Abstract
Background
Our study describes the prevalence of nonalcoholic steatohepatitis (NASH) and liver fibrosis in Hispano-American morbidly obese patients and the utility of different serum markers to predict significant liver fibrosis in this population.
Methods
We perform a retrospective chart review of all patients undergoing Roux-en-Y gastric bypass with routine liver biopsy performed at Valley Baptist medical center during a 24-month period (2005–2006).
Results
Of 129 liver biopsies, only 25.7% had some degree of steatosis, but about 55% had NASH, and 30.9% had liver fibrosis. Of those patients with liver fibrosis, only 6.9% had moderate to severe fibrosis (stages 2–4), and only one patient had cirrhosis (0.7%). Of the 129 patients, only 92 had a FIBROspect score II in their chart, and they ranged from 9 to 95, with a mean of 28.3. Of these patients, 36 had a score less than 20, and none had significant fibrosis in their biopsy. FIBROspect II® score (cutoff <20) had a negative predictive value (NPV) of 100% (confidence interval (CI) 95%, 0.9035–1) positive predictive value (PPV) of 15% (CI 95%, 0.0838–0.2693), sensitivity of 100%, and specificity of 42% to predict stage 2 fibrosis or higher.
Conclusions
NASH and liver fibrosis are present in a high percentage of morbidly obese patients. Liver function tests and ultrasound are not reliable tests to diagnose or rule out advance liver fibrosis. The use of FIBROspect II® score in the preoperative evaluation of morbidly obese patients can rule out significant liver fibrosis (stages 2–4) and avoid the morbidities related to liver biopsy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity as one of the most common health problems in the USA is associated with multiple comorbidities like insulin resistance, metabolic syndrome, hypertension, sleep obstructive apnea, and also liver disease [1–5]. In the past decades in Europe and North America, there has been a rapid increase in the prevalence of morbid obesity as well as their associated conditions, especially nonalcoholic fatty liver disease (NAFLD). In North America, around 32% of the adult population is obese, and as much as 80% of adults with morbid obesity could have fatty liver disease [2, 6].
NAFLD involves a wide spectrum of histological lesions ranging from simple hepatic steatosis to nonalcoholic steatohepatitis (NASH) with or without liver fibrosis. During the past 20 years, NAFLD has become the most common chronic liver disease in Europe and North America. Patients with NAFLD and advanced stages of liver fibrosis are at high risk of progressing to end-stage liver disease or cirrhosis [7–9].
NASH is a very common pathology in morbid obese patients that undergo bariatric surgery [9]. The exact prevalence of NASH with and without liver fibrosis in the different populations like Caucasians, African American, Hispanics, and Asians has been a matter of research and remains to be clearly defined for each of them [6–9]. It is of great importance for bariatric surgeons to have clear knowledge of the disease prevalence, behavior, and the available diagnostic tests for liver fibrosis and NASH [10].
Multiple noninvasive techniques have been used to diagnose fatty liver disease. Ultrasound has a moderate to high sensitivity but low specificity and is unable to evaluate the stage of the disease and to differentiate between liver fibrosis and steatohepatitis [11]. There have been several studies that try to predict the risk for having severe fibrosis using liver function tests, ultrasound, and risk factors like diabetes and hyperlipidemia, but most of these techniques are complicated algorithms or require multiple testing and are still not highly sensitive or specific [12, 13]. Currently, none of the noninvasive tests can rule out significant liver fibrosis with a 100% predictive value, and most surgeons rely on liver biopsy to accurately diagnose or rule out NAFLD [13–16].
Liver biopsy has been the gold standard to diagnose liver fibrosis and NAFLD in patients with morbid obesity. Some surgeons perform liver biopsy routinely, and this adds morbidity to any bariatric surgical procedure [15]. There are several biochemical markers used currently to evaluate and to rule out significant liver disease in patients with chronic hepatitis and also in obese patients. The use of serum markers will avoid liver biopsy. Presently, several novel markers have been studied; one of the best known to predict liver fibrosis in patient with chronic hepatitis has been FIBROspect II score; this is the result of three different serum markers (serum hyaluronic acid, alpha 2 macroglobulin, and tissue inhibitor metalloprotease 1) all related to extracellular matrix remodeling that will likely be elevated in patients with significant amount of liver fibrosis. Its utility as a predictor of liver disease in morbid obese patient has not been studied in detail [14, 16].
