Abstract
Background
An increasing importance has been placed on a bariatric program’s readmission rates. Despite the importance of such data, there have been few studies that document 1-year readmission rates. There have been even fewer studies that delineate the causes of readmission. The objective of this study is to delineate the rates and causes of readmissions within 1 year of bariatric operations performed in a high-volume center.
Methods
Records for all patients undergoing bariatric operations during a 31-month period were harvested from the hospital electronic medical database. Readmissions for these patients were then identified within the hospital database for the year following the index operation. The electronic medical records of all readmitted patients were reviewed.
Results
The overall 1-year readmission rate for 1,939 consecutive bariatric operations was 18.8%. The laparoscopic adjustable gastric band (LAGB) had the lowest readmission rate of 12.69%. Next was the vertical banded gastroplasty-Roux-en-Y gastric bypass (VBG-RYGB) with a rate of 15.4%. The laparoscopic Roux-en-Y gastric bypass (LRYGB) had the highest readmission rate of 24.2%. Leading causes of readmission were abdominal pain with normal radiographic studies and elective operations. Independent factors predicting readmission were found to be LOS > 3 days (odds ratio 1.69 p = 0.004) and having a LRYGB (odds ratio of 1.49 p = 0.003). The previously reported reoperation rate for bowel obstruction of 9.7% had decreased to 3.7% due to changes in operative technique.
Conclusion
Rates of readmissions for patients undergoing bariatric surgery center at our high-volume center decreased over time and are comparable to other major abdominal operations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery has been shown to lower health care costs over the 5-year period following surgery [1]. Bariatric surgery also decreases premature mortality in morbidly obese patients compared to morbidly obese subjects who do not undergo weight loss surgery [2]. Nonetheless, bariatric surgery may be a cost looser for insurance providers [3]. This dichotomy has stimulated intense interest in bariatric surgery outcomes that impact global patient costs and, as a result, focused attention on readmission rates following weight loss operations.
Patients sustain high readmission rates following all types of gastrointestinal operations. Kiran et al. [4] of the Cleveland Clinic, for example, reported a 10.1% readmission rate within 30 days following a variety of intestinal operations. Similarly, Emick et al. [5] of Johns Hopkins Medical Institution reported a 26% readmission rate following pancreaticoduodenectomy. Recently, several papers have reported 30-day readmission rates following bariatric operations for morbidity obesity and found 30-day readmission rates ranging form 0.6 to 11.3% [6, 7]. Few reports, however, have documented 1-year readmission rates following weight loss surgery.
The purpose of this study was to determine the rates and causes of readmissions within 1 year of index bariatric operations at a high-volume American College of Surgeons-accredited 1A Bariatric Surgery Program. We hypothesized that 1-year readmission rates following open vertical banded gastroplasty-Roux-en-Y gastric bypass (VBG-RYGB) and laparoscopic Roux-en-Y gastric bypass (LRYGB) would exceed those following laparoscopic adjustable gastric banding (LAGB). Indeed, we found that patients following LAGB required a much lower rate of readmissions within 1 year of surgery than either VBG-RYGB or LRYGB but were surprised to find that rates of 1-year readmission following LRYGB were significantly greater than after open VBG-RYGB.
Methods
Study Design
This was a retrospective study of the bariatric surgery database from 6/1/2003 and 12/31/05. The subset of patients who were readmitted to the hospital within 365 days of the date of their index bariatric operation was studied.
Setting
Data were taken from the Bariatric Database at Hackensack University Medical Center (HUMC), a 781-bed teaching and research hospital affiliated with The University of Medicine and Dentistry of New Jersey—New Jersey Medical School. The Bariatric Program at Hackensack University Medical Center is one of the busiest in the country by volume, and it is accredited by the American College of Surgeons as a IA Bariatric Surgery Program.
Statistics
Data are presented as median and ranges. Groups were compared by Kruskal–Wallis one-way analysis of variance (ANOVA). Stepwise and univariate logistic regression analysis was performed only on patient records with complete data sets. All statistical operations were accomplished using Unistat 5.5 Statistical Package for Windows (Unistat, London, UK).
