Abstract
Vascular cognitive impairment, no dementia (VCIND) refers to cognitive deficits associated with underlying vascular causes that are insufficient to confirm a diagnosis of dementia. The default mode network (DMN) is a large-scale brain network of interacting brain regions involved in attention, working memory and executive function. The role of DMN white matter integrity in cognitive deficits of VCIND patients is unclear. Using diffusion tensor imaging (DTI), this study was carried out to investigate white matter microstructural changes in the DMN in VCIND patients and their contributions to cognitive deficits. Thirty-one patients with subcortical VCIND and twenty-two healthy elderly subjects were recruited. All patients underwent neuropsychological assessments and DTI examination. Voxel-based analyses were performed to extract fractional anisotropy (FA) and mean diffusivity (MD) measures in the DMN. Compared with the healthy elderly subjects, patients diagnosed with subcortical VCIND presented with abnormal white matter integrity in several key hubs of the DMN. The severity of damage in the white matter microstructure in the DMN significantly correlated with cognitive dysfunction. Mediation analyses demonstrated that DTI values could account for attention, executive and language impairments, and partly mediated global cognitive dysfunction in the subcortical VCIND patients. DMN integrity is significantly impaired in subcortical VCIND patients. The disrupted DMN connectivity could explain the attention, language and executive dysfunction, which indicates that the white matter integrity of the DMN may be a neuroimaging marker for VCIND.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebrovascular disease remains a leading cause of death and disability in older people worldwide(Mansfield et al. 2018). In addition to causing physical disabilities, cerebrovascular disease could also contribute to cognitive impairment. Vascular cognitive impairment (VCI) refers to all forms of cognitive dysfunction consisting of a complex interaction of cerebrovascular disease and risk factors that lead to changes in brain structures due to strokes and lesions(Skrobot et al. 2018). VCI ranges from subjective cognitive decline and mild cognitive impairment (vascular cognitive impairment, no dementia; VCIND) to overt dementia (vascular dementia)(Sachdev et al. 2014). Vascular cognitive impairment, no dementia refers to cognitive deficits associated with underlying vascular causes that fall short of a diagnosis of dementia(Stephan et al. 2009). According to the China Cognition and Aging Study, VCIND is the most common subtype of mild cognitive dysfunction in China, accounting for 42.0% of the total cases(Jia et al. 2014). The Canadian Study of Health and Aging pointed out that 50 % of VCIND patients progressed to dementia over 5 years of follow-up(Rockwood et al. 2000). Therefore, it is very important for us to investigate the brain alterations in VCIND subjects.
Subcortical VCIND manifests as white matter hyperintensities or lacunes in subcortical white matter and the basal ganglia on magnetic resonance imaging (MRI), and these regions contribute to cognitive deficits(van de Pol et al. 2007). However, the role of white matter hyperintensity in cognitive deficits is still controversial. Previous studies suggested that the white matter hyperintensity severity rather than the distribution correlates with cognitive deficits(Fazekas et al. 1996), whereas other studies came to the opposite conclusion(de Vocht 2007; Debette et al. 2007; Mirsen et al. 1991). The inconsistency may arise from methodological differences in evaluating white matter hyperintensity. One potential factor is the variability in the pathologies that underlie white matter hyperintensity. These white matter hyperintensities could be composed of various lesions, ranging from multiple small cavitations, marked arteriosclerosis and mild perivascular alterations to loss of various tracts(Fazekas et al. 1993). Another potential factor that can explain these inconsistencies is the poor discrimination of absolute lesion volume and the visual rating scales of white matter hyperintensity displaying a ceiling effect(Kim et al. 2011; van Straaten et al. 2006). Therefore, precise measurements are needed to reveal the role of white matter hyperintensities in cognitive deficits in patients with subcortical VCIND.
Diffusion tensor imaging (DTI), a sensitive magnetic resonance imaging (MRI) based technique, is a noninvasive measurement used for delineating specific white matter structures in vivo(Nitkunan et al. 2006). A recent study demonstrated that abnormal DTI parameters significantly correlated with the level of metabolite contents of neurons, suggesting that DTI can identify axonal disruption in the white matter tracts(Robinson et al. 2016). DTI detects white matter microstructural alterations by measuring the directionality of molecular diffusion (fractional anisotropy, FA) and the average motion of water molecules (mean diffusivity, MD)(Xu et al. 2010). However, most DTI studies have used manual tracing of regions of interest (ROIs) and thus included only limited regions or assessing whole brain areas(O'Sullivan et al. 2004) rather than neural networks. Recent dementia studies have pointed out that neurodegenerative diseases are considered brain network diseases due to the failure to integrate certain brain regions into an efficient network and the disconnections within neural networks(Della Nave et al. 2007; Zhou et al. 2008). The default mode network (DMN) is one of the most important brain networks involved in executive and attention function(Buckner et al. 2008). It was first introduced by Raichle(Raichle et al. 2001) and colleagues and has gained increasing attention from the neurology and neuroscience communities ever since(Rosazza and Minati 2011). This network is composed of the posterior cingulate cortex (PCC), the adjacent precuneus (pCu), the retrosplenial cortex (RSC), the medial temporal lobes (MTL), medial prefrontal areas (mPFC) and the inferior parietal cortex. This set of regions is intensely activated during the resting state and de-activated during the demanding tasks requiring focused attention such as visual-spatial tasks and working memory tasks(Corbetta and Shulman 2002). Activation of the DMN regions also correlates with other networks during executive tasks(Leech et al. 2011). Convergent evidence demonstrates DMN connectivity alterations in AD and MCI patients(Agosta et al. 2013; Chua et al. 2008; Filippi et al. 2013; Li et al. 2019; Weiler et al. 2014; Zhan et al. 2016), and these alterations have been found to be related to the severity and the progression of the disease(Hansen et al. 2014; Mintun et al. 2006). Additionally, in VaD, decreased DMN functional connectivity has been reported using resting-state functional MRI (fMRI)(Kim et al. 2011). While fMRI provides an indirect evaluation of neural activity, DTI is a direct measurement of white matter structural integrity.