The aim of our study is to describe the prevalence of NASH and liver fibrosis in morbidly obese Hispano-American patients undergoing Roux-en-Y gastric bypass and also to evaluate the utility of different serum markers including FIBROspect II to detect significant liver fibrosis in this population. A secondary goal of our study is to evaluate the diagnostic value of ultrasound in morbid obese patient with NAFLD.
Materials and Methods
We performed a retrospective chart review of all patients that underwent Roux-en-Y gastric bypass at Valley Baptist medical center in Harlingen, Texas, during a 24-month period (2005–2006).
-
Inclusion criteria includes all patients that had a Roux-en-Y gastric bypass between 2005 and 2006 with a body mass index (BMI) >40 kg/m2 or a BMI greater than 35 kg/m2 with significant co-morbidities like diabetes mellitus, hypertension, metabolic syndrome, hyperlipidemia, and could show that dietary attempts at weight control were ineffective.
-
Exclusion criteria includes BMI <40 with no co-morbidities.
Data Collection
All data was obtained from patients’ charts at the surgeon’s office. Patients were evaluated for height, weight, and BMI on their first visit and at 15 days and 1, 3, 6, 12, and 24 months. Patients had the following laboratory values measured by the same laboratory previous to their surgery: albumin, alkaline phosphatase (ALK), aspartate aminotransferase (AST), alanine aminotransferase (ALT), gamma-glutamyl transferase (GGT), lactate dehydrogenase (LDH), bilirubin, blood urea nitrogen, calcium, glucose, phosphorus, total protein, uric acid, international normalized ratio, partial thromboplastin time, triglycerides, high density lipoproteins, low density lipoproteins, and cholesterol. Also, a complete blood count, iron, ferritin, vitamins A, D, and B1, and complete urinalysis were obtained on their first visit. FIBROspect score II was routinely ordered and obtained only on patients that had insurance approval. All patients with no history of cholecystectomy had a preoperative right upper quadrant ultrasound to evaluate for steatosis and cholelithiasis.
Gastric Bypass and Liver Biopsy
All patients that met eligibility criteria published by the National Institute of Health consensus guidelines for the treatment of the morbidly obese patient underwent gastric bypass surgery. The pouch and the Roux-en-Y loop were all constructed under the same technique and by the same surgeon. All the patients had an intraoperative needle liver biopsy performed routinely.
Pathology
At least two fragments were obtained from each liver biopsy; they were sent to pathology in Bouin’s fixative. All the biopsies were stained with hematoxilin and eosin, trichrome, and iron. The Kleiner–Brunt classification system was used to evaluate for NASH and for liver fibrosis. The classification included grading of macrovesicular steatosis (NASH grade) and staging of liver fibrosis (fibrosis stage). NASH grade 0 corresponded to no steatosis, NASH grade 1 up to 33%, NASH grade 2 from 33% to 66%, and NASH grade 3 more than 66%. In the fibrosis staging system, stage 0 corresponded to no fibrosis; stage 1, perisinusoidal/pericellular fibrosis, focally or extensively present; stage 2 perisinusoidal/pericellular fibrosis with focal or extensive periportal fibrosis; stage 3, perisinusoidal/pericellular fibrosis and portal fibrosis with focal or extensive bridging fibrosis; and stage 4, cirrhosis.
Statistical Analysis
All the data was stored in Microsoft Office Excel 2008 data sheet. Statistical Package for the Social Sciences 17.0 for windows was used for statistical analysis. A bivariate Pearson correlation was used to compare the different variables, and t student test was used to evaluate for difference of the means. Multiple regression analysis was used for all the independent variables to assess the predicting value for liver fibrosis. A p value <0.05 was considered statistically significant.