Operations
Three bariatric operations are offered by the surgeons at Hackensack University Medical Center: an open VBG-RYGB, LRYGB, and LAGB. The VBG-RYGB is performed via a midline laparotomy. A small tubular lesser curve based gastric pouch is created and reinforced with a polypropylene band. A two-layer hand-sewn anastomosis is created to a 100 or 150 cm Roux limb. This is done in a retro-gastric and retro-colic manner [8, 9]. The LAGB is placed using the pars flaccida technique. The LRYBP creates a small gastric pouch that is stapled to a 100 cm roux limb using a 25-mm EEA stapler in a retro-colic and retro-gastric manner [10, 11].
Patient Definition
After obtaining permission from the institutional review board, all patients undergoing bariatric operations at HUMC during the 6/2/2003 and 12/31/2005 were entered in a retrospective hospital database based on the corrected operative log. Readmissions were defined as any admission to the HUMC for any reason. Emergency room visits not resulting in hospital admission were not included.
Variables
Patient demographics as well as anthropometrics were included when available. Insurance data as well as documented comorbidities were also included. Each readmission was chart reviewed to determine the cause of readmission.
Results
Analysis of All Patients
A total of 1,939 patients underwent bariatric operations at HUMC from 6/1/2003 and 12/31/05. The breakdown of operations was as follows: VBG-RYBG, 591 (30.4%); LRYBG, 883 (45.5%); LAGB, 465 (24.0%). There were 27 documented revisions and 1,912 primary operations. The mean initial length of stay (LOS) for all patients was 3 days (0–46). The VBG-RYGB median and mean length of stay was 3 days (0–39). The median and mean LOS for the LRYGB was also 3 days (0–46). The median and mean LOS for the LAGB was 1 day (0–8). The LOS was statistically different for each of the three operations.
Patient Characteristics
Information on age and gender was available on all 1,939 patients. Of the entire cohort, there were 1,457 (75.1%) women and 482 (24.9%) men. There were no differences between the genders of each of the three operations. The average age for all patients was 42 years (13–79). Information on preoperative height and weight was available for 1,674 patients. The mean height for all patients was 168 cm (142–201). The mean weight was 133 kg (57–290). The mean BMI of all patients was 47 kg/m2 (18–83). There was no significant difference in BMI for each of the three bariatric operations.
Patients Not Readmitted
There were 1,674 patients who did not require readmission to HUMC within 1 year after their index bariatric operation. Of those not readmitted, the breakdown of operations was as follows: VBG-RYGB, 516 (30.1%); LRYGB, 739 (44.2%); LAGB, 419 (25.0%). There were 1,652 patients who had primary bariatric operations, and 22 had revisional surgery. The LOS for those not readmitted was 2.5 days (0–39), VBG-RYBG 3 days (0–39), LRYGB was 3 days (0–19), and LAGB 1 day (0–8) LOS was statistically significant for each group.
Of this cohort, there were 1,254 women (74.9%) and 420 men (25.1%). The mean age was 42 years (13–79). The median height was 168 cm (142–201). The mean weight was 133 kg (59–290) and the mean body mass index (BMI) was 47 kg/m2 (21–83).
The data on race were available for 1,663 patients. The break down was as follows: White 79.2%, African American 11.4%, other 6.2%, Asian 2.7%. This database did not differentiate Hispanic from non-Hispanic. American Society of Anesthesiologists (ASA) classification was available for 1,654 patients. The ASA classification was as follows: ASA 1, 11.4%; ASA 2, 35.9%; ASA 3, 52.1; ASA 4, 0.7%.
Insurance data were available on 1,663 of the patients not readmitted. HMOs accounted for 38.2%, Private insurance paid for 53.1%. Medicare and Medicaid paid for 6.5% of patients. 4.5% were self-paid and 1% were charity care.
Data on comorbidities were available for 1,663 patients. Of those patients not readmitted, 31.8% had no comorbidities, 27.2% listed one comorbidity, 22.4% had two comorbidities. Of the patients, 12.2% had three comorbidities and 5.9% listed four or more comorbidities. The most frequent comorbidities listed were as follows: hypertension 42.5%, type II diabetes 22.9%, sleep apnea 22.1%, asthma 18.9%, hypercholesterolemia 16.0% (Table 1).
