Abstract
Background
The BioEnterics Intragrastric Balloon (BIB®) together with restricted diet has been used for the treatment of obesity and morbid obesity.
Methods
A prospective study was conducted on 100 patients who had undergone the BIB procedure between February 2005 and February 2007.
Results
Mean age, mean weight, and mean BMI of the patients were 35.35 ± 9.25 years, 113.23 ± 24.76 kg (range 73–200 kg), and 39.28 ± 6.98 kg/m2 (range 30–69.2 kg/m2), respectively. Six months after the BIB procedure, mean weight and mean BMI were reduced to 100.46 ± 26.05 kg (range 58–178 kg) and 34.70 ± 11 kg/m2 (range 21.83–61.59 kg/m2), respectively. There was a statistically significant reduction in weight and BMI at 6 months after the BIB procedure (p < 0.01). Excess weight loss (EWL) at 6 months ranged between 0 and 28 kg, with a mean value of 12.68 ± 7.70 kg. The subjects had 0 to 99.2% %EWL (mean 28.63 ± 19.29). Reduction in BMI at 6 months ranged between 0 and 12.3 kg/m2, with a mean value of 4.51 ± 2.85 kg/m2, and percent excess body mass index loss (%EBMIL) was 38.20 ± 28.78% (range 0–158%). At 6 months, there was a significant reduction in body weight and BMI (p < 0.01) in both groups. The reduction in BMI of the morbidly obese group was significantly greater than that of the obese group (p = 0.035), and both the %EWL and %EBMIL of the morbidly obese patients were significantly lower than those of the obese patients at 6 months (p = 0.001).
Conclusions
BIB application is a reasonable weight loss method with few complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is a serious health problem at all ages, which influences the morbidity, mortality, and quality of life of the affected individuals. The etiology of obesity is multifactorial, which makes the success in treatment more difficult. The goal of the treatment is not only to achieve excess weight loss (EWL) but to maintain it; therefore, it is usually difficult for the patients to get significant permanent weight loss [1]. Whether managed by diets, exercise and medication, or endoscopic and surgical interventions, the treatment of obesity aims to reduce weight and the risks of comorbidities [2]. Temporary intragastric balloon application together with a diet program has gained popularity [3, 4]. This clinical prospective study has been designed to evaluate the effects of intragastric balloon application on obese patients.
Materials and Methods
Between February 2005 and February 2007, 100 patients had undergone the BioEnterics Intragastric Balloon (BIB—Inamed, Allergan, Irvine, CA, USA) procedure. Sixty-two female (62%) and 38 (38%) male patients aged between 15 and 62 years old were enrolled in the study. All subjects were given deep sedation as described by Coskun and Aksakal [5] in the operating room and monitored (noninvasive arterial blood pressure, SpO2, 3-lead ECG). A flexible endoscope (Olympus, CLV-U40) was used for both balloon application and removal procedures. An initial upper GI endoscopy and the BIB application were done by the same surgeon. After insertion, the balloon was filled with 550 mL of saline stained with 10 mL methylene blue dye. The drugs used during and after the BIB procedure were applied in the way that Coskun and Aksakal [5] described.
The balloon removal procedures were done after an 8-h starvation, using the BIB removal kit (Kobi Medizintechnik GmBH, Lehrte, Germany). The patients were discharged after 2 h of observation. Balloon exclusion criteria are given in Table 1. Percent excess body mass index loss (%EBMIL) was calculated according to Deitel et al. formulation in all patients [6].
Statistical Analysis
The Statistical Package for Social Sciences for Windows 10.0 program was used for the analysis. Descriptive data are given as means ± standard deviation. Student t test and Mann Whitney U test (for non-Gaussian data) were used to compare the groups. Paired simple t test was used to compare the data in each group and the Chi-square test was used for evaluation of the quality data. A p value less than 0.05 was considered significant.
