Abstract
Background
Among bariatric restrictive operations, the procedure of choice is still controversial. The aim of this study is to compare the cost of two gastric restrictive procedures: laparoscopic vertical banded gastroplasty (LVBG) and laparoscopic adjustable gastric banding (LAGB).
Methods
This is a prospective nonrandomized study comparing the cost effectiveness of LVBG and LAGB. Fifty-nine LVBG are compared to 83 LAGB performed during the same period, September 2005 and August 2006. Both groups demonstrate similar body mass index range and gender distribution.
Results
Cost analysis is evaluated as: preoperative, intraoperative, postoperative, follow-up, and management of complication cost. Both groups have similar preoperative and immediate postoperative cost. The material cost for LVBG is significantly lower than for LAGB ($1,326.42 for LVBG to $3,253.42 for LAGB). This material cost, however, excludes instruments and materials that are used in both procedures. Although both groups have similar postoperative routine visits, LAGB visits require band fills which increase its cost by $28 if fills are by palpation or $179 if by ultrasound. The complications in LAGB were also more severe with four patients returning to the operating room and another one medically managed for pulmonary embolism. These are at a higher cost compared to LVBG where none of the patients require reoperation or readmissions. The rate of percentage excess weight loss in LVBG patients however is more rapid than in LAGB patients.
Conclusions
LVBG required less expensive instruments and materials for the operation and was associated with a higher rate of weight loss and less complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is at an epidemic proportion in the USA and much of the Western world, and surgical management is presently the only effective method of achieving sustainable weight loss. Bariatric surgery can either be restrictive, malabsorptive, or a combination of restrictive and malabsorptive procedure. Laparoscopic adjustable gastric bands (LAGB) and laparoscopic vertical banding gastroplasty (LVBG) are the main restrictive bariatric operations performed at the present time. Although there are many studies comparing these procedures, there is no study to compare their cost effectiveness in the USA. We therefore aim to compare the cost of these two gastric restrictive operations to their achieved weight loss.
Materials and Methods
This is a prospective, nonrandomized study of all the restrictive bariatric operations performed at a single institution by a single surgeon between September 2005 and August 2006. Fifty-nine patients underwent LVBG while 83 individuals had LAGB during the study period. The surgical procedure was chosen by the patient after consultation with the surgeon.
The NIH criteria for obesity surgery are applied. There is at least one preoperative surgical consult for all patients. They are also declared fit for bariatric surgery by the psychologist, dietician, and internist (when indicated). Demographic data, body mass index (BMI), medication, and past medical and surgical history are recorded.
Hospital length of stay (LOS) and both intra- and postoperative complications are recorded. Postoperative gastrograffin swallow is performed in all patients on the first postoperative day (POD). The follow-up regimen is at 10–14 days, 6–8 weeks, then at 3, 6, 9, and 12 months postoperatively. Patients who miss the follow-up schedule are invited again by the secretary team to participate in follow-up evaluations.
Surgical Technique
Anesthetic techniques are similar for both groups. All patients received a preoperative antibiotic.
Five 10-mm ports are placed in the upper abdomen and a self-retaining retractor holds the left liver lobe. The peritoneal fold at the angle of His is incised and a window is created at the angle of His. The position of the circular stapler is measured 5 cm below the angle of His and 3 cm from the lesser curvature. A window is made at this level through the lesser omentum adjacent to the nerve of Laterjet. The left midline port is dilated to allow the circular stapler introduction. A 32 French gauge (Fr) nasogastric tube (NGT) is passed through the staple line to ensure adequate outlet and guide the linear stapling and division of the gastric pouch to the angle of His. The staple lines of the pouch, remnant, and circular stapler portion are then reinforced with sutures. The outlet is reinforced with a 5 × 1.5-cm lightweight partially absorbable (poliglecaprone–polypropylene) mesh, sutured with three nonabsorbable sutures, with the 32Fr NGT in place to calibrate the stoma. The mean operating time is 94.1 ± 13.5 min.
For the LAGB, the standard pars flaccida approach is used. Five ports are used as well as a self-retaining retractor to elevate the left lobe of the liver. One of the ports is a 15-mm port through which the band itself is inserted. A window is created at the angle of His. The transparent portion of the lesser omentum (pars flaccida) is opened. A small opening is made in the peritoneum just medial to the most inferior aspect of the right crus as it disappears into the retroperitoneal fat. Care is taken to distinguish this structure from the inferior vena cava. A long grasper is inserted at this opening to exit at the opening made at the angle of His. The band is inserted in this position and locked in place and anterior gastrogastric sutures are placed. The port is then secured in the rectus sheath after the tubings are connected. The mean operating time is 75.1 ± 10.3 min.