Readmissions
There were 265 patients who required 364 readmissions within 1 year after their index bariatric operation (Fig. 1). The percentage of patients readmitted 1 year after bariatric surgery at HUMC was 16.7%. The overall readmission rate for all patients was 18.8% (total number of readmissions/number of index operations). The rates of readmission by operation were as follows: VBG-RYBG, 15.4%; LRYGB, 24.2%; and LAGB, 12.7%. Of the 27 documented revisions, there were 5 readmissions with a rate of 18.5%. The mean initial LOS for the 265 readmitted patients was 3 days (0–46). This was significantly longer than the LOS of 2.5 for those not readmitted. The mean length of stay at readmission was 3 days (0–34). By operation, it was VBG-RYBG, 4 days (0–34); LRYGB, 3.3 days (0–26); and LAGB, 3.1 days (0–22). There was no statistical difference in LOS at readmission. The mean number of days from operation to readmission for all patients was 127 (0–365). The breakdown by operation was as follows: VBG–RYBG: 112 (0–362) LRYGB: 129(0–365) and LAGB 142 (0–355). These differences were not statistically significant.
Of the cohort that was readmitted, there were 203 women (76.6%) and 62 men (23.4%). Demographic information was available for all 265 patients. The median of those readmitted was 42 years (16–78). Height and weight was available for 234 of the 265 readmitted patients. The mean BMI of the readmitted patients was 47 kg/m2(18–82). There was no statistic difference between age, weight, or BMI of those admitted and those not readmitted for each of the three operations.
Data were available on the race make up of 262 of the readmitted patients. The break down was as follows: White 76.0%, African American 12.2%, Other 7.6%, and Asian 3.4%. This database did not differentiate Hispanic from non-Hispanic. ASA data were also available for 262 patients. 6.9% were classified as ASA 1. 37.8% were classified as ASA 2. 54.2% were ASA 3, and 1.2% were ASA 4.
Insurance data were available on 262 readmitted patients. There were 49.6% privately insured. 38.2% belonged to a HMO. 6.5% were insured by either Medicare or Medicaid. There were 5.3% self-pay patients and 0.4% were charity care.
Data on medical comorbidities were available on 262 readmitted patients. The numbers of listed comorbidities were as follows: zero 28.2%, one 27.7% two 22.1%, three 13.3% four or more 9.5%. The most frequent comorbidities listed were hypertension (45.8%), asthma (22.9%), and type II diabetes (22.1%; Table 1).
Increased Odds for Readmission
Stepwise and multivariate logistic regression analysis identified three factors that impacted readmission rates (Table 2). An initial length of stay of greater than 5 days had an odds ratio for readmission of 2.12 (p < 0.005). Having a laparoscopic Roux-en-Y gastric bypass had an odds ratio of 1.50 (p < 0.002). Listing asthma as a comorbid condition had an odds ratio of 1.55 (p < 0.005).
Breakdown by 6-Month Periods
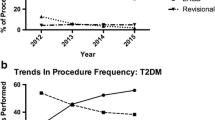
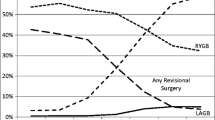
Operations were stratified by type of operation and by 6-month periods from June 2003 through December 2005 (Table 3). The first period includes seven months: June 2003 through December 2003. The total number of operations was similar for each time period. The number of VBG-RYGB declined from 206 to 92 in these four time periods. The number of LRYGB remained about the same. The number of LAGB increased from 91 to 161.
The number of patients from each time period that required readmission within 1 year of index bariatric operation declined during these four time periods (Table 4). A total of 94 patients required readmission in the first time period, and this dropped to 43 in the fourth time period. The number of patients requiring readmission within 1 year of the index bariatric operation also dropped for patients following VBG-RYGB, LRYGB, and LAGB.
The rates for patients requiring at least one readmission within a year of the index bariatric operations dropped overall from 17.8% in the first time period to 9.1% in the fourth time period (Table 5). LRYGB dropped from a 23.3% in the first time period to 11.4% in the fourth time period. LAGB increased in the second time period to 19.4% from 11.0% in the first time period but then dropped to 5.6% in the fourth time period. The rate of readmission for VBG-RYGB was similar for each of the four time periods, although there was a trend towards lower rates with time.