Results
The mean age of the patients was 35.35 ± 9.25 years, with a mean weight of 113.23 ± 24.76 kg (range 73–200 kg) and mean BMI 39.28 ± 6.98 kg/m2 (range 30–69.2 kg/m2). At 6 months, the mean weight and mean BMI were reduced to 100.46 ± 26.05 kg (range 58–178 kg) and 34.70 ± 7.11 kg/m2 (range 21.83–61.59 kg/m2), respectively. There was statistically significant reduction in weight and BMI at 6 months (p = 0.001, p = 0.01).
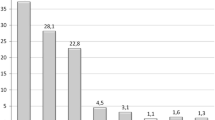
EWL at 6 months ranged between 0 and 28 kg, with a mean of 12.68 ± 7.70 kg. The subjects had lost 0% to 99.2% of their excess body weight (mean 28.63 ± 19.29). BMI reduction at 6 months ranged between 0 and 12.3 kg/m2, with a mean of 4.51 ± 2.85 kg/m2, and %EBMIL was 38.20 ± 28.78% (range 0–158%). The reduction in BMI of the morbidly obese patients was significantly more than that of the obese group at 6 months (p = 0.035). The %EWL and %EBMIL of the morbidly obese group were significantly lower than those of the obese group at 6 months (p = 0.012, p = 0.001). Complications due to the procedures are given in Table 2.
Discussion
The idea of using an intragastric device was first developed by Neiben in 1982, when he observed the long period of good tolerance of the gastric bezoars that resulted in significant weight loss [7]. The development of the BIB filled with saline has drawn attention to this method again. The recent studies have shown that the BIB is more reliable with better results than the previous balloons. BIB application is a repeatable and reversible restrictive method compared to other bariatric interventions [8, 9]. BIB application has an important role in reducing mortality and morbidity of morbidly obese patients when applied before bariatric or other operations [10, 11].
Genco et al. [11] placed BIBs in 2,515 patients (mean BMI 44.4 kg/m2) and reported a mean %EWL of 33.9 at 6 months. In our series, mean EWL at 6 months was 28.63 ± 19.29%. On their follow-up at 6 months, obese patients and morbidly obese patients had mean weight losses of 9 and 13 kg, respectively. Herve et al. [12] studied 100 patients and reported that the group with a mean BMI of 30–34.9 kg/m2 had a mean loss of 11.7 kg at 6 months (mean %EWL 41.2), patients weighing 35–39.9 kg/m2 lost a mean of 16.6 kg (mean %EWL 42.2), and the group with a mean BMI >40 kg/m2 lost 17.2 kg (mean %EWL 25.9). In our series of 100 patients who underwent BIB application (mean BMI 39.28 ± 6.98 kg/m2), the mean weight loss and mean %EWL of the obese group (BMI 30–39.9 kg/m2) were as follows: 11.43 ± 7.15 kg and 31.95 ± 21.27%, respectively. In the morbidly obese group (BMI ≥ 40 kg/m2), results of the same variables were as follows: 14.94 ± 8.24 kg and 22.60 ± 13.36%, respectively.
The BIB system usually causes nausea and vomiting in the first week of application. Authors have reported that 77–78% of the patients had nausea and vomiting during the first week of balloon application [12, 13]. In our study, nausea (82%), vomiting (65%), and crampy abdominal pain (75%) were observed in the first 72 h, which diminished progressively by the end of the first week.
Ten of our 100 patients developed balloon intolerance in their first week (2–7 days) with no signs of dehydration. We had suggested hospitalization to these patients; however, all 10 patients demanded balloon removal, which leads us to comment on this situation as psychological intolerance of the BIB. We believe that detailed informed consent prior to the intervention is necessary in order to avoid psychological intolerance. As a matter of fact, after the first few cases of the 100 interventions, we observed much less psychological intolerance, probably due to our improved patient management. Early BIB removal due to patient intolerance has been found in 4.3% to 13.6% in the literature [4, 8, 12, 13].
