Abstract
Background
Restrictive bariatric operations are efficient with low morbidity but entail high rate of failure on follow up of several years. We present our experience in laparoscopic revision of patients who previously underwent silastic ring vertical gastroplasty (SRVG) into laparoscopic sleeve gastrectomy (LSG) and Roux-en-Y gastric bypass (LRYGB).
Methods
Data on 12 patients who underwent revisional operations after SRVG was prospectively collected. Six patients underwent LRYGB and six patients underwent LSG. The pathogeneses for failures of SRVG were disruption of staple line, enlargement of gastric pouch, and opening of the ring.
Results
The average age and body mass index (BMI) were 39 and 43, respectively, in the LSG group versus average age and BMI of 39 and 45, respectively, in the LRYGP group (p = 0.45 and p = 0.35, respectively). The average operative time were 206 and 368 min in the LSG and LRYGB groups, respectively (p < 0.01). There were five postoperative complications among LSG group versus two complications in LRYGB group (p < 0.01). Patients who underwent LSG suffered from the following complications: staple line leak in two patients, intra-abdominal hematoma in one patient, intra-abdominal collection in one patient, and gastric outlet obstruction in one patient. Anastomotic leak and wound infection were the complications seen among patients underwent LRYGB. All complications were treated conservatively without necessitating immediate reoperations. Follow-up has shown adequate reduction of body weight and improved quality of life in both groups of patients.
Conclusions
Revisional bariatric operation is a challenging laparoscopic procedure with higher morbidity compared to primary bariatric operations. Morbidity of LSG compared to LRYGB as a revisional procedure for SRVG is significantly higher.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
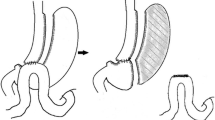
Obesity is a worldwide epidemic disease. Bariatric operations for patients who suffer from morbid obesity are effective in reducing body weight and comorbidities. Today, there is an arsenal of several surgical options for inducing weight loss. In the past, silastic ring vertical gastroplasy (SRVG) and vertical band gastroplasty (VBG) have been common surgical procedures. Their mechanism for weight loss is limitation of food intake by restriction of passage of food through the stomach. These procedures necessitated laparotomy and have been shown to be followed by a relatively low morbidity and mortality. However, long-term follow-up has shown unsatisfying weight reduction [1]. The reasons for failure of these restrictive procedures, other than noncompliance of the patients, were disruption of the staple line which caused ring or band bypass of food without restriction, gradual enlargement of the proximal pouch which provided the pouch with the characteristics of normal stomach as a reservoir organ for food, and tear or opening of the silastic ring which may have abolished the restriction. Due to the wide use of these procedures in the past, combined with its high failure rate, bariatric surgeons are faced with an growing number of patients who necessitate revision operation as a rescue procedure [2–5]. Proposed surgical procedures for revision of failed previous vertical gastroplasties [6] are redo gastroplasty, addition of an adjustable band over the existing pouch, or conversion into a combined restrictive and malabsorptive procedure—gastric bypass [7, 8], standard biliopancreatic diversion (BPD), or duodenal switch (DS) [9]. Also, laparoscopic approach to perform the revision is desirable. The first two procedures are susceptible to a high rate of failure. Open gastric bypass is a very tenable option and provides additional long-lasting weight loss. Several series of laparoscopic performance have been reported, but the procedure is challenging with a long operative time. In our experience, laparoscopic conversion of failed vertical gastroplasty into gastric bypass was feasible and safe, but due to long operating time, an attempt to convert to a sleeve gastrectomy instead was made.
For several years, laparoscopic sleeve gastrectomy (LSG) has been proposed as single stage operation [10]. In the past, this procedure was presented as a modification of BPD and was combined with DS [11]; however, it necessitated extensive surgical procedure. Observations and studies have shown that patients who underwent this first stage procedure achieved adequate weight loss. According to this finding, LSG alone has become a weight reduction procedure with low morbidity [12].
Searching the English medical literature has shown several studies which described LSG as revision procedure for failed BPD–DS [13] and gastric banding [14], but none as a remedial operation for a failed SRVG/VBG. In this article, we describe our results of performing LSG as a revision procedure for six patients who underwent SRVG which failed. We also describe our experience with relatively high postoperative complications.