To date, little is known regarding white matter structural integrity in the DMN in VCIND patients and even less is known regarding its role in cognitive deficits. Therefore, the main aim of the present study is to investigate the contributions of white matter microstructural abnormalities in the DMN to cognitive impairment in patients with subcortical VCIND. In pursuit of this, using the DTI method, we investigate white matter tract integrity in the DMN and the cognitive consequences of this hypothesized disconnection in subcortical VCIND.
Materials and methods
This study received approval from the institutional review board at Xuan Wu Hospital Capital Medical University. Informed written consent was obtained from each participant. The methods were carried out in accordance with the Declaration of Helsinki.
Subjects
Thirty-one consecutive patients with subcortical VCIND were prospectively recruited from the memory clinic at Xuan Wu Hospital. All patients were diagnosed by a consensus group of three senior neurologists. The patients met the following inclusion criteria: (1) there was an informant report and/or complaint of cognitive dysfunction involving memory impairments and/or other cognitive domain deficits that continued for more than 3 months; (2) the patients were neither normal nor demented according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition(Winblad et al. 2004), and these criteria comprised: a clinical dementia rating (CDR) ≥ 0.5 on at least one domain(Hughes et al. 1982) and global score = 0.5, and a Mini-Mental State Examination (MMSE) score ≥ 20 (primary school) or ≥ 24 (junior school or above)(Folstein et al. 1975; Zhang et al. 1990); (3) the patients had normal or slightly impaired daily living activities as defined by a total score of ≤1.5 for the three functional CDR domains (home and hobbies, community affairs, and personal care)(Zhang et al. 1990); (4) the patients were literate Han Chinese with a consistent caregiver (>4 days/week). Participants who had disorders other than subcortical VCIND that would affect cognition or any conditions that would preclude completion of neuropsychological testing were excluded.
All patients meeting the clinical criteria underwent MRI screening including a hippocampal assessment. The MRI-based entry criteria details were as follows: (1) multiple (≥3) supratentorial subcortical small infarcts (3–20 mm in diameter) with/without white matter lesions of any degree or moderate to severe white matter lesions (Fazekas rating scale score ≥ 2)(Fazekas et al. 1987); with/without small infarcts; (2) absence of cortical or watershed infarcts, hemorrhages, hydrocephalus, or white matter lesions with specific causes (e.g., multiple sclerosis); and (3) no hippocampal or entorhinal cortex atrophy (score of 0 on the medial temporal lobe atrophy scale of Scheltens (Scheltens et al. 1992).
Twenty-two healthy elderly subjects were recruited from the community and served as a normal control (NC) group. These healthy individuals were free from a history of any major medical, neurological, or psychiatric illness. No apparent abnormal findings or cognitive impairment were identified in MRI or neuropsychological testing.
Neuropsychological assessment
Neuropsychological evaluations included the MMSE, the Montreal Cognitive Assessment (MoCA), the CDR scales, Clock drawing Test, Digit Span, the Trail Making Test (TMT) A and B, the WHO-UCLA Auditory Verbal Learning Test (AVLT), the Boston Naming Test (BNT), the Hachinski Ischemic Scale (HIS), the Geriatric Depression Scale (GDS), the Neuropsychiatric Inventory and the Activities of Daily Living (ADL) assessment.
Imaging data acquisition
Imaging data were collected on a 3.0 Tesla (Skyra Siemens, Germany) scanner. Brain structural MRI data were collected with a three-dimensional (3D) magnetization-prepared rapid gradient echo (MP-RAGE) squeeze with the following parameters: repetition time (TR) = 2100 ms, echo time (TE) =2.56 ms, field of view (FOV) = 256 mm × 256 mm, acquisition matrix = 256 × 256, flip angle (FA) = 12°, and slice thickness = 1 mm with 192 slices. The diffusion tensor images were collected with alignment to the AC-PC line using a double spin-echo EPI sequence (TR = 7500 ms, TE = 96 ms, flip angle = 90°, FOV = 240 mm × 240 mm, in-plane resolution = 1.75 mm × 1.75 mm voxels, and 54 contiguous 2-mm-thick axial slices) with 64 non-collinear encoding directions (b = 1000 s/mm2) and 11 images without diffusion weighting (b = 0 s/mm2, b0). FLAIR images were acquired for Fazekas rating (TR = 8500 ms, TE = 81 ms, time inverse = 2440 ms, FOV = 240 mm × 240 mm, acquisition matrix = 320 × 320, thickness = 3 mm, 3.15 mm gap, 19 slices).