Results
A total of 129 underwent Roux-en-Y gastric bypass during the study period, and all had routine liver biopsy performed. Eighty-seven patients were Hispanics, and 42 were Caucasians. One hundred four were females, and only 25 patients were males. The mean age of the patients was 41 for Hispanics and 50 for Caucasians (p < 0.05). The mean BMI was 49 for Hispanics and 46 for Caucasians (p = 0.067).
Prevalence of Nonalcoholic Fatty Liver Disease in Morbidly Obese Patients
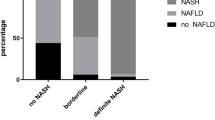
Of 129 liver biopsies, only 25.7% had some degree of steatosis, but about 55% had NASH, and 30.9% had liver fibrosis. Of those patients with liver fibrosis, only 6.9% had moderate to severe fibrosis (stages 2–4), and only one patient had cirrhosis (0.7%; Table 1). When evaluated by race of the 42 Caucasian patients, 17 (40%) had simple steatosis, 20 (47%) had some degree of NASH, and nine (21%) had liver fibrosis. Of 87 Hispanic patients, 16 (18%) had simple steatosis, 51 (58%) had some degree of NASH, and 31 (35%) had liver fibrosis. (Note: In both groups, several patients had some degree of NASH and also liver fibrosis).
Right Upper Quadrant Ultrasound for Diagnosis of NASH
A total of 102 abdominal ultrasounds reports were reviewed. Only 36 had the diagnosis of fatty liver in their report. Twenty-one of 52 patients with grades 1–3 of NASH had the diagnosis of fatty liver by ultrasound. Of the nine patients with stages 2–4 fibrosis, only two had the diagnosis of fatty liver disease by ultrasound (Table 2).
FIBROspect II® Score
Of the 129 patients included in our study, only 92 had a FIBROspect II® score in their chart, and they ranged from 9 to 95, with a mean of 28.3. The one patient with cirrhosis had a FIBROspect II score of 55. Thirty-six patients had a score less than 20, and none had significant fibrosis in their biopsy. Using a cutoff of <20, FIBROspect II® had a negative predictive value (NPV) of 100% (confidence interval (CI) 95%, 0.90–1), positive predictive value (PPV) of 15% (CI 95%, 0.08–0.26), sensitivity of 100%, and specificity of 42% to predict liver fibrosis stage 2 or higher. The accuracy of the test was 46.7%. The likelihood ratio for a positive test result was 1.73, and likelihood ratio for a negative test result was 0 (Table 3). Of the 37 patients that had no FIBROspect score II recorded in their chart, only one had stage 2 fibrosis, the rest had stage 0 or 1. Also, none of these patients had NASH grade higher than 2.
Predictors of Liver Fibrosis
Using Pearson coefficient to evaluate linear correlation between liver function test, BMI, age, and degree of NASH with stage of liver fibrosis (from 0 to 4), only four variables had correlation with the severity of liver fibrosis: FIBROspect II® score, NASH grade, AST, and BMI lost at 6 and 12 months (Table 4). Also important to notice is that age had a significant positive correlation with the FIBROspect II score.
Given that the degree of NASH is part of the NAFLD scoring system and that BMI at 6 months and 1 year are data obtained postoperatively, they were not considered for a multiple regression analysis since they cannot be used to predict the degree of fibrosis preoperatively.
When using multiple regression analysis, FIBROspect® score II and AST predicted the amount of fibrosis with a p = 0.002. The coefficient for FIBROspect was 0.014 (CI 95%, 0.005–0.02), and the constant value was 0.004 (CI 95%, −0.278–0.286). A receiver operating characteristic curve (ROC curve) was done for AST and FIBROspect II to evaluate their ability to discriminate between minimal fibrosis and significant fibrosis. The area under the curve (AUROC) for FIBROspect was 0.7 and for AST was 0.5 (Fig. 1).
When comparing the means for all the variables in patients with stages 0–1 vs stages 2–4, we found that FS II, BMI, BMI at 6 months, and BMI at 1 year were all significantly different in both groups. Patients with moderate to severe fibrosis had a higher FS II and a higher BMI at 0, 6 months, and 1 year. The age in the group with significant degree of liver fibrosis was higher but with a p < 0.10 (p = 0.062; Tables 5 and 6).