Materials and Methods
Patients
All patients who were operated between January 2006 and December 2007 were enrolled in the study. The diagnosis of failure of previous SRVG has been done leaning on the weight loss failure or weight regain when patient reached the criteria for bariatric surgery as coined by National Institutes of Health Consensus Conference. Preoperative workup, besides the regular bariatric surgery candidate’s battery, included upper endoscopy, upper gastrointestinal barium swallowing studies, and, in some cases, abdominal computed tomography scans. All patients were interviewed by a dietitian and psychiatrist in order to rule out noncompliance as reason for inadequate weight loss. Patients, who suffered from failure of previous SRVG without known anatomical reason and were found to be compliant, were also included in the study (Table 3).
Study Design
Patients who underwent LSG (RLSG) were compared to patients who underwent laparoscopic Roux-en-Y gastric bypass (LRYGB) during the same period of time by the same surgeon. Data collected included demographic characteristics (Table 1), indications for revision (Table 2), perioperative variables with a special stress put on complications, and follow-up. The t test and Fisher’s exact test were used to compare continuous variables. A p value of 0.05 or less was considered statistically significant. Statistical analysis was achieved using the SPSS version 11.5 (Statistical Package for Social Science, Chicago, IL, USA).
Surgical Procedures
All operations were attempted laparoscopically. All procedures started from complete dissection of the adhesions around the stomach. The silastic ring was identified, divided, and removed. The old staple line was usually delineated without difficulty, sometimes facilitated by filling the stomach with water through the nasogastric tube.
LRYGB was performed using six–nine trocars (5–12 mm, Excell, Ethicon Endosurgery, Cincinnatti, OH, USA). The procedure started with stomach pouch construction, using a staple (blue or green load, ETS-Flex, EndoGIA 45 mm Ethicon Endosurgery, Cincinnatti, OH, USA). The proximal pouch was constructed to a volume of ∼20–30 cm3. An attempt has always been made to cut the stomach proximally to the old staple line. After pouch construction, we proceeded to divide the jejunum 40 cm distal to the Treitz’s ligament (white load, EndoGIA 45 mm, Ethicon Endosurgery, Cincinnatti, OH, USA) and performed side-to-side jejunojejunostomy anastomosis with the same stapler and hand-sewn closure of the common enterotomy by continuous Prolene 3/0. The mesenterium defect was closed by silk 3/0 continuous suture. Gastrojejunal anastomosis between the gastric pouch and the Roux limb was achieved by two layers of continuous Vicryl 3/0 and Prolene 3/0. Intraoperative examination of the gastrojejunal anastomosis was done by inflating the gastric pouch with methylene blue. Closed suction drain (Jackson Pratt) was placed near the gastrojejunal anastomosis.
LSG was performed using five–eight trocars (5–12 mm, Excell, Ethicon Endosurgery, Cincinnatti, OH, USA). The omentum adjacent to the whole length of the greater curvature and splenic short gastric vessels were divided by Harmonic scalpel (Ethicon Endosurgery, Cincinnatti, OH, USA). A 38-Fr gastric bougie was inserted to the pylorus. Longitudinal stomach division was done starting 2–3 cm proximally to the pylorus by consecutive application of an endoscopic stapler (Blue and green load, EndoGIA 45 mm, Ethicon Endosurgery, Cincinnatti, OH, USA) parallel to the bougie, up to the gastroesophageal junction. Two closed suction drains (Jackson Pratt) were placed near the staple line. In both procedures, water soluble contrast swallow leak test was performed at the first post operative day and a semiliquid diet was initiated if anastomotic or staple line leakage was ruled out.
Results
Six patients underwent revision of a failed previous SRVG operation into gastric bypass (RLRYGB). Indications for revision of the failed SRVG were: (Table 2) two patients displayed staple line disruption and one patient has proximal pouch enlargement. The reason for failure of the other three patients was not defined. In three patients the operation was completed laparoscopically, in two, a 6–7-cm incision was required to complete the gastrojejunal anastomoses, and in one case, conversion to a formal laparotomy was required due to severe adhesions in the upper part of the stomach. An additional six patients underwent laparoscopic conversion of the failed SRVG into sleeve gastrectomy (RLSG). The reasons for failure of SRVG were three patients had an opened or widened silastic ring, two patients had staple line disruption, and one patient had proximal pouch enlargement.