ROI definition
The default mode network (DMN) was defined directly from our previous study(Tao et al. 2015). Briefly, a data-driven method was used to extract the mask of the DMN. After obtaining the independent components, a threshold of Z > 2 was used to obtain eight ROIs.
DTI processing and tractography
All data preprocessing and processing procedures for the DTI data were implemented using the Brainnetome diffusion toolkit (http://diffusion.brainnetome.org) (Xie et al. 2016). The preprocessing of the DTI data included the following steps: (1) converting DICOM data; (2) extracting a brain mask; (3) correcting for eddy current and head motion; (4) fitting diffusion tensors to the data. Tensor calculation and tractography were performed with a deterministic stream line method to obtain tracts by setting the fractional anisotropy (FA) threshold to 0.25 and the angular threshold to 60°. An FA threshold of 0.25 was chosen to avoid voxels that are not part of the white matter tract (cortex has FA~0.2), minimize the inclusion of voxels with a higher degree of partial volume contamination, and limit the presence of spurious tracts. (5) Registering ROIs from MNI space to the individual space; (6) Tract pruning, which involved, for each pair of brain regions in the DMN, extracting the tracts start in one region and end in the other one. Then the mean FA, mean MD and number of the tracts were calculated for the tracts linking each pair of brain regions.
Statistical analysis
Statistical data analysis was performed using the SPSS (Version 20, SPSS Inc., Chicago, IL, USA). An independent sample t test was used separately for the assessment criterion and the functional rating scales between the VCIND and control groups. For the tracts linking the regions within the DMN, only the tracts with more than 80% of the subjects were further analysed. The mean FA, mean MD and tract numbers were compared between groups with a two-sample two-tailed t-test at P < 0.05 (Bonferroni corrected, N = the statistical tract numbers). Partial correlation analyses controlling for age, sex and education were used to study the relationship between white matter pathways and neuropsychological scores (P < 0.05, Bonferroni corrected, N = the statistical tract numbers).
To further estimate the mediation effect of groups between the cognitive abilities and white matter properties (FA, MD), we subsequently performed a mediation analysis with the linear regression method(Baron and Kenny 1986; Liu et al. 2017). Only variables that were significantly correlated with FA or MD values in the DMN were included in the mediation analysis. DTI values in the DMN as mediations of the associations between diagnostic group and neuropsychological evaluations were tested.
Results
Demographics
Table 1 displays demographics and the main neuropsychological statistics for the normal controls and VCIND subjects. There were no differences across groups regarding age, years of education and sex (P > 0.05). As expected, the VCIND patients performed significantly worse on the MMSE, MoCA, and Clock drawing task than the NCs (all P < 0.001). The VCIND patients also showed poor performance on the Boston Naming test, Digit span, Trail Making test and AVLT test (P < 0.05).
DTI values in the DMN across groups
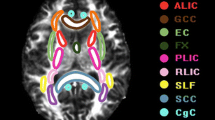
For both the NC and VCIND subjects, 20 tracts were evaluated for group differences. Among these connectivities, the VCIND subjects showed reduced FA values in the left TP-mPFC and PCC-right TP compared with the NCs (P < 0.05, Bonferroni corrected). Compared to the NCs, the VCIND patients showed higher MD in 8 pairs of connectivities (including the following links of PCC-mPFC, PCC-right supF, right TP-mPFC, mPFC-left HIP, left TP-left HIP, left TP-left supF and left TP-right TP and left TP-mPFC) at P < 0.05 (Bonferroni corrected) (Fig. 1). In summary, decreased FA and increased MD values were widespread throughout the DMN.
Significantly different DTI values across groups in DMN. a FA values decreased in the PCC-right TP and left TP-mPFC tracts in the VCIND patients. b Compared to the NCs, the VCIND patients showed higher MD in the link of the PCC-mPFC, PCC-right supF, right TP-mPFC, mPFC-left HIP, left TP-left HIP, left TP-left supF and left TP-right TP tracts
Correlations between DMN connectivity and neuropsychological tests
As shown in Fig. 2, overall, the results revealed that the DTI parameters (especially MD) in the DMN were significantly correlated with cognitive scores in VCIND subjects.
For FA, positive correlations were detected between FA and MoCA in the PCC-right TP, revealing that a higher FA in this link was associated with better cognitive function. For MD, we found a significant negative correlation between MMSE and MoCA and MD in several connectivities, including left TP-mPFC, mPFC-left HIP, PCC-mPFC, PCC-right supF, left TP-left HIP and right TP-mPFC, which indicated that higher MD was associated with worse cognitive function. Moreover, we found that MoCA showed a stronger correlation with DTI values than MMSE, which suggested that MoCA might be more sensitive to detect general cognitive impairment in VCIND patients (Fig. 2).
For specific cognitive domains, no significant correlations were found between FA, MD and memory function as measured by the AVLT. Visual-spatial and executive function detected by Clock drawing test showed negative correlation with MD in five tracts (left TP-left supF, PCC-mPFC, left TP-mPFC, left TP-left HIP and left TP-left HIP) (Fig. 2). Moreover, executive function measured by Trail Making Test-B showed significant negative relationship with MD values in the PCC-right supF and right TP-mPFC tracts. Attention measured by Back Digit Span showed a strong correlation with MD values in the left TP-mPFC, mPFC-left HIP, PCC-right supF and left TP-left HIP tracts. As for language abilities measured by Boston Naming test, they were found to be significantly associated with FA in the PCC-right TP link and MD in the PCC-mPFC link.