Discussion
Out study shows that NASH has a high prevalence in the morbidly obese population, especially in the Hispano-American population; this is a similar to what other studies have speculated. In our Hispanic population, 58% of the patients had some degree of NASH, and about 35% had some degree of fibrosis. The only patient that had cirrhosis was Hispanic [6, 8–10]. Adding the patients with steatosis and NASH, approximately 80% of the patients had some degree of fatty liver disease, which is also similar to what the literature describes [6]. When comparing the Caucasian population to the Hispanic population, our results showed a trend towards having a higher degree of NASH and fibrosis in the Hispanic population, but this was not significant, and this results could be in part due to a small sample and the fact that the Caucasian population in our study was significantly older than the Hispanic population. When comparing the percentage of NASH in both populations, the Hispanic patients had higher prevalence of steatohepatitis and also of liver fibrosis, in contrast to the Caucasian patients that had more prevalence of simple steatosis.
Based in our results, patients with moderate to severe fibrosis tend to be significantly older and to have a higher BMI and FIBROspect® score II. These results can be used to select the high-risk patients for significant liver fibrosis or advanced NAFLD and perform liver biopsies only in this group. Also, these patients should have a close follow-up since they can develop cirrhosis in the future, but more studies are needed to differentiate which patients will have regression of their liver disease with bariatric surgery and which ones will progress to cirrhosis.
Our study shows that patients with higher degree of fibrosis and with higher FIBROspect score II will have a significantly higher BMI at 6 months and 1 year post-Roux-en-Y gastric bypass, suggesting that liver fibrosis plays a role in the failure of obesity surgery. The exact pathophysiology for these is not very well known, but having a pathologic liver metabolism plays an important role in weight loss after bariatric surgery. The effect of liver fibrosis in the long-term follow-up is unknown, and further research is needed to elucidate in this matter.
One of the most interesting findings in our results was that the sensitivity and specificity of the right upper quadrant ultrasound was very poor (40% and 70%), making the test an unreliable tool for screening of fatty liver disease. Also interesting is that many patients that were diagnosed with fatty liver by ultrasound had no evidence of NASH by pathology diagnosis. This could be attributable to operator-dependant skills or to a sample error in the biopsies, although similar results have been found in previous studies showing that ultrasound should not be the only tool to screen for fatty liver disease [11].
When using only the liver enzymes, it becomes very difficult to rule out significant fibrosis (stages 2–4) without a liver biopsy [9]. Previous studies have used algorithms and equations that include AST and ALT but the negative predictive value was not higher than 88% [12]. When using the FIBROspect score II (cutoff <20), high degree of fibrosis (stages 2–4) can be ruled out with a negative predictive value of 100%. In patients with chronic hepatitis C, the FIBROspect® score II had similar results. When using a cutoff point extremely low (<20), FIBROspect II also had a very high NPV in patients with chronic hepatitis C [14, 16, 17]. The ROC curve in our results shows that the AUROC for AST was close to 0.5; when the AUROC is equal to 0.5, that means it cannot discriminate between disease and no disease. On the other hand, the AUROC for the FIBROspect was 0.7 indicating that it can discriminate between significant disease and mild disease, but in our finding, the PPV was low. We have found a noninvasive test that can be used to rule out significant disease in patient with morbid obesity and high-risk factors for liver disease. The use FIBROspect® II score has become part of our practice since it is a simple and easy way to avoid liver biopsy in morbidly obese patients that have high-risk factors for NAFLD. Its use is to rule out significant disease; FIBROspect II score cannot be used solely to diagnose advanced fibrosis or cirrhosis; our only patient with cirrhosis did have a higher score than 20, but was not the highest score (55), in contrast to patients with hepatitis C, where a very high score would have a very high PPV for advanced liver fibrosis [16, 17].