Four of the operations were completed laparoscopically, one was converted into hand-assisted technique due to difficulty in bougie passage, and one was converted into formal laparotomy due to enlarged left liver lobe and difficulty in visualization of the upper stomach. The mean age of patients in both groups was 39 years (Table 1). The mean body mass index (BMI) was 43 in the RLSG and 45 in the RLRYGB (p = 0.35). The average time elapsed between the previous SRVG operation and the remedial procedure were 12 and 9 years, respectively (p = 0.17). The mean operative times were 368 and 206 min in LRYGB and LSG, respectively (p < 0.01). Hospital stay was 5.8 and 8.6 days in LRYGB and LSG, respectively (p = 0.23). The total morbidity rate was 33% and 83% in LRYGB and LSG, respectively (p < 0.01; Table 3). Among the RLRYGB, one patient had leakage from the gastrojejunostomy anastomosis, and one patient had had a surgical wound infection. All complications were treated conservatively without necessitating reoperation. Among the patients in the RLSG, two patients had leakage from the staple line, one patient had intra-abdominal hematoma, one patient had intra-abdominal collection, and one patient had gastric outlet obstruction. Two patients underwent additional operations: one at 2 months and another at 4 months post the conversion procedures for open drainage of a persistent abscess adjacent to the sleeve. There were no mortalities.
Discussion
LSG is becoming an important modality in the armamentarium of bariatric surgery. It was first described as a restrictive component of the BPD–DS. Feng and Gagner presented LSG as the first stage in the staged approach for BPD–DS for super morbid obesity patients [15]. However, LSG was proved to be effective as a stand-alone bariatric procedure on a short-term basis. Restriction of passage for food through the stomach is obviously the major mechanism for weight loss induced by this procedure. Another widely investigated mechanism is reduction of ghrelin level, probably incited by the excision of the gastric fundus [16, 17]. In the short-term follow-up, patients achieved adequate weight loss but there is less data on long-term follow-up to declare that LSG is effective in the long term. Surgeons decide to perform this procedure due to its efficacy and technical simplicity accompanied by relatively low morbidity. The postoperative morbidity of LSG is relatively low but generally caused by breakdown of staple line which leads to leak and bleeding and gastric tube strictures [18].
The feasibility of LSG as a revisional procedure for failed previous bariatric operation has already been published. However, the data are scarce, and there are almost none regarding its morbidity rate and weight loss effect when performed as a remedial operation. Gagner and Rogula reported on repeated LSG (resleeving) as a treatment for weight regain after failure of BPD–DS [13]. Also, an indication for LSG as rescue operation has been described by Bernante et al., who presented this operation as a revision procedure for failed previous gastric banding [14]. There is a relative contradiction for performing repeated restrictive operation after a failure of a previous restrictive procedure. However, since there is a purported neurohumoral effect after performing LSG, it may be used as a revision procedure.
The revision operations are more technically demanding and associated with higher total morbidity than primary bariatric operations. The hypothesized pathogenesis for high rate of complications is the probable existence of dense fibrous tissue at the surgical field which necessitates more dissection and tissue trauma. In our experience, it seems that not only that the proximal part of the stomach is thickened and edematous (the area of previous operation) but also its distal part. One would presume that the distal part should stay relatively virgin, while in fact, this part is as thickened as the proximal stomach. We can hypothesize that some paracrine growth factors secreted by the chronically obstructed upper pouch cause the rest of the stomach to hypertrophy. Manipulation, such as stapling of these stomachs as opposed to primary operations, may not achieve a perfect sealed staple line. The staples may not penetrate both stomach walls, and this condition puts the patient in a higher risk for developing leak and hemorrhage. The fact that RLRYGB group had only one patient who suffered a leak, in contradiction to the RLSG group which had four patients who suffered from leak, hematoma and fluid collection emphasized that there may be differences between these procedures. A major difference between the procedures is the longer staple line in LSG which statistically puts a patient at higher risk for complications. Our impression is supported by the scarce literature available. Deitel et al. reported a much higher leak rate (5.2%) among patients undergoing revision of previous laparoscopic adjustable gastric banding to LSG [19].
There are several possible technical explanations for the higher complication rate that we have observed in the sleeve operations comparing to the bypass procedure. Performing the LSG necessitates dissection of the omentum from the entire greater curvature of the stomach. Nearly all gastric tissue which has been detached from the omentum is resected except for small portion of gastric wall adjacent to the gastroesophageal junction and pylorus. We assume that dissection of the omentum may cause inadvertent damage to the tissue of the stomach, with an immediate intraoperative intent to include this damaged area in the resected specimen. During the procedure, the planned extent of resection is not always fulfilled and that damaged gastric tissue left behind may cause complications.