Mediation analysis results
For general cognitive function (Table 2), we found a significant mediation between the MMSE, MoCA scores and DTI values. For MoCA scores, FA, MD and the group effect were all significant when FA, MD values and group were entered into the regression model in the PCC-right TP, right TP-mPFC and PCC-mPFC tracts, revealing that DTI values on these three links partly mediated the group-cognition relationship. In other hubs that DTI values correlated with MoCA scores, a significant group-cognition association was absent, but the FA and MD effects were significant, revealing full mediation of FA and MD on the group-MoCA association. For MMSE scores, in mPFC-left HIP, PCC-right supF and left TP-left HIP tracts, significant group-cognition association was absent when MD values were entered into the regression model, but the MD effects were significant, revealing full mediation of FA on the group-MMSE association.
For specific cognitive domains (Table 3), significant mediations were also found between neuropsychological assessment scores and DTI values. For Clock drawing test, full mediation of MD on the group-cognition association was found in the left TP-mPFC, left TP-left supF, left TP-right TP and left TP-left HIP tracts. In the PCC-mPFC, MD partly mediated the group-cognition relationship. For Trail Making Test B, Backward Digit Span and Boston Naming test, significant group-cognition effects were absent when FA and MD values were entered into the regression model, but FA and MD effects were significant, revealing full mediation of FA and MD on the group-cognition associations in the DMN.
Discussion
The main aim of the present study was to detect the white matter microstructural changes in the default mode network and investigate the role of white matter damage in cognitive deficits in patients with subcortical VCIND. The results showed significant microstructural alterations in key regions of the DMN network, which mediated cognitive dysfunction in the VCIND patients.
As reported in previous studies, the conclusions about white matter microstructural changes in VCI patients have been controversial. On the one hand, researchers had found reduced FA and increased MD values only in a limited number of regions. For example, several studies found decreased FA in the anterior CC, frontal, and parietal white matter in VaD(H. J. Chen et al. 2018; Lin et al. 2015; Zarei et al. 2009). Other studies reported that FA decreased and ADC increased in the regions of frontal, parietal, temporal, and centrum semiovale areas in VCI patients (Lopez-Oloriz et al. 2014; Sun et al. 2011). On the other hand, several groups have reported that VCIND patients had more widespread white matter changes. They found that FA values decreased and MD values increased in all supratentorial white matter, including the frontal lobes, parietal lobes, temporal lobes, occipital lobes, and corpus callosum (Chua et al. 2008; Zhou et al. 2011). As previously mentioned, neurodegenerative diseases could be considered as brain network diseases due to the disconnection within neural networks and the failure to integrate certain brain regions into an efficient network(S. Q. Chen et al. 2016; Della Nave et al. 2007; Zhou et al. 2008). The DMN is one of the most important brain networks involved in attention and executive function (Qiu et al. 2009). Hence, the present study confirmed the role of white matter microstructural changes in the DMN in cognitive deficits in patients with subcortical VCIND.
Previous studies have reported correlations between cognitive impairments and white matter microstructural changes as reflected by DTI metrics in VaD patients(Kim et al. 2011; Thong et al. 2014; Xu et al. 2010; Zhou et al. 2008, 2011). However, no conclusions had been drawn regarding VCIND patients yet. Our current findings demonstrate that damages in white matter tracts already contribute to cognitive impairment in the early stage of VCI. A noteworthy hypothesis to explain the cognitive impairment in VCIND patients is that nerve tract damage results in a disconnection syndrome due to the disruption of large tracts of white matter(Chua et al. 2008; Lin et al. 2015). Our results, in line with previous results, provided additional evidence that damage to white matter tracts might be an important mechanism of cognitive impairment in VCIND patients.
It is known that executive and attention dysfunction, but not memory loss, are characteristic impairments in patients with subcortical VCIND (Seo et al. 2010, 2012). Here, within the DMN, correlation analyses revealed that DTI values were significantly correlated with general cognitive function, assessed with the MMSE, MoCA and specific cognitive domains including visual-spatial, language, attention and executive function. There is no correlation between DTI values and memory function. Furthermore, although DTI-cognition associations were identified, it is unclear whether these associations were due to contributions from a third variable or whether the group-related cognitive differences were due to the group DTI differences. A mediation analysis revealed that DTI changes in the DMN could fully explain the group-related differences in cognitive function. DTI values in the DMN not only mediated impairments in global cognitive function, but also mediated impairments in language, attention and executive functions, as measured by Boston Naming Test, Trail Making Test and Backward Digit Span.
Moreover, the current study revealed different levels of sensitivity of the neuropsychological tests in their correlations with the white matter damage. The National Institute of Neurological Disorders and Stroke-Canadian Stroke Network had recommended MoCA for clinical trials of vascular dementia(Hachinski et al. 2006). Previous researchers found that MoCA showed better sensitivity and specificity in the diagnosis of vascular cognitive dysfunction (Pinto et al. 2018). Our results further demonstrated that MoCA is highly correlated with white matter integrity compared to MMSE for general cognitive assessments in patients with subcortical VCIND. As the most commonly used screening tool for cognitive function, MoCA seems to be superior to MMSE in the identification and detection of of VCI, and more related to white matter integrity damage.