BIB is designed to stay in the stomach for 6 months. Longer periods may lead to sudden rupture and intestinal obstruction and its complications [14]. Gastric perforation is very rare, but it necessitates urgent intervention. Al-Momen and El-Mogy [13] reported gastric perforation in one patient (2.2%), and Genco et al. [11] reported five gastric perforations (0.19%), of which three underwent laparoscopic surgery, but the other two died. Doldi et al. [4] reported a silent balloon rupture, which passed out with the stools, whereas Roman et al. [8] reported a patient having partial intestinal obstruction due to balloon rupture and displacement and a second patient with intestinal obstruction at 14 months. Genco et al. [11] reported gastric outlet obstruction in 19 patients (0.76%) in the first week of BIB application and balloon rupture in nine cases (0.36%).
One of our cases (1.1%) had balloon rupture and spontaneous discharge through the gastrointestinal tract at 5 months. The patient had suffered mild nausea and abdominal pain but did not notice color change of the urine and was relieved after passage of the balloon. At BIB removal time, two patients had developed esophagitis (2.2%), but no gastric ulceration or perforation was observed. BIB application is a reasonable weight loss method with few complications. Besides this, in superobese patients, BIB application provides satisfactory weight loss prior to bariatric surgery as a means of preoperative preparation.
References
Gostout CJ, Rajan E. Endoscopic treatments for obesity: past, present and future. Gastroenterol Clin North Am. 2005;34:143–50.
Melissas J, Mouzas J, Filis D, et al. The intragastric balloon—smoothing the path to bariatric surgery. Obes Surg. 2006;16:897–902.
Wahlen CH, Bastens B, Herve J, et al. The Bioenterics intragastric balloon (BIB): how to use it. Obes Surg. 2001;11:524–7.
Doldi SB, Micheletto G, Perrini MN, et al. Treatment of morbid obesity with intragastric balloon in association with diet. Obes Surg. 2002;12:583–7.
Coskun H, Aksakal C. Experience with sedation technique for intragastric balloon placement and removal. Obes Surg. 2007;17:995–6.
Deitel M, Gawdat K, Melissas J. Reporting weight loss. Obes Surg. 2007;17:565–8.
Neiben OG, Harboe H. Intragastric balloon as an artificial bezoar for treatment of obesity. Lancet. 1982;1:198–9.
Roman S, Napoleon B, Mion F, et al. Intragastric balloon for “non-morbid” obesity: a retrospective evaluation of tolerance and efficacy. Obes Surg. 2004;14:539–44.
Genco A, Cipriano M, Bacci V, et al. Bioenterics intragastric balloon (BIB): a short term, double-blind, randomized, controlled, crossover study on wight reduction in morbidly obese patients. Int J Obes. 2006;30:129–33.
Busetto L, Sagato G, De Luca M, et al. Preoperative weight loss by intragastric balloon in super-obese patients treated with laparoscopic gastric banding: a case-control study. Obes Surg. 2004;14:671–6.
Genco A, Bruni T, Doldi SB, et al. Bioentrics intragastric balloon: the Italian experience with 2515 patients. Obes Surg. 2005;15:1161–4.
Herve J, Wahlen H, Schaeken A, et al. What becomes of patients one year after the intragastric balloon has been removed? Obes Surg. 2005;15:864–70.
Al-Momen A, El-Mogy I. Intragastric balloon for obesity: a retrospective evalution of tolerance and efficacy. Obes Surg. 2005;15:101–5.
Mathus-Vliegen EM, Tytgat GN, Veldhuyzen-Offermans EA. Intragastric balloon in the treatment of super-morbid obesity. Double-blind, sham-controlled, crossover evaluation of 500-milliliter balloon. Gastroenterology. 1990;99:362–9.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Coskun, H., Bostanci, O., Dilege, E. et al. BioEnterics Intragastric Balloon: Clinical Outcomes of the First 100 Patients—A Turkish Experience. OBES SURG 18, 1154–1156 (2008). https://doi.org/10.1007/s11695-008-9565-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-008-9565-0