Statistical Analysis
The Mann–Whitney–Wilcoxon rank-sum test was used to analyze differences between preoperative and postoperative values. The Fisher exact test was used to analyze the difference in postoperative complications between both groups.
Results
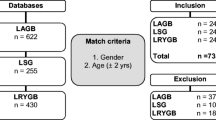
There is no statistically significant difference in the groups in terms of demographics: age, gender, or BMI range (Table 1, Fig. 1). The percentage excess weight loss (%EWL) in the LVBG group is significantly higher than in the LAGB group in the first year of follow-up (Table 2).
Preoperative Cost
The preoperative cost for both procedures is similar; they underwent the same preoperative work up. This includes the initial bariatric surgeon office visit, preoperative laboratory testing, nutritional assessment and counseling, psychiatric evaluation, and esophagogastroduodenoscopic assessment.
Intraoperative Cost
In calculating the intraoperative cost, we exclude the cost of operating room (OR) equipment or instruments that are common to both procedures, the cost of reusable OR equipment, and the cost of equipment, medications, and materials used by the anesthesiologist. We also exclude personnel cost and the cost of OR space and time.
Intraoperative cost analyses therefore include only cost of instruments or materials specific to either LVBG or LAGB. LVBG-specific materials cost $1,326.42 while the cost of LAGB-specific materials is $3,253.44, a significant difference (p < 0.01). The cost of the band used in LAGB was $2,725.45
Immediate Postoperative Cost
The costs of managing the patients in the immediate postoperative period are also similar. This is because both groups needed the same nursing care and postoperative medication. Both study groups have gastrograffin upper gastrointestinal study on the first postoperative day.
Although some patients in the LVBG group were discharged on postoperative day (POD) 3 during the learning phase, most patients are discharged on POD 1. There was no statistically significant difference in the hospital length of stay (Table 3) after both procedures.
Follow-up Cost
The follow-up schedule for both LVBG and LAGB are the same, they are on POD 10 to 14, then at 4 weeks, 6–8 weeks, 12–16 weeks, and every 3 months for 1 year and annually afterwards.
The difference in the amount of money necessary to follow-up these patients is in the cost of performing band fills for the LAGB study group. The number of band fills in each of the LAGB patient is shown in Fig. 2, while Table 4 depicts the band fills done with ultrasound (US) guidance and the cost of these band fills when performed using ultrasound.
Band fills cost $28 when it is performed by palpation or $179 when the bands are filled using US guidance. Eighty-five percent of the time band fills is performed under US guidance. Only 12 times (15%) were band fills done by palpation, making a total of $336 for band fills by palpation. The total cost of filling the bands in the LAGB patients is therefore $22,460, an average of extra $362 per patient ($22,460/number of patients).
Cost of Complications Work-up and Management
Table 5 reveals the postoperative complications and symptoms in the groups. Table 6 shows the main diagnostic study performed to work up the postoperative complications, the cost of each work up, and the number of patients requiring each diagnostic study in the study groups, while Table 7 shows the total cost of this work up. There is no statistically significant difference in the cost of diagnostic work up postoperatively per study group.
None of the patients in the LVBG group needed to return to the OR while four patients in the LAGB group went back to the OR. The first was for control of port site hemorrhage and the second for band removal and drain placement for esophageal injury, with a subsequent OR visit necessary for better placement of the drains. The third went back to the OR for drainage of a subhepatic abscess and band removal for band erosion. The last patient needed her flipped port re-anchored to the rectus sheath because it could not be assessed for fills.
Also one patient in the LAGB group was admitted for work up and treatment of pulmonary embolism whereas there was no readmission necessary for any of the LVBG patients.
Discussion
Adjustable gastric banding and vertical banded gastroplasty are the commonly used restrictive surgical procedure in obesity surgery [1, 2].
Vertical banded gastroplasty (VBG) has been in clinical use since 1979 and adjustable gastric banding (AGB) since 1985 [3]. Currently, both restrictive procedures are performed laparoscopically [3].
Although both are credited with achieving weight loss in morbidly obese patients, there is a greater weight loss during the first 6–12 months with VBG [3]. In the intermediate period, 2 to 3 years after surgery, patients who had VBG are able to achieve and maintain their weight loss [4, 5].