A potential limitation is the cross-sectional nature of the current study. Longitudinal observations from early stage VCIND to dementia would help us to better understand the dynamic changes in the role of the DMN in the cognitive deficits of VCI. The present study was based in a single hospital and had a relatively small sample size. Studies combining population-based multicenter research and large sample sizes should be promoted in the future. Moreover, as demonstrated by post-mortem studies, the co-occurrence of VCI and other neurodegenerative disorders in the elderly is very frequent (Debette et al. 2007). When we selected patients, we have performed various physical and auxiliary examinations to exclude the possibility of co-existing neurodegenerative diseases. However, we could not completely exclude the possibility that the VCIND patients included in our study might also suffer from other confounding preclinical cognitive disorders. A further cross-validation study with properly controlled diagnostic biomarkers for AD, Lewy body diseases, etc. would be needed. Additionally, the associations between white matter integrity and other fibers might enhance our understanding about the brain connectivity and brain function in VCI subjects, therefore, some related analysis should be performed in the future. Finally, it should be noted that we cannot infer that the cognitive changes are specifically associated with white matter changes in the DMN and not driven by generalized white matter changes or changes in other networks. In fact, we have investigated the altered patterns among other regions area using a latest well-used Brainnetome Atlas (Fan et al. 2016), and around 0.1–0.5% connections showed impaired FA or MD properties in VCIND subjects. Hence, additional work to investigate the specific change of brain network in VCIND are needed in the future studies.
In conclusion, the current study revealed significant white matter integrity damage in the DMN in patients with subcortical VCIND. The damage in DMN white matter tracts mediated the characteristic cognitive deficits in VCIND patients, including executive function and attention. The microstructural white matter evaluation could provide insight into the pathogenesis of cognitive impairments in VCIND, as well as potential imaging biomarkers.
References
Agosta, F., Caso, F., & Filippi, M. (2013). Dementia and neuroimaging. Journal of Neurology, 260(2), 685–691. https://doi.org/10.1007/s00415-012-6778-x.
Baron, R. M., & Kenny, D. A. (1986). The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173–1182. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/3806354.
Buckner, R. L., Andrews-Hanna, J. R., & Schacter, D. L. (2008). The brain's default network: anatomy, function, and relevance to disease. Annals of the New York Academy of Sciences, 1124, 1–38. https://doi.org/10.1196/annals.1440.011.
Chen, S. Q., Cai, Q., Shen, Y. Y., Xu, C. X., Zhou, H., & Zhao, Z. (2016). Hydrogen proton magnetic resonance spectroscopy in multidomain amnestic mild cognitive impairment and vascular Cognitive impairment without dementia. American Journal of Alzheimer's Disease and Other Dementias, 31(5), 422–429. https://doi.org/10.1177/1533317515628052.
Chen, H. J., Gao, Y. Q., Che, C. H., Lin, H., & Ruan, X. L. (2018). Diffusion tensor imaging with tract-based spatial statistics reveals white matter abnormalities in patients with vascular cognitive impairment. Frontiers in Neuroanatomy, 12, 53. https://doi.org/10.3389/fnana.2018.00053.
Chua, T. C., Wen, W., Slavin, M. J., & Sachdev, P. S. (2008). Diffusion tensor imaging in mild cognitive impairment and Alzheimer’s disease: a review. Current Opinion in Neurology, 21(1), 83–92. https://doi.org/10.1097/WCO.0b013e3282f4594b.
Corbetta, M., & Shulman, G. L. (2002). Control of goal-directed and stimulus-driven attention in the brain. Nature Reviews. Neuroscience, 3(3), 201–215. https://doi.org/10.1038/nrn755.
de Vocht, F. (2007). [Health complaints and cognitive effects caused by exposure to MRI scanner magnetic fields]. Tijdschr Diergeneeskd, 132(2), 46–47. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/17334150.
Debette, S., Bombois, S., Bruandet, A., Delbeuck, X., Lepoittevin, S., Delmaire, C., Leys, D., & Pasquier, F. (2007). Subcortical hyperintensities are associated with cognitive decline in patients with mild cognitive impairment. Stroke, 38(11), 2924–2930. https://doi.org/10.1161/STROKEAHA.107.488403.
Della Nave, R., Foresti, S., Pratesi, A., Ginestroni, A., Inzitari, M., Salvadori, E., Giannelli, M., Diciotti, S., Inzitari, D., & Mascalchi, M. (2007). Whole-brain histogram and voxel-based analyses of diffusion tensor imaging in patients with leukoaraiosis: correlation with motor and cognitive impairment. AJNR. American Journal of Neuroradiology, 28(7), 1313–1319. https://doi.org/10.3174/ajnr.A0555.
Fan, L., Li, H., Zhuo, J., Zhang, Y., Wang, J., Chen, L., Yang, Z., Chu, C., Xie, S., Laird, A. R., Fox, P. T., Eickhoff, S. B., Yu, C., & Jiang, T. (2016). The human brainnetome atlas: a new brain atlas based on connectional architecture. Cerebral Cortex, 26(8), 3508–3526. https://doi.org/10.1093/cercor/bhw157.
