Abstract
Background
Nonalcoholic steatohepatitis (NASH) and gallbladder disease (GD) are members of metabolic syndrome in morbidly obesity. Insulin resistance is a risk factor for NASH and GD. The aim of the present study was to investigate the relationship between insulin resistance (HOMA-IR), liver fibrosis, NASH and GD in morbidly obese patients who presented with fatty liver during preoperative abdominal ultrasonography examination.
Methods
We studied 152 morbid obese patients with fatty liver disease including 54 with NASH, 11 with GD and two with concurrent NASH and GD that were undergoing laparoscopic bariatric surgery. Clinical data (gender, age, body mass index [BMI], and associated diseases), laboratory evaluation, and histopathology were obtained from the patient databases. We analyzed the relationship between clinical characteristics, histological parameters, HOMA-IR, and fibrosis stage associated with NASH and GD in morbid obese patients.
Results
Among the 152 patients with fatty liver disease, 93 were females and 59 were males. The mean age was 30.3 ± 8.9 years and the mean BMI was 44.9 ± 5.4 kg/m2. Fifty-four patients (54/152, 35.5%) were diagnosed as NASH and 11 patients (11/152, 7.2%) received concomitant laparoscopic cholecystectomy because of gallbladder disease (GD). Morbidly obese patients with fatty liver disease and GD were significantly older (P = 0.020), had higher serum levels of cholesterol (P = 0.020) and low-density lipoprotein (LDL)-cholesterol (P = 0.044), and had lower serum levels of total bilirubin (P = 0.044), C-peptide (P = 0.023), and insulin (P = 0.039) than the NASH group. Histopathology factors of hepatic steatosis (P = 0.012), ballooning degeneration (P = 0.001), lobular inflammation (P = 0.019), fibrosis (P = 0.026), and glycogenated nuclei (P = 0.028) were significantly different between NASH and GD groups. However, further multivariate analysis failed to demonstrate any independent clinicopathological factor. The prevalence of chronic hepatitis B and NASH was the same (18%) in all 11 GD patients. Besides, when we compared NASH patients (n = 54) with concurrent NASH-GD patients (n = 2), we found that waist (P = 0.016), waist/hip (P = 0.039), and HOMA-IR (P = 0.040) were independent associated factors. We further assessed the HOMA-IR distribution and the relationship between fibrosis stage in patients with NASH and GD. In the NASH group, HOMA-IR distribution progressively decreased when the severity of fibrosis was plotted as a function of insulin resistance.
Conclusion
The prevalence of NASH in gallbladder disease was 18% in morbid obese population. We concluded that age, serum cholesterol, and low-density lipoprotein cholesterol levels were risk factors associated with gallbladder disease and fatty liver disease. Insulin resistance was more common in concurrent NASH and gallbladder disease. The mechanism between insulin resistance, fibrosis stage, NASH, and gallbladder disease is unknown.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is a common health problem in both Western and Eastern countries. Nonalcoholic steatohepatitis (NASH), first named by Ludwig et al. [1], is part of a broad spectrum of nonalcoholic fatty liver disease ranging from hepatic steatosis, ballooning degeneration of hepatocytes, lobular inflammation to steatohepatitis, which shows progression to liver fibrosis [2–4]. The main risk factors associated with NASH include obesity, hyperlipidemia, type 2 diabetes mellitus, insulin resistance, and conditions associated with the metabolic syndrome [5–7].
Gallbladder disease (GD) is highly prevalent in obese population [8–10]. Association of GD to metabolic syndrome includes obesity, type II diabetes mellitus, dyslipidemia and insulin resistance [11–14]. A pathogenic link between low-grade systemic chronic inflammation, obesity, insulin resistance, NASH, and GD is interesting. As NASH and GD share many similar risk factors, it will be expected that insulin resistance may be an important factor in both NASH [15, 16] and GD [17]. However, a few controversial studies have been reported to identify the possible association of NASH and GD [18, 19]. The prevalence and multiple risk factor analysis associated with GD observed in NASH patients in obese population have rarely been investigated. A previous study in Asian population [20] suggested that chronic liver disease, particularly liver cirrhosis, was a risk factor for cholecystolithiasis. Fibrosis is thought to be a disease resulting from NASH. The relationship of liver fibrosis stage regarding to the factors associated with the presence of NASH and GD in obese population is still unknown. Furthermore, it is unclear whether NASH patients who also have concurrent GD have any specific metabolic risk factors.