Causes of Readmission
The leading cause of readmission was abdominal pain with normal radiographic studies (Table 6). This accounted for 43/364 (11.8%) readmissions. 74.4% of these readmissions were after LRYGB. The next largest category of readmission was for elective surgery not related to the bariatric operation. This accounted for 39 readmissions or 10.7% of the cohort. The next two most frequent causes were nausea and vomiting without radiographic or endoscopic abnormalities and cholecystectomy. These two groups were responsible for 37 (10.2%) readmissions each. Miscellaneous causes accounted for 30 (8.2%) readmissions. There were 23 (6.3%) admissions for strictures requiring endoscopic dilatation. GI complaints not related to the bariatric operation such as diarrhea or constipation accounted for 23 admissions. There were 20 patients requiring operation for adhesive small bowel obstructions (5.5%). There were 18 patients requiring operations for internal hernias during this time period (4.9%). There were significantly more patients 17/18 (94%) with internal hernia who had LRYGB than VBG-RYGB. Eighteen patients were also readmitted with renal calculi and its sequelae (4.9%). There were 15 admissions (4.1%) for pneumonia/atelectasis/shortness of breath.
Readmissions Related to Bariatric Operation
Of the 364 readmission, 245 were deemed to be related to the initial bariatric operation. The rate of related readmissions was 12.6% (245/1939). Included in this number were all surgical complications, diarrhea within 30 days of surgery, nausea and vomiting with normal radiographic/endoscopic studies with in 100 days of the surgery. There were 119 readmission deemed not related to the bariatric operation. This included causes such as elective plastics and orthopedic surgery, medical admissions, and shortness of breath after 90 days of the operation. The rate of readmission for nonrelated cause was 6% (119/1,939).
Cholecystectomy
Since one group of surgeons at HUMC routinely preformed cholecystectomy for the presence of gallstones and another did not, the data were analyzed after the removal of all readmissions for cholecystectomy. Once this was done, the VBG-RYGB had a readmission rate of 14.1% (84/584), The LRYGB had a readmission rate of 21.9% (188/857), and the LAGB had a readmission rate of 11.9% (55/461). Based on these data, the routine cholecystectomy for gallstones at the time of bariatric operation reduced the rate of readmission for cholecystectomy from 2.9 to 1.2%.
Readmissions for Internal Hernias and Adhesive Obstructions
Numbers and rates of readmission for internal hernias and adhesive obstructions stratified by 6 month periods are listed in Table 7. Rates of readmissions for internal hernias during the 6 month periods dropped from 1.14 to 0.21% with an average of 0.92% for the entire study period. Rates of readmission for adhesive obstructions ranged from 0.42 to 1.96% with an average of 1.03%. Overall there was no significant difference in the rates of obstruction from internal hernias and adhesive obstructions.
Discussion
The purpose of this study was to compare and contrast the readmission rates at 1 year for the three bariatric operations offered at HUMC: LAGB, VBG-RYGB, and LRYGB. To our knowledge, is the largest series of patients followed for 1 year using a hospital’s electronic medical record and not multi-institutional administrative data. HUMC was uniquely qualified to perform this because of the high volume of each of the three operations. A total of 1,939 consecutive index bariatric operations were identified in a 31-month period. There were 364 total readmissions within the first year, a rate of 18.8%. There were 265 patients readmitted within the first year with a patient readmission rate of 16.7%. LAGB had the lowest rate of readmission at 12.7% (59/465). Next was VBG-RYBG with a readmission rate of 15.4% (91/591). The highest readmission rate was LRYBG with 24.3% (214/883). Factors that increased risk of readmission were undergoing a LRYGB, listing asthma as a comorbid condition, and staying in the hospital more than 5 days. The increased risk after a LRYGB was only present for the first months after surgery.
The most frequent causes for readmission were abdominal pain and elective operations. The leading causes for readmission for VBG-RYGB were vomiting, miscellaneous, and elective operations. For the LAGB, the leading causes for readmission were elective operations, vomiting, and band revisions. The leading causes for readmission for LRYGB were abdominal pain, cholecystectomy, and adhesive small bowel obstruction. Rates of readmission for internal hernias dropped over the period of the study and overall closely approximately those observed for adhesive obstructions.