Fazekas, F., Chawluk, J. B., Alavi, A., Hurtig, H. I., & Zimmerman, R. A. (1987). MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR. American Journal of Roentgenology, 149(2), 351–356. https://doi.org/10.2214/ajr.149.2.351.
Fazekas, F., Kleinert, R., Offenbacher, H., Schmidt, R., Kleinert, G., Payer, F., et al. (1993). Pathologic correlates of incidental MRI white matter signal hyperintensities. Neurology, 43(9), 1683–1689 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/8414012.
Fazekas, F., Kapeller, P., Schmidt, R., Offenbacher, H., Payer, F., & Fazekas, G. (1996). The relation of cerebral magnetic resonance signal hyperintensities to Alzheimer's disease. Journal of Neurological Science, 142(1-2), 121-125. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/8902731.
Filippi, M., van den Heuvel, M. P., Fornito, A., He, Y., Hulshoff Pol, H. E., Agosta, F., et al. (2013). Assessment of system dysfunction in the brain through MRI-based connectomics. Lancet Neurology, 12(12), 1189–1199. https://doi.org/10.1016/S1474-4422(13)70144-3.
Folstein, M. F., Folstein, S. E., & McHugh, P. R. (1975). “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12(3), 189-198. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/1202204.
Hachinski, V., Iadecola, C., Petersen, R. C., Breteler, M. M., Nyenhuis, D. L., Black, S. E., Powers, W. J., DeCarli, C., Merino, J. G., Kalaria, R. N., Vinters, H. V., Holtzman, D. M., Rosenberg, G. A., Wallin, A., Dichgans, M., Marler, J. R., & Leblanc, G. G. (2006). National Institute of Neurological Disorders and Stroke-Canadian stroke network vascular cognitive impairment harmonization standards. Stroke, 37(9), 2220–2241. https://doi.org/10.1161/01.STR.0000237236.88823.47.
Hansen, N. L., Lauritzen, M., Mortensen, E. L., Osler, M., Avlund, K., Fagerlund, B., & Rostrup, E. (2014). Subclinical cognitive decline in middle-age is associated with reduced task-induced deactivation of the brain's default mode network. Human Brain Mapping, 35(9), 4488–4498. https://doi.org/10.1002/hbm.22489.
Hughes, C. P., Berg, L., Danziger, W. L., Coben, L. A., & Martin, R. L. (1982). A new clinical scale for the staging of dementia. The British Journal of Psychiatry, 140, 566-572. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/7104545.
Jia, J., Zhou, A., Wei, C., Jia, X., Wang, F., Li, F., Wu, X., Mok, V., Gauthier, S., Tang, M., Chu, L., Zhou, Y., Zhou, C., Cui, Y., Wang, Q., Wang, W., Yin, P., Hu, N., Zuo, X., Song, H., Qin, W., Wu, L., Li, D., Jia, L., Song, J., Han, Y., Xing, Y., Yang, P., Li, Y., Qiao, Y., Tang, Y., Lv, J., & Dong, X. (2014). The prevalence of mild cognitive impairment and its etiological subtypes in elderly Chinese. Alzheimers Dement, 10(4), 439–447. https://doi.org/10.1016/j.jalz.2013.09.008.
Kim, S. H., Park, J. S., Ahn, H. J., Seo, S. W., Lee, J. M., Kim, S. T., Han, S. H., & Na, D. L. (2011). Voxel-based analysis of diffusion tensor imaging in patients with subcortical vascular cognitive impairment: correlates with cognitive and motor deficits. Journal of Neuroimaging, 21(4), 317–324. https://doi.org/10.1111/j.1552-6569.2010.00527.x.
Leech, R., Kamourieh, S., Beckmann, C. F., & Sharp, D. J. (2011). Fractionating the default mode network: distinct contributions of the ventral and dorsal posterior cingulate cortex to cognitive control. The Journal of Neuroscience, 31(9), 3217–3224. https://doi.org/10.1523/JNEUROSCI.5626-10.2011.
Li, J. C., Jin, D., Li, A., Liu, B., Song, C. Y., Wang, P., et al. (2019). ASAF: altered spontaneous activity fingerprinting in Alzheimer’s disease based on multisite fMRI. Science Bulletin, 64(14), 998–1010. https://doi.org/10.1016/j.scib.2019.04.034.
Lin, L., Xue, Y., Duan, Q., Sun, B., Lin, H., Chen, X., Luo, L., Wei, X., & Zhang, Z. (2015). Microstructural white matter abnormalities and cognitive dysfunction in subcortical ischemic vascular disease: an atlas-based diffusion tensor analysis study. Journal of Molecular Neuroscience, 56(2), 363–370. https://doi.org/10.1007/s12031-015-0550-5.
Liu, Q., Zhu, Z., Teipel, S. J., Yang, J., Xing, Y., Tang, Y., & Jia, J. (2017). White matter damage in the cholinergic system contributes to cognitive impairment in subcortical vascular cognitive impairment, no dementia. Frontiers in Aging Neuroscience, 9, 47. https://doi.org/10.3389/fnagi.2017.00047.
Lopez-Oloriz, J., Lopez-Cancio, E., Arenillas, J. F., Hernandez, M., Dorado, L., Dacosta-Aguayo, R., et al. (2014). Diffusion tensor imaging, intracranial vascular resistance and cognition in middle-aged asymptomatic subjects. Cerebrovascular Diseases, 38(1), 24–30. https://doi.org/10.1159/000363620.