The purpose of this study was to identify the prevalence and risk factors associated with GD and NASH in morbid obesity presented with fatty liver during preoperative abdominal ultrasonography examination. Assessment to the effect of insulin resistance (HOMA-IR) on fibrosis stage between NASH and GD groups in morbidly obese patients was also analyzed.
Materials and Methods
Study Design, Patient Selection, and Serological Testing
The retrospective study was performed with the approval of the ethic committee. From 2003 to 2005, a total of 152 morbid obese patients with fatty liver diagnosed during preoperative abdominal ultrasonography examination undergoing laparoscopic weight reduction surgery were consecutively enrolled. Part of the database was published previously [21]. All patients gave written informed consent for participation. Patients with a history of obesity of >5 years' duration, BMI >40 kg/m2 with comorbidities, documented weight-loss attempts in the past, and good motivation for surgery were submitted in our study. The preoperative assessment included a clinical and familial assessment, a psychiatric assessment, anthropometric measurements, and laboratory tests. An assessment of alcohol consumption was obtained at the surgical consultation. Laboratory tests included liver function tests, fasting lipid profiles, fasting glucose profile, fasting insulin, C-peptide, HbA1c, adiponectin, HOMA-IR = (fasting insulin [μIU/mL] × fasting glucose [mmol/L] / 22.5), hepatitis B and C serology (HBsAg, HBV DNA, and antibody to HCV). In this study, we decided to use a HOMA-IR of more than 2.0 as the criterion to represent insulin resistance [22].
Laparoscopic wedge-resected liver biopsies were taken as a routine part of the operative procedure in all 152 obese patients. Patients with intraoperative findings of gallstones were undergone concomitant cholecystectomy.
Pathological Assessment
All liver biopsies were fixed and examined using hematoxylin–eosin and the Periodic-acid Schiff with diastase stain for necroinflammatory grading. Masson’s trichome and silver reticulin stains were reviewed for fibrosis and architectural changes. Each specimen was blindly interpreted with one pathologist (P-L L). Steatosis was graded as follow: (0) <5% of the hepatocytes with steatosis, (1) 5–33% of the hepatocytes with steatosis, (2) >33–66% of the hepatocytes with steatosis, (3) >66% of the hepatocytes with steatosis. Lobular inflammation was scored as: (0) no inflammation, (1) <2 foci per 200× field, (2) 2–4 foci per 200× field and (3) >4 foci per 200× field. Ballooning degeneration was scored as: (0) none, (1) few balloon cells, and (2) many/prominent balloon cells. Portal inflammation was analyzed as: (0) none to minimal, (1) moderate, and (2) severe. Liver fibrosis stage was assessed on a five-stage scale: (0) no fibrosis, (1) perisinusoidal fibrosis without portal or periportal fibrosis, (2) perisinusoidal fibrosis with portal or periportal fibrosis, (3) perisinusoidal fibrosis with portal or periportal fibrosis with focal or extensive bridging fibrosis, and (4) cirrhosis. Presence of Mallory bodies, PAS-D Kupffer cells, acidophil bodies, and glycogenated nuclei was recorded. NAFLD Activity Score (NAS) is defined as the unweighted sum of the scores for steatosis (0–3), lobular inflammation (0–3), and ballooning (0–2); thus giving the score ranging from 0 to 8. Fibrosis is not included as a component of the activity score. NAS of ?5 correlated with a diagnosis of NASH, and biopsies with scores of less than 3 were diagnosed as “not NASH” [23, 24].
The gallbladder specimens were examined and histologic parameters graded using hematoxylin–eosin stain. Histological graded parameters included; (a) degree of acute inflammation, (b) chronic inflammation, (c) cholesterolosis, (d) presence of cholesterol polyp, and (e) gastric metaplasia.
Statistical Analysis
Data were expressed as median (interquartile range), mean ± SD, and percentages. Data were analyzed by Chi-square test, Mann–Whitney U tests, and the multiple logistic regressions where appropriate. A P value of less than 0.05 was considered statistically significance. The SPSS statistical software (SPSS, Inc., Chicago, IL) was used for statistical analysis.