There have been very few studies documenting the 1-year readmission rate for gastrointestinal operations. Most reports have detailed 30-day readmission rates. Goodney and colleagues examined the national Medicare database for 30-day readmission rates for high-risk gastrointestinal operations [12]. These included the following: colectomy 11.1%, gastrectomy 16.6%, esophagectomy 18.4%, and pancreatic resection 18.7%. In our study, 131 of the 364 readmissions following bariatric operations occurred within the first 30 days after surgery for a rate of 6.8%. This is similar to our previously reported 6.5% 30-day readmission rate for a larger cohort of 2,823 bariatric patients [13]. Similarly, Nguyen et al. [14] reported a 6.6% 30-day readmission rate following 40 bariatric operations at each of 29 university hospitals, and Weller et al. [15] reported a 7.6% 30-day readmission rate after 7,868 bariatric operations recorded in the New York State inpatient discharge database for January through November 2003. In the largest study to date, Nguyen et al. [16] calculated a 0.6% 30-day readmission rate among 24,165 Roux-en-Y gastric bypasses performed between 1999 and 2002 that were recorded in the University Health System Consortium Clinical Data. Most of these studies relied on either administrative or insurance data.
One-year readmission rates following bariatric operations have been infrequently reported. Zingmond et al. published a 1-year readmission rate of 19.3% after gastric bypass by mining a California statewide patient discharge database that included 60,077 patients who had undergone gastric bypass between 1995 and 2004 [17]. In this study, they also reported the admission rates for these patients during the year preceding their bariatric operation: a rate of 7.9%. They attributed the dramatic increase in admissions following surgery to procedure related complications. The most common admitting diagnoses prior to surgery were elective operations and obesity related complications. The most common diagnoses after bariatric surgery were GI tract procedure or gastric bypass-related complication and also elective surgery. The 1-year readmission rate of 19.3% was very close to our rate of 18.8%. Moreover, the reasons for readmission were very similar.
All the previous authors used administrative data to support their conclusions. Many publications have documented the inaccuracies of administrative data compared to hospital based records [18]. Previous reports had estimated the accuracy of administrative data at around 57% for the correct primary diagnosis and 27% correct for secondary diagnostic data [19]. This discrepancy between the administrative diagnosis and the actual diagnosis led us to review in detail the medical records of all of the readmitted patients. In out study, we found that the administrative data from the hospital financial records in either the form of admitting or discharge ICD-9 codes accurate in only 89% (325/365) of readmissions. These results suggest that one must interpret with cautions data from multi-institutional administrative databases.
As we had hypothesized, patients following LAGB (12.7%) required the lowest readmission rate. In contrast, we were surprised by the increased rate of readmissions following LRYGB (24.2%) as compared to VBG-RYGB (15.4%). VBG-RYGB posted the highest rate of admissions classified as vomiting. There was no increased rate of readmissions due to either wound complications or hernias for the open VBG-RYGB as one might have predicted. Much of the excess readmissions following LRYGB resulted from abdominal pain, elective cholecystectomy, and intestinal obstruction. The difference in cholecystectomy readmissions is largely due to the preferences of the surgeons. As a group, the laparoscopic surgeons rarely remove the gall bladder at the time of gastric bypass while the open gastric bypass surgeons have a much more liberal policy towards removing the gall bladder at time of gastric bypass.
The bowel obstruction data were surprising as well. We previously reported a rate of reoperation for bowel obstruction after LRYGB of 9.7% with a minimum of 18-month follow-up [20]. The current data show a significant reduction in the overall reoperation rate for bowel obstruction to 3.7% (35/883). Table 7 illuminates our learning curve in regards to preventing internal hernias following LRYGB with rates for consecutive 6-month groups dropping from 1.14% and 1.47% to 0.87% and then 0.21%. There were similar numbers of adhesive obstructions (18) as internal hernias (17) in the LRYGB group. We feel that this decrease is due to the change in our operative technique. Starting in July 2004, all of the laparoscopic surgeons began routinely closing all of the mesenteric defects. Although prior publications have listed that the average time to obstruction (511 days postoperation) is beyond the follow-up of this paper, we feel that the trend is significant [20]. Despite the reduction in rate of reoperation for bowel obstruction, it does not yet approach the low overall reoperation rate for bowel obstruction following open VBG-RYGB (0.5%).
Limitations
This is a paper examining the readmission rate of a single institution with a large geographic draw. It is possible that a significant portion of readmissions are missed because the patients either were taken to the nearest emergency room or chose another hospital.
Conclusions
Hospital readmissions following bariatric surgery was 18.8%. This was comparable to other complex abdominal operations. The LAGB had the lowest readmission rate (12.69%), followed by the VBG-RYGB (15.4%) and then the LRYGB (24.2%). This study showed a decreasing readmission rate over time. Factors that increased the risk of readmission were as follows: undergoing a LRYGB, listing asthma as a comorbidity, and staying in the hospital more than 5 days after operation.