Mansfield, A., Inness, E. L., & McIlroy, W. E. (2018). Stroke. Handbook of Clinical Neurology, 159, 205–228. https://doi.org/10.1016/B978-0-444-63916-5.00013-6.
Mintun, M. A., Larossa, G. N., Sheline, Y. I., Dence, C. S., Lee, S. Y., Mach, R. H., Klunk, W. E., Mathis, C. A., DeKosky, S., & Morris, J. C. (2006). [11C]PIB in a nondemented population: potential antecedent marker of Alzheimer disease. Neurology, 67(3), 446–452. https://doi.org/10.1212/01.wnl.0000228230.26044.a4.
Mirsen, T. R., Lee, D. H., Wong, C. J., Diaz, J. F., Fox, A. J., Hachinski, V. C., & Merskey, H. (1991). Clinical correlates of white-matter changes on magnetic resonance imaging scans of the brain. Archives of Neurology, 48(10), 1015–1021. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/1929891.
Nitkunan, A., McIntyre, D. J., Barrick, T. R., O'Sullivan, M., Shen, Y., Clark, C. A., et al. (2006). Correlations between MRS and DTI in cerebral small vessel disease. NMR in Biomedicine, 19(5), 610–616. https://doi.org/10.1002/nbm.1052.
O'Sullivan, M., Morris, R. G., Huckstep, B., Jones, D. K., Williams, S. C., & Markus, H. S. (2004). Diffusion tensor MRI correlates with executive dysfunction in patients with ischaemic leukoaraiosis. Journal of Neurology, Neurosurgery, and Psychiatry, 75(3), 441–447. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/14966162.
Pinto, T. C. C., Machado, L., Bulgacov, T. M., Rodrigues-Junior, A. L., Costa, M. L. G., Ximenes, R. C. C., & Sougey, E. B. (2018). Is the Montreal Cognitive Assessment (MoCA) screening superior to the mini-mental state examination (MMSE) in the detection of mild cognitive impairment (MCI) and Alzheimer’s disease (AD) in the elderly? International Psychogeriatrics, 1–14. https://doi.org/10.1017/S1041610218001370.
Qiu, A., Fennema-Notestine, C., Dale, A. M., Miller, M. I., & Alzheimer’s disease neuroimaging, I. (2009). Regional shape abnormalities in mild cognitive impairment and Alzheimer's disease. Neuroimage, 45(3), 656–661. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/19280688.
Raichle, M. E., MacLeod, A. M., Snyder, A. Z., Powers, W. J., Gusnard, D. A., & Shulman, G. L. (2001). A default mode of brain function. Proceedings of the National Academy of Sciences of the United States of America, 98(2), 676–682. https://doi.org/10.1073/pnas.98.2.676.
Robinson, J. L., Baxi, M., Katz, J. S., Waggoner, P., Beyers, R., Morrison, E., Salibi, N., Denney, T. S., Vodyanoy, V., & Deshpande, G. (2016). Characterization of structural connectivity of the default mode network in dogs using diffusion tensor imaging. Scientific Reports, 6, 36851. https://doi.org/10.1038/srep36851.
Rockwood, K., Wentzel, C., Hachinski, V., Hogan, D. B., MacKnight, C., & McDowell, I. (2000). Prevalence and outcomes of vascular cognitive impairment. Vascular Cognitive impairment investigators of the Canadian Study of Health and Aging. Neurology, 54(2), 447–451. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/10668712.
Rosazza, C., & Minati, L. (2011). Resting-state brain networks: literature review and clinical applications. Neurological Sciences, 32(5), 773–785. https://doi.org/10.1007/s10072-011-0636-y.
Sachdev, P., Kalaria, R., O'Brien, J., Skoog, I., Alladi, S., Black, S. E., et al. (2014). Diagnostic criteria for vascular cognitive disorders: a VASCOG statement. Alzheimer Disease and Associated Disorders, 28(3), 206–218. https://doi.org/10.1097/WAD.0000000000000034.
Scheltens, P., Leys, D., Barkhof, F., Huglo, D., Weinstein, H. C., Vermersch, P., ... Valk, J. (1992). Atrophy of medial temporal lobes on MRI in “probable” Alzheimer's disease and normal ageing: diagnostic value and neuropsychological correlates. Journal of Neurology, Neurosurgery, and Psychiatry, 55(10), 967-972. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/1431963.
Seo, S. W., Ahn, J., Yoon, U., Im, K., Lee, J. M., Tae Kim, S., Ahn, H. J., Chin, J., Jeong, Y., & Na, D. L. (2010). Cortical thinning in vascular mild cognitive impairment and vascular dementia of subcortical type. Journal of Neuroimaging, 20(1), 37–45. https://doi.org/10.1111/j.1552-6569.2008.00293.x.
Seo, S. W., Lee, J. M., Im, K., Park, J. S., Kim, S. H., Kim, S. T., Ahn, H. J., Chin, J., Cheong, H. K., Weiner, M. W., & Na, D. L. (2012). Cortical thinning related to periventricular and deep white matter hyperintensities. Neurobiology of Aging, 33(7), 1156–1167. https://doi.org/10.1016/j.neurobiolaging.2010.12.003.