Results
Patient Characteristics
We studied 152 morbid obese patients with fatty liver consisting of 59 men and 93 women. The mean age was 30.3 ± 8.9 years. The mean BMI was 44.9 ± 5.4 kg/m2. Fifty-four patients (54/152, 35.5%) were diagnosed as NASH. Eleven patients (11/152, 7.2%) received concomitant laparoscopic cholecystectomy because of gallbladder stone(s).
Comparison Between NASH and Gallbladder Disease (GD) in Morbid Obesity Presented with Fatty Liver
Table 1 summarizes the demographic and clinical characteristics between NASH and GD groups in morbid obese patients with fatty liver disease. The mean BMI was similar in both groups. The clinical factors of age (P = 0.020), total bilirubin (P = 0.044), cholesterol (P = 0.020), low-density lipoprotein cholesterol (P = 0.044), C-peptide (P = 0.023), and insulin (P = 0.039) were significantly different. Patients with fatty liver disease and GD were significantly older, had higher serum total cholesterol, higher serum LDL-cholesterol and higher HOMA-IR levels than those in the NASH group. Steatosis (P = 0.012), ballooning degeneration (P = 0.001), lobular inflammation (P = 0.019), fibrosis (P = 0.026), and glycogenated nuclei (P = 0.028) were identified as significantly different pathological factors between two groups. However, further multivariate analysis failed to demonstrate any independent factor between these two groups.
Histology Features of Liver and Gallbladder in 11 Gallbladder Disease (GD) Obese Patients
The histological findings are summarized in Table 2. Most patients present steatosis, ballooning degeneration, lobular inflammation, portal inflammation, and fibrosis in their liver biopsy specimens. The prevalence of chronic hepatitis B and NASH was the same (18%) in all 11 gallbladder disease patients. Our data did not enroll any hepatitis C carrier or alcoholic fatty liver disease in those who received liver biopsy and concomitant cholecystectomy.
Factors Associated with NASH Versus Concurrent NASH–Gallbladder Disease (NASH–GD)
Patients with NASH (n = 54) were compared with concurrent NASH-GD (n = 2). Among the clinical variables tested during univariate analysis, waist (NASH vs. NASH-GD: 127.1 ± 13.4 vs. 9.7 ± 1.3; P = 0.016), waist/hip (NASH vs. NASH–GD: 0.9 ± 0.1 vs. 0.8 ± 0.0; P = 0.039), and HOMA-IR (NASH vs. NASH–GD: 5.0 ± 4.2 vs. 9.7 ± 1.3; P = 0.040) were independent associated factors (data not shown). Further multivariate analysis has failed to analyze any independent factor.
Fibrosis Stage, Degree of HOMA-IR in NASH Versus Gallbladder Disease (GD)
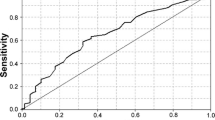
Obesity, NASH, and gallbladder disease are tightly related to insulin resistance. It is unknown whether liver fibrosis is associated with insulin resistance in NASH and GD groups. Therefore, we further assessed the HOMA-IR (quartiles of HOMA) distribution and the relationship between fibrosis stage in patients with NASH and GD. In the NASH group, HOMA-IR distribution progressively decreased when the severity of fibrosis was plotted as a function of insulin resistance (Fig. 1). The first quartile of HOMA-IR showed significantly different (r = 0.567, P = 0.039) between two different groups.