The percentage of patient who achieved and maintained ≥50% EWL in a 5-year prospective comparison of VBG and RYGBP was not statistically different [6]. AGB as well has been shown to achieve weight loss comparable to RYGBP after about 5 years follow-up though the rate of weight loss is noted to be slower [7, 8]. VBG results in an excess weight loss of approximately 60%, an improved quality of life, and decreased obesity-related comorbidity [4, 9–13]. VBG is more effective in terms of late complications, reoperations, and weight loss when compared to AGB [14].
VBG has been better studied than AGB since it has been in existence longer. Its complications and failures as well as the reasons for such are well documented. When performing LVBG, we take steps to address these reasons.
We used a six-row linear stapler with division in between the staple line to ensure complete division of the gastric pouch in VBG. We also oversew the whole staple line, thereby reducing the possibility of staple line dehiscence, leak, gastrogastric fistula, weight regain, and reflux which were noted to be the causes of significantly high reoperation rate in VBG by MacLean et al. [6, 15, 16].
These two factors, using a six-linear stapler and oversewing the staple line, are the major difference in our study and that of Van Dielen et al. They reported a 6% leak rate and a subsequent 2% mortality rate following the leak in contrast to the absence of leaks or mortality in the present study. They also had a staple line disruption in 33% necessitating reoperation which did not occur in our study just by applying the factors above [17].
Miller et al. in their study had two deaths in the VBG and one death in the AGB group in 30 days. The VBG group had higher %EWL after 12 months but a higher reintervention rate than the AGB [3]. However, in that study, they compared open VBG and LAGB. The complications that reached statistical significance such as hematoma, wound infection, and incisional hernia were related to the fact that VBG was an open procedure. Staple line dehiscence was likewise common in their study (22%) because the stomach, though stapled off, was not divided. Using only one TA 90 does not also ensure it was completely stapled off. We completely staple off the stomach, divide it, and reinforce both staple lines with sutures. The other significant complications of outlet stenosis and pouch dilatation in their study were likely due to the outlet stenosis which was uncommon in our experience because we created our outlet ensuring a 32-Fr nasogastric tube could pass through the outlet we created while they estimated instead of measuring all the time.
Pasnik et al. described a staple line dehiscence of 1.5%, using the TA 90 [18] (compare this to Miller’s study). We did not have any staple line dehiscence using the GIA six-row stapler, with divisions and suture reinforcement of the staple lines.
Our study is comparable to the findings of Kuhlmann et al. in their paper “Cost effective bariatric surgery in Germany today” where they discovered that LVBG was the most cost-effective restrictive bariatric operation in Germany. It was less costly by over $1,200 but equally effective in reduction of comorbidities and mortality when compared to LAGB [19].
Pasnik et al. reported VBG to be less expensive in Poland when compared to gastric banding and gastric bypass [18]. VBG has provided significant weight reduction and improved quality of life in the majority of morbidly obese Polish patients [18].
Van Gement et al. estimated the operative cost (excluding hospital stay, endoscopy, physical therapy, laboratory, radiology, outpatient visits) of open VBG in the Netherlands at about $3,000 in 1999 [4], and you will then wonder how much it will cost when done laparoscopically in the USA and about a decade later, yet it is less expensive when compared to the adjustable gastric band.
Naslund et al. reported an operating time for LVBG of between 85 and 225 min and length of stay of 2–6 days [5], while Morino et al. noted a mean length of stay of 3.7 days in LAGB and 6.6 days in LVBG [14], which were too long compared to our mean length of stay of 1.5 days for LVBG and 1.1 days for LAGB.
This is the first cost analysis comparing the two main restrictive bariatric procedures in the USA. Only the Netherlands has a similar study in all English literature. There are similarities as well as differences in our study and those of Van Mastrigt et al.’s Netherlands study [20] on cost effectiveness of LVBG versus LAGB. We discovered that the material and operative cost for LAGB were higher compared to the material and operative cost of the LVBG. We also both noted that the cost of outpatient care was higher in the LAGB group due to the band inflating procedure.
However, in the study of Van Mastrigt et al., the LOS in the LAGB group was significantly shorter compared to LVBG, while there was no significant difference in our study. Also, although about the same number of patients in the LAGB group of both studies requires reoperation, 11 patients in their LVBG group required reoperation for immediate postoperative complications such as splenectomy and perforation whereas none of our LVBG patients needed reoperation whether in the immediate period or within a year postoperatively.
They had 2% mortality in their LVBG group while there was no mortality in ours. There was no death in the LVBG or the LAGB group in our study [20].
In summary, this study shows that per patient LAGB costs $1,927 more intraoperatively, $336 more for follow-up, and $8.7 more for work up in case of complications when compared to LVBG. Also LAGB complications require a return to the OR on more occasions than with LVBG.