The reduction in BMI curves of both groups were not statistically different. However, the groups were too small to draw conclusions (Fig. 1). Indeed, the construction of the sleeve in a severely thickened stomach may produce an unpredictable final volume, and it is well known today that the eventual weight loss is determined by the extent of resection.
In conclusion, due to our relative high rate of complications, we refrain from recommending LSG as a procedure for a revision of failed SRVG. Performing the time tested option of LRYGB is a safer choice. The long operative time currently seen, using the laparoscopic approach, will probably shorten after overcoming the learning curve. Another surgical option such as the standard biliopancreatic diversion, probably without a duodenal switch, where a sleeve resection is a part of the operation, would be a viable option. However, there are apparently several faults to the current study. The groups used were small, and the patients’ assignment to the groups was not random. The experience that we present encompasses the learning curve biases, leading the way for larger and randomized studies that may still be required.
References
Kaminski DL. Gastric restrictive procedures to treat obesity: reasons for failure and long-term evaluation of the results of operative revision. Int J Surg Investig 2001;2:413–21.
Brolin RE, Cody RP. Impact of technological advances on complications of revisional bariatric operations. J Am Coll Surg 2008;206:1137–44.
Khaitan L, Van Sickle K, Gonzalez R, et al. Laparoscopic revision of bariatric procedures: is it feasible? Am Surg 2005;71:6–10.
Gagner M, Gumbs AA. Gastric banding: conversion to sleeve, bypass, or DS. Surg Endosc 2007;21:1931–5.
Parikh M, Pomp A, Gagner M. Laparoscopic conversion of failed gastric bypass to duodenal switch: technical considerations and preliminary outcomes. Surg Obes Relat Dis 2007;3:611–8.
Gonzalez R, Gallagher SF, Haines K, et al. Operative technique for converting a failed vertical banded gastroplasty to Roux-en-Y gastric bypass. J Am Coll Surg 2005;201:366–74.
Iannelli A, Amato D, Addeo P, et al. Laparoscopic conversion of vertical banded gastroplasty (Mason MacLean) into Roux-en-Y Gastric Bypass. Obes Surg 2008;18:43–6.
Mognol P, Chosidow D, Marmuse JP. Roux-en-Y gastric bypass after failed vertical banded gastroplasty. Obes Surg 2007;17:1431–4.
Gumbs AA, Pomp A, Gagner M. Revisional bariatric surgery for inadequate weight loss. Obes Surg 2007;17:1137–45.
Iannelli A, Dainese R, Piche T, et al. Laparoscopic sleeve gastrectomy for morbid obesity. World J Gastroenterol 2008;14:821–7.
Ren CJ, Patterson E, Gagner M. Early results of laparoscopic biliopancreatic diversion with duodenal switch: a case series of 40 consecutive patients. Obes Surg 2000;10:514–23.
Gumbs AA, Gagner M, Dakin G, et al. Sleeve gastrectomy for morbid obesity. Obes Surg 2007;17:962–9.
Gagner M, Rogula T. Laparoscopic reoperative sleeve gastrectomy for poor weight loss after biliopancreatic diversion with duodenal switch. Obes Surg 2003;13:649–54.
Bernante P, Foletto M, Busetto L, et al. Feasibility of laparoscopic sleeve gastrectomy as a revision procedure for prior laparoscopic gastric banding. Obes Surg 2006;16:1327–30.
Feng JJ, Gagner M. Laparoscopic biliopancreatic diversion with duodenal switch. Semin Laparosc Surg 2002;9:125–9.
Kotidis EV, Koliakos GG, Baltzopoulos VG, et al. Serum ghrelin, leptin and adiponectin levels before and after weight loss: comparison of three methods of treatment—a prospective study. Obes Surg 2006;16:1425–32.
Cohen R, Uzzan B, Bihan H, et al. Ghrelin levels and sleeve gastrectomy in super–super-obesity. Obes Surg 2005;15:1501–2.
Lalor PF, Tucker ON, Szomstein S, et al. Complications after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis 2008;4:33–8.
Deitel M, Crosby RD, Gagner M. The First International Consensus Summit for Sleeve Gastrectomy (SG), New York City, October 25–27, 2007. Obes Surg 2008;18:487–96.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Elazary, R., Hazzan, D., Appelbaum, L. et al. Feasibility of Sleeve Gastrectomy as a Revision Operation for Failed Silastic Ring Vertical Gastroplasty. OBES SURG 19, 645–649 (2009). https://doi.org/10.1007/s11695-008-9714-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-008-9714-5