Discussion
In obese population, systemic chronic inflammatory status is believed to play an important role in the pathogenesis of steatohepatitis, atherosclerosis, cardiovascular diseases and gallbladder disease [25–27]. The prevalence of NASH and gallbladder disease was 33.8% [21] and 10.1% [28], respectively, among obese population in Asia. In this study, we first compared the clinical risk factors between NASH and gallbladder disease among morbid obesity that had fatty liver disease undergoing bariatric surgery. Gallbladder disease among morbidly obese patients with fatty liver were significantly older, had higher serum levels of cholesterol and LDL cholesterol and had lower serum levels of total bilirubin, C-peptide, and insulin than the NASH group. Our study confirmed that age was a common risk factor associated with gallbladder disease in general and obese populations. In addition, the present study supported the existence of a more important pathogenic link between gallbladder disease and serum cholesterol and LDL-cholesterol levels. The most important pathogenic event in gallstone formation is the secretion of hepatic bile supersaturated with cholesterol, and hypersecretion of biliary cholesterol is the most common cause of lithogenic bile in humans. It has been well-known that bile acid synthesis significantly correlates with very low-density lipoprotein (VLDL) production. Hyperinsulinemia has shown to be associated with increased risk of gallstones. Insulin may play a role in gallstone formation by two mechanisms: increasing cholesterol saturation of bile and decreasing gallbladder motility. Insulin also activates low-density lipoprotein (LDL) receptors in the liver, thereby increasing cholesterol excretion in the bile. An association of gallbladder disease with higher fasting serum insulin and C-peptide levels in normal BMI women was reported from a large, national, population-based sample [29]. Although the association of gallbladder disease with insulin and C-peptide level was less significant when compared with the NASH group in our study, this observation may suggest that diabetes appears to be a risk factor for both gallbladder disease and NASH, regardless of the presence of other factors. The failure of control group study to account for the association of diabetes, gallbladder disease, and NASH is one of the limitations of this study. On the other hand, the histopathology findings of steatosis, ballooning degeneration of hepatocytes, lobular inflammation, glycogenated nuclei, and fibrosis stage were different between NASH and gallbladder disease. These findings were closely related to the pathogenesis of NASH. We have failed to demonstrate any significantly risk factor regarding to the histopathology of gallbladder between NASH and gallbladder disease. On the contrary, we did not observe any significantly different in the liver function test, blood pressure, high-sensitivity CRP, and adiponectin level between NASH and gallstone disease.
We next analyzed the histological features of liver and gallbladder in obese patients with gallstone disease. Most morbidly obese patients present mild steatosis, mild ballooning degeneration, mild lobular inflammation, mild portal inflammation, and mild fibrosis in their liver biopsy specimens [30]. The resected gallbladder specimens display acute and chronic inflammatory infiltrate, mild cholesterolosis, and minimal gastric metaplasia. The prevalence of NASH in GD of our morbidly obese population was 18%, which was similar to the prevalence reported by Loria P et al. in normal BMI general population [19]. Uric acid and apolipoprotein-B were found to be associated with the gallstone disease in nonalcoholic fatty liver disease in this previous study. A previous report among Chinese in Taiwan demonstrated that the prevalence of concurrent gallstone and fatty liver was 6.5% [18]. A previous epidemiology study of comorbidity of liver and gallstone disease in a large population [31] reported that cholelithiasis occurred in 13.7% of patients with nonalcoholic liver cirrhosis. Other risk factors for cholelithiasis besides liver disease were female gender, older age, Native American or Hispanic ethnicity, and presence of diabetes mellitus. In our current study, we only enrolled two patients with concurrent NASH and gallbladder disease. Interestingly, we observed an increase of HOMA-IR in patients with concurrent NASH-GD than NASH (P = 0.040). This may explain the important role of insulin resistance in these two diseases. However, given the relatively limited sample size, further studies are needed in a larger cohort to address this interesting issue.
The prevalence of chronic hepatitis B in gallbladder disease in our study was 18%. The prevalence of HBsAg and chronic B hepatitis was 4.4–4.5% in gallstone disease among normal BMI population in Taiwan [18]. A prospective study by Sheen and Liaw [20] showed a linear trend toward the prevalence of cholecystolithiasis increased with the progression of liver disease, i.e., from “healthy” HBsAg carrier through chronic hepatitis to liver cirrhosis. Chronic hepatitis B seems to be a risk factor for gallbladder disease [28]. Paradoxically, chronic hepatitis B was not a risk factor in the development of NASH [21] and HBsAg-positive subjects had less prevalence of metabolic syndrome than HBsAg-negative subjects [32]. Further longitudinal studies are indicated to verify the complex relationship between the role of hepatitis B viral replication, gallbladder disease, NASH, liver fibrosis, and metabolic syndrome in obese population.