This study is however limited because the total cost of each procedure could not be computed; therefore, only the cost of the materials, procedures, and studies that were peculiar to each procedures were calculated. Moreover, only 72% in the LVBG group and 75% in the LAGB group completed the follow-up schedule. Also most of the band fills were done by ultrasound guidance. Furthermore, a long-term follow-up will be necessary. We hope to report our findings at 3 and 5 years after the initiation of this study.
In conclusion, LVBG costs less to perform and maintain postoperatively while achieving a higher weight loss than LAGB in a short-term period and a longer-term study will be necessary.
References
Council on scientific affairs. Treatment of obesity in adults. JAMA 1988;260:2547–51.
Buchwald H, Williams SE. Bariatric surgery worldwide 2003. Obes Surg. 2004;14:1157–64.
Miller K, Pump A, Hell E. Vertical banded gastroplasty versus adjustable gastric banding: prospective long-term follow up study. Surg Obes Relat Dis. 2007;3:84–90.
Van Gement WG, Adang EMM, Kop M, et al. A prospective cost-effective analysis of vertical banded gastroplasty for the treatment of morbid obesity. Obes Surg. 1999;9:484–91.
Naslund E, Freedman J, Lagergren J, et al. Three year results of laparoscopic vertical banded gastroplasty. Obes Surg. 1999;6:369–73.
Kalfarentozos F, Skroubis G, Kehagias I, et al. A prospective comparison of vertical banded gastroplasty and Roux-en-Y gastric bypass in a non-superobese population. Obes Surg. 2006;16:151–8.
Galvani C, Gorodner M, Moser F, et al. Laparoscopic adjustable gastric band versus laparoscopic Roux-en-Y gastric bypass: ends justify the means. Surg Endosc 2006;20(6):934–41.
Jan JC, Hong D, Bardaro SJ, et al. Comparative study between laparoscopic adjustable gastric banding and laparoscopic gastric bypass: single-institution, 5-year experience in bariatric surgery. Surg Obes Relat Dis. 2007;3(1):42–50.
Kral JG, Sjostrom LV, Sullivan MBE. Assessment of quality of life before and after surgery for severe obesity. Am J Clin Nutr 1992;55:611S–4S.
Van Gemert WG, Adang EMM, Greve JWM, et al. Quality of life assessment of morbidly obese patients: effects of weight reducing surgery. Am J Clin Nutr. 1998;67:197–201.
Mason EE, Maher JW, Scott DH, et al. Ten years of vertical banded gastroplasty for severe obesity. Probl Gen Surg. 1992;9:280–9.
Van Gemert WG, Greve JWM, Soeters PB. Long term results of vertical banded gastroplasty: Marlex versus Dacron banding. Obes Surg. 1997;7:128–35.
Brolin RE. Results of obesity surgery. Gastroenterol Clin North Am. 1987;16:317–37.
Morino M, Toppono M, Bonnet G, et al. Laparoscopic adjustable silicon gastric banding versus vertical banded gastroplasty in morbidly obese patients: a prospective randomized controlled clinical trial. Ann Surg. 2003;238:835–42.
MacLean LD, Rhode BM, Forse RA. Late results of vertical banded gastroplasty for morbid and super obesity. Surgery 1990;107:20–7.
MacLean LD, Rhode BM, Forse RA, et al. Surgery for obesity—an update of a randomized trial. Obes Surg. 1995;2:145–8.
Van Dielen FMH, Soeters PB, de Brauw LM, et al. Laparoscopic adjustable gastric banding versus open vertical banded gastroplasty: a prospective randomized trial. Obes Surg. 2005;15:1292–8.
Pasnik K, Krupa J, Stanowski E. Vertical banded gastroplasty: 6 years experience at a center in Poland. Obes Surg. 2005;15:223–7.
Kuhlmann HW, Falcone RA, Wolf AM. Cost effective bariatric surgery in Germany today. Obes Surg. 2000;10:549–52.
Van Mastrigt GAPG, Van Dielen FMH, Severens JL, et al. One year cost-effectiveness of surgical treatment of morbid obesity: vertical banded gastroplasty versus lap band. Obes Surg 2006;16:75–84.
Disclosure
There are no financial interests that may lead to conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ojo, P., Valin, E. Cost-Effective Restrictive Bariatric Surgery: Laparoscopic Vertical Banded Gastroplasty Versus Laparoscopic Adjustable Gastric Band. OBES SURG 19, 1536–1541 (2009). https://doi.org/10.1007/s11695-008-9771-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-008-9771-9