2005001/articles/adults/aobesity.htm.
Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–55.
Sturm R. Increases in clinically severe obesity in the United States, 1986–2000. Arch Intern Med. 2003;163:2146–8.
Hensrud DD, Klein S. Extreme obesity: a new medical crisis in the United States. Mayo Clin Proc. 2006;81 Suppl 10:S5–10.
Sjostrom L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351:2683–93.
Sjostrom L, Narbro K, Sjostrom CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741–52.
Livingston EH, Fink AS. Quality of life: cost and future of bariatric surgery. Archives of surgery (Chicago, Ill: 1960). 2003;138:383–8.
Cremieux PY, Buchwald H, Shikora SA, et al. A study on the economic impact of bariatric surgery. Am J Manag Care. 2008;14:589–96.
Padwal RS. Characteristics of patients undergoing bariatric surgery in Canada. Obes Res. 2005;13:2052–4.
Santry HP, Gillen DL, Lauderdale DS. Trends in bariatric surgical procedures. JAMA. 2005;294:1909–17.
Livingston EH, Ko CY. Socioeconomic characteristics of the population eligible for obesity surgery. Surgery. 2004;135:288–96.
Flum DR, Khan TV, Dellinger EP. Toward the rational and equitable use of bariatric surgery. JAMA. 2007;298:1442–4.
Christou NV, Efthimiou E. Bariatric surgery waiting times in Canada. Can J Surg. 2009;52:229–34.
Padwal R, Sharma AM. Treating severe obesity: morbid weights and morbid waits. CMAJ. 2009;181:777–8.
Capital Health. About Us (online). 2008. Accessed on March 13, 2010 at www.capitalhealth.ca/AboutUs/default.htm.
National Heart, Lung, and Blood Institute, National Institutes of Health. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. NIH Publication No. 98-4083. Bethesda, MD: National Institutes of Health; 1998.
Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79:6–16.
Miles R, Panton L. The influence of the perceived quality of community environments on low income women's efforts to walk more. J Community Health. 2006;31:379–92.
Sobal J, Stunkard AJ. Socioeconomic status and obesity: a review of the literature. Psychol Bull. 1989;105:260–75.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37.
Mauro M, Taylor V, Wharton S, et al. Barriers to obesity treatment. Eur J Intern Med. 2008;19:173–80.
Acknowledgments
This study was unfunded.
Competing interests
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study is to be presented in poster form at the University of Alberta, Resident Research Day, on May 20, 2010.
Contributors
R. Padwal developed the study concept. K. Halloran and R. Padwal performed data analysis/interpretation and cowrote the initial draft. All other authors performed data interpretation and critically revised the manuscript for important intellectual content. All authors approved the final version of the manuscript.
Rights and permissions
About this article
Cite this article
Halloran, K., Padwal, R.S., Johnson-Stoklossa, C. et al. Income Status and Approval for Bariatric Surgery in a Publicly Funded Regional Obesity Program. OBES SURG 21, 373–378 (2011). https://doi.org/10.1007/s11695-010-0149-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-010-0149-4