Insulin resistance is an important risk factor in NASH and gallbladder disease. The association between insulin resistance and fibrosis in NASH and gallbladder disease remains unknown. Hyperinsulinemia induces hepatic stellate cell proliferation, whereas high levels of glucose unregulated the expression of profibrogenic cytokines. Lipid peroxidation by-products and inflammatory cytokines released by injured cells have shown to act as paracrine mediators of hepatic stellate cell activation. Therefore, hepatic fibrosis might be caused by complex independent risk factors of liver steatosis, insulin resistance, and systemic inflammatory cytokines production in NASH. On the other hand, several studies suggested that the risk of developing gallstones was correlated with the severity of liver cirrhosis as graded by the Child–Pugh classification [33]. In this study, performed in morbid obese patients, we observed progressively decreased when the severity of fibrosis was plotted as a function of insulin resistance in NASH group. We could rarely observe any relationship between gallbladder disease, fibrosis stage, and insulin resistance. Mechanisms of this association are unclear. For a better understanding of this complex relationship, further studies should be addressed to investigate the coordinated control of energy metabolism and glucose and lipid homeostasis communication between liver and other organs.
In conclusion, the prevalence of NASH in gallbladder disease was 18% in morbid obese patients. Age was a common risk factor associated with gallbladder disease in normal BMI and obese population. Serum cholesterol and low-density lipoprotein cholesterol levels demonstrated a more important pathogenic link to gallbladder disease than NASH. Insulin resistance is more common in concurrent NASH and gallbladder disease. Insulin resistance seems to be a common pathogenic mechanism associated with hepatic fibrosis, but the mechanism between NASH and gallbladder disease is unknown.
Abbreviations
- BMI:
-
Body mass index
- NASH:
-
Nonalcoholic steatohepatitis
- NAS:
-
NAFLD activity score
- GD:
-
Gallbladder disease
- CHB:
-
Chronic hepatitis B
- GGT:
-
γ-glutamyltransferase
- HOMA-IR:
-
Homeostatic model assessment method-insulin resistance
- ALT:
-
Alanine transaminase
- AST:
-
Aspartate transaminase
- LDL-C:
-
Low-density lipoprotein cholesterol
- HDL-C:
-
High-density lipoprotein cholesterol
References
Ludwig J, Viggiona TR, McGill DB, et al. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hither-to unnamed disease. Mayo Clin Proc. 1980;55:434–8.
Dixon JB, Bhathal PS, O’Brien PE. Nonalcoholic fatty liver disease: predictors of nonalcoholic steatohepatitis and liver fibrosis in severely obese. Gastroenterology. 2001;121:91–100.
Angulo P, Keach JC, Butts KP, et al. Independent predictors of liver fibrosis in patients with nonalcoholic steatohepatitis. Hepatology. 1999;30:1356–62.
Ong JP, Elariny H, Collantes R, et al. Predictors of nonalcoholic steatohepatitis and advanced fibrosis in morbidly obese patients. Obes Surg. 2005;15:310–5.
Moretto M, Kupski C, Mottin CC, et al. Hepatic steatosis in patients undergoing bariatric surgery and its relationship to body mass index and co-morbidities. Obes Surg. 2003;13:622–4.
Wolf AM, Busch A, Kuhlmann HW, et al. Histological changes in liver of morbidly obese patients: correlation with metabolic parameters. Obes Surg. 2005;15:228–37.
Harnois F, Msika S, Sabate J-M, et al. Prevalence and predictive factors of non-alcoholic steatohepatitis (NASH) in morbidly obese patients undergoing bariatric surgery. Obes Surg. 2006;16:183–8.
Aidonopouios AP, Papavramidis ST, Zaraboukas TG, et al. Gallbladder findings after cholecystectomy in morbidly obese patients. Obes Surg. 1994;4:8–12.
Fobi M, Lee H, Igwe D, et al. Prophylactic cholecystectomy with gastric bypass operation: incidence of gallbladder disease. Obes Surg. 2002;12:350–3.
Dittrick GW, Thompson JS, Campos D, et al. Gallbladder pathology in morbid obesity. Obes Surg. 2005;15:238–42.
Liew P-L, Lee Y-C, Lin Y-C, et al. Comparison of artificial neural networks with logistic regression in prediction of gallbladder disease among obese patients. Dig Liver Dis. 2007;39:356–62.