References
Christou NV, Sampalis JS, Liberman M, et al. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg. 2004;240:416–23.
Flum DR, Dellinger EP. Impact of gastric bypass operation on survival: population-based analysis. J Am Coll Surg. 2004;199:543–51.
Craig BM, Tseng DS. Cost-effectiveness of gastric bypass for severe obesity. Am J Med. 2002;113:491–8.
Kiran RP, Delaney CP, Senagore AJ, et al. Outcomes and prediction of hospital readmission after intestinal surgery. J Am Coll Surg. 2004;198;877–83.
Emick DM, Riall TS, Cameron JL, et al. Hospital readmission after pancreaticoduodenectomy. J Gastrointest Surg. 2006;10:1242–52.
Nguyen NT, Paya M, Stevens CM, et al. The relationship between hospital volume and outcome in bariatric surgery at academic medical centers. Am Surg. 2004;240:586–94.
Weller WE, Rosati C, Hannan EL. Relationship between surgeon and hospital volume and readmission after bariatric surgery. J Am Coll Surg. 2007;204:383–91.
Capella JF, Capella RF. The weight reduction operation of choice: vertical banded gastroplasty or gastric bypass? Am J Surg. 1996;171(1):74–9.
Capella JF, Capella RF. An assessment of vertical banded gastroplasty-Roux-en-Y gastric bypass for the treatment of morbid obesity. Am J Surg. 2002;183(2):117–23.
Oliak D, Ballantyne GH, Weber P, Davies RJ, Schmidt HJ. Laparoscopic Roux-en-Y gastric bypass: defining the learning curve. Surg Endosc. 2003;17(3):405–8.
Chau WY, Schmidt HJ, Kouli W, Davis D, Wasielewski A, Ballantyne GH. Patient characteristics impacting excess weight loss following laparoscopic adjustable gastric banding. Obes Res. 2005;15(3):346–50.
Goodney PP, Stukel TA, Lucas FL, Finlayson EV, Birkmeyer JD. Volume, length of stay, and readmission rates in high-risk surgery. Ann Surg. 2003;238:161–7.
Saunders JK, Ballantyne GH, Belsley S, et al. 30-day readmission rates at a high volume bariatric surgery center: laparoscopic adjustable gastric banding, laparoscopic gastric bypass, and vertical banded gastroplasty-Roux-en-Y gastric bypass. Obes Surg. 2007;17:1171–7.
Nguyen NT, Slver M, Robinson M, et al. Results of a national audit of bariatric surgery performed at academic centers: a 2004 university health system consortium benchmarking project. Arch Surg. 2006;141:445–50.
Weller WE, Rosati C, Hannan EL. Relationship between surgeon and hospital volume and readmission after bariatric operations. J Am Coll Surg. 2006;202:753–61.
Nguyen NT, Paya M, Stevens CM, Mavandadi S, Zainabadi K, Wilson SE. The relationship between hospital volume and outcome in bariatric surgery at academic medical centers. Ann Surg. 2004;240:586–94.
Zingmond DS, McGory ML, Ko CY. Hospitalization before and after gastric bypass surgery. JAMA. 2005;294:1918–24.
Benesch C, Witter DM Jr, Wilder AL, Duncan PW, Samsa GP, Matchar DB. Inaccuracy of the ICD-9-Cm in identifying diagnosis of ischemic cerebrovascular disease. Neurology. 1998;50:306.
Peabody JW, Luck J, Jain S, Bertenthal D, Glassman P. Assessing the accuracy of administrative data in health information systems. Med Care. 2004;41:1066–72.
Capella RF, Iannace VA, Capella JF. Bowel obstruction after open and laparoscopic gastric bypass surgery for morbid obesity. J Am Coll Surg. 2006;203:328–35.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Saunders, J., Ballantyne, G.H., Belsley, S. et al. One-year Readmission Rates at a High Volume Bariatric Surgery Center: Laparoscopic Adjustable Gastric Banding, Laparoscopic Gastric Bypass, and Vertical Banded Gastroplasty-Roux-en-Y Gastric Bypass. OBES SURG 18, 1233–1240 (2008). https://doi.org/10.1007/s11695-008-9517-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-008-9517-8