Limitations of our study include a relatively small sample and short-term follow-up. The majority of our patients were Hispanic, and the use of FIBROspect II® score in other populations might not show the same results. Another limitation is that only 92 of the 129 patient had a FIBROspect score II in their chart, but we believe it is unlikely that our study is bias from this since only one of the 37 patients without the test had moderate fibrosis. Long-term follow-up to evaluate the progression of liver disease would be ideal and also would help to evaluate the role of gastric bypass in treating fatty liver disease.
An incidental finding not related to the aims of this study was that morbid obese patient with moderate to severe fibrosis will have less weight loss at 6 and 12 months after Roux-en-Y gastric bypass.
Conclusions
NASH and liver fibrosis are present in a high percentage of morbidly obese patients. Liver function tests and ultrasound are not reliable diagnostic tests of advanced liver fibrosis. The use of FIBROspect® II score in the preoperative evaluation of morbidly obese patients can rule out significant liver fibrosis (stages 2–4) and avoid the morbidities related to liver biopsy. It could be used in high-risk patients as a screening tool.
References
Flegal KM, Carroll MD, Ogden CL, et al. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002;288:1723–7.
Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–55.
Residori L, Garcia-Lorda P, Flancbaum L, et al. Prevalence of co morbidities in obese patients before bariatric surgery: effect of race. Obes Surg. 2003;12:333–40.
Guajardo-Salinas, et al. Predictors of weight loss and effectiveness of Roux-en-Y gastric bypass in the morbidly obese Hispano-American population. Obes Surg. 2008;18(11):1369–75.
Allison DB, Fontaine KR, Manson JE, et al. Annual deaths attributable to obesity in the United States. JAMA. 1999;282:1530–8.
Diehl AM. Hepatic complications of obesity. Gastroenterol Clin North Am. 2005;34:45–61.
Amarapurkar DN, Hashimoto E, Lesmana LA, et al. How common is non-alcoholic fatty liver disease in the Asia-Pacific region and are there local differences? J Gastroenterol Hepatol. 2007;22(6):788–93.
Bacon BR, Farahvash MJ, Janney CG, et al. Nonalcoholic steatohepatitis: an expanded clinical entity. Gastroenterology. 1994;107(4):1103.
Gholam PM, Flancbaum L, Machan JT, et al. Nonalcoholic fatty liver disease in severely obese subjects. Am J Gastroenterol. 2007;102:399–408.
Mottin, et al. Histological behavior of hepatic steatosis in morbidly obese patients after weight loss induced by bariatric surgery. Obes Surg. 2005;15(6):788–93.
Almeida AM, Cotrim HP, Barbosa DBV, et al. Fatty liver disease in severe obese patients: diagnostic value of abdominal ultrasound. World J Gastroenterol. 2008;14:1415–8.
Angulo P, Hui JM, Marchesini G, et al. The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology. 2007;45(4):846–54.
Imbert-Bismut F, Ratziu V, Pieroni L, et al. Biochemical markers of liver fibrosis: a prospective study. Lancet. 2001;357:1069–75.
Christensen C, Bruden D, Livingston S, et al. Diagnostic accuracy of a fibrosis serum panel (FIBROSpect II) compared with Knodell and Ishak liver biopsy scores in chronic hepatitis C patients. J Viral Hepatitis. 2006;13(10):652–8.
Bravo A, Sheth S, Chopra S. Liver biopsy. N Engl J Med. 2001;344(7):495–500.
Zaman A, Rosen H, Ingram K, et al. Assessment of FIBROspect II to detect hepatic fibrosis in chronic hepatitis C patients. Am J Med. 2007;120(3):280.e9–e14.
Patel K, Gordon SC, Jacobson I, et al. Evaluation of a panel of non-invasive serum markers to differentiate mild from moderate-to advanced liver fibrosis in chronic hepatitis C patients. J Hepatol. 2004;41:935–42.
Conflict of interest statement
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guajardo-Salinas, G.E., Hilmy, A. Prevalence of Nonalcoholic Fatty Liver Disease (NAFLD) and Utility of FIBROspect II to Detect Liver Fibrosis in Morbidly Obese Hispano-American Patients Undergoing Gastric Bypass. OBES SURG 20, 1647–1653 (2010). https://doi.org/10.1007/s11695-009-0027-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-009-0027-0