Seinige UL, Sataloff DH, Lieber CP, et al. Gallbladder disease in the morbidly obese patient. Obes Surg. 1991;1:51–6.
Pagliarulo M, Fornari F, Fraqueli M, et al. Gallstone disease and related risk factors in a large cohort of diabetes patients. Dig Liver Dis. 2004;36:130–4.
Fraquelli M, Pagliarulo M, Colucci A, et al. Gallbladder motility in obesity, diabetes mellitus and coeliac disease. Dig Liver Dis. 2003;35:S12–6.
Sanyal AJ, Campbell-Sargent C, Mirshahi F, et al. Nonalcoholic steatohepatitis: association of insulin resistance and mitochondrial abnormalities. Gastroenterology. 2001;120:1183–92.
Chitturi S, Abeygunasekera S, Farrell GC, et al. NASH and insulin resistance: insulin hypersecretion and specific association with the insulin resistance syndrome. Hepatology. 2002;35:373–9.
Nervi F, Miquel JF, Alvarez M, et al. Gallbladder disease is associated with insulin resistance in a high risk hispanic population. J Hepatol. 2006;45:299–306.
Lu S-N, Chang W-Y, Wang L-Y, et al. Risk factors for gallstones among Chinese in Taiwan. J Clin Gastroenterol. 1990;12:542–6.
Loria P, Lonardo A, Lombardini S, et al. Gallstone disease in non-alcoholic fatty liver: prevalence and associated factors. J Gastroenterol Hepatol. 2005;20:1176–84.
Sheen I-S, Liaw Y-F. The prevalence and incidence of cholecystolithiasis in patients with chronic liver diseases: a prospective study. Hepatology. 1989;9:538–40.
Liew P-L, Lee W-J, Lee Y-C, et al. Hepatic histopathology of morbid obesity: concurrence of other forms of chronic liver disease. Obes Surg. 2006;16:1584–93.
Haffner SM, Miettinen H, Stern MP. The homeostasis model in the San Antonio Heart Study. Diabetes Care. 1997;20:1087–92.
Brunt EM, Janney CG, Bisceglie AMD, et al. Nonalcoholic steatohepatitis: a proposal for grading and staging histologic lesions. Am J Gastroenterol. 1999;94:2467–74.
Kleiner DE, Brunt EM, Natta MV, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–21.
Silverman JF, O’ Brien KF, Long S, et al. Liver pathology in morbidly obese patients with and without diabetes. Am J Gastroenterol. 1990;85:1349–55.
Gholam PM, Kotler DP, Flancbaum LJ. Liver pathology in morbidly obese patients undergoing Roux-en-Y gastric bypass surgery. Obes Surg. 2002;12:49–51.
Dixon JB, Bhathal PS, Hughes NR, et al. Nonalcoholic fatty liver disease: improvement in liver histological analysis with weight loss. Hepatology. 2004;39:1647–54.
Liew P-L, Weu Wang, Yi-Chih L, et al. Gallbladder disease among obese patients in Taiwan. Obes Surg. 2007;17:383–90.
Ruhl CE, Everhart JE. Association of diabetes, serum insulin, and C-peptide with gallbladder disease. Hepatology. 2000;31:299–303.
Papadia FS, Marinari GM, Camerini G, et al. Liver damage in severely obese patients: a clinical-biochemical-morphologic study on 1,000 liver biopsies. Obes Surg. 2004;14:952–8.
Buchner AM, Sonnenberg A. Factors influencing the prevalence of gallstones in liver disease: the beneficial and harmful influences of alcohol. Am J Gastroenterol. 2002;97:905–9.
Chu C-M, Lin D-Y, Liaw Y-F. Does increased body mass index with hepatic steatosis contribute to seroclearance of hepatitis B virus (HBV) surface antigen in chronic HBV infection? Int J Obes. 2007;31:1–5.
Conte D, Fraquelli M, Fornari F, et al. Close relation between cirrhosis and gallstones. Arch Intern Med. 1999;159:49–52.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liew, PL., Lee, WJ., Wang, W. et al. Fatty Liver Disease: Predictors of Nonalcoholic Steatohepatitis and Gallbladder Disease in Morbid Obesity. OBES SURG 18, 847–853 (2008). https://doi.org/10.1007/s11695-007-9355-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-007-9355-0