Skrobot, O. A., Black, S. E., Chen, C., DeCarli, C., Erkinjuntti, T., Ford, G. A., et al. (2018). Progress toward standardized diagnosis of vascular cognitive impairment: guidelines from the vascular impairment of cognition classification consensus study. Alzheimers Dement, 14(3), 280–292. https://doi.org/10.1016/j.jalz.2017.09.007.
Stephan, B. C., Matthews, F. E., Khaw, K. T., Dufouil, C., & Brayne, C. (2009). Beyond mild cognitive impairment: vascular cognitive impairment, no dementia (VCIND). Alzheimer's Research & Therapy, 1(1), 4. https://doi.org/10.1186/alzrt4.
Sun, Y. W., Qin, L. D., Zhou, Y., Xu, Q., Qian, L. J., Tao, J., & Xu, J. R. (2011). Abnormal functional connectivity in patients with vascular cognitive impairment, no dementia: a resting-state functional magnetic resonance imaging study. Behavioural Brain Research, 223(2), 388–394. https://doi.org/10.1016/j.bbr.2011.05.006.
Tao, Y., Liu, B., Zhang, X., Li, J., Qin, W., Yu, C., & Jiang, T. (2015). The structural connectivity pattern of the default mode network and its association with memory and anxiety. Frontiers in Neuroanatomy, 9, 152. https://doi.org/10.3389/fnana.2015.00152.
Thong, J. Y., Du, J., Ratnarajah, N., Dong, Y., Soon, H. W., Saini, M., et al. (2014). Abnormalities of cortical thickness, subcortical shapes, and white matter integrity in subcortical vascular cognitive impairment. Human Brain Mapping, 35(5), 2320–2332. https://doi.org/10.1002/hbm.22330.
van de Pol, L. A., Korf, E. S., van der Flier, W. M., Brashear, H. R., Fox, N. C., Barkhof, F., & Scheltens, P. (2007). Magnetic resonance imaging predictors of cognition in mild cognitive impairment. Archives of Neurology, 64(7), 1023–1028. https://doi.org/10.1001/archneur.64.7.1023.
van Straaten, E. C., Fazekas, F., Rostrup, E., Scheltens, P., Schmidt, R., Pantoni, L., et al. (2006). Impact of white matter hyperintensities scoring method on correlations with clinical data: the LADIS study. Stroke, 37(3), 836–840. https://doi.org/10.1161/01.STR.0000202585.26325.74.
Weiler, M., de Campos, B. M., Nogueira, M. H., Pereira Damasceno, B., Cendes, F., & Balthazar, M. L. (2014). Structural connectivity of the default mode network and cognition in Alzheimers disease. Psychiatry Research, 223(1), 15–22. https://doi.org/10.1016/j.pscychresns.2014.04.008.
Winblad, B., Palmer, K., Kivipelto, M., Jelic, V., Fratiglioni, L., Wahlund, L. O., Nordberg, A., Bäckman, L., Albert, M., Almkvist, O., Arai, H., Basun, H., Blennow, K., de Leon, M., DeCarli, C., Erkinjuntti, T., Giacobini, E., Graff, C., Hardy, J., Jack, C., Jorm, A., Ritchie, K., van Duijn, C., Visser, P., & Petersen, R. C. (2004). Mild cognitive impairment--beyond controversies, towards a consensus: report of the International Working Group on Mild Cognitive Impairment. Journal of Internal Medicine, 256(3), 240–246. https://doi.org/10.1111/j.1365-2796.2004.01380.x.
Xie, S., Chen, L., Zuo, N., & Jiang, T. (2016). DiffusionKit: A light one-stop solution for diffusion MRI data analysis. Journal of Neuroscience Methods, 273, 107–119. https://doi.org/10.1016/j.jneumeth.2016.08.011.
Xu, Q., Zhou, Y., Li, Y. S., Cao, W. W., Lin, Y., Pan, Y. M., & Chen, S. D. (2010). Diffusion tensor imaging changes correlate with cognition better than conventional MRI findings in patients with subcortical ischemic vascular disease. Dementia and Geriatric Cognitive Disorders, 30(4), 317–326. https://doi.org/10.1159/000320491.
Zarei, M., Damoiseaux, J. S., Morgese, C., Beckmann, C. F., Smith, S. M., Matthews, P. M., Scheltens, P., Rombouts, S. A., & Barkhof, F. (2009). Regional white matter integrity differentiates between vascular dementia and Alzheimer disease. Stroke, 40(3), 773–779. https://doi.org/10.1161/STROKEAHA.108.530832.
Zhan, Y. F., Yao, H. X., Wang, P., Zhou, B., Zhang, Z. Q., Guo, Y. E., et al. (2016). Network-based statistic show aberrant functional connectivity in Alzheimer’s disease. Ieee Journal of Selected Topics in Signal Processing, 10(7), 1182–1188. https://doi.org/10.1109/Jstsp.2016.2600298.
Zhang, M. Y., Katzman, R., Salmon, D., Jin, H., Cai, G. J., Wang, Z. Y., et al. (1990). The prevalence of dementia and Alzheimer’s disease in Shanghai, China: Impact of age, gender, and education. Annals of Neurology, 27(4), 428–437. https://doi.org/10.1002/ana.410270412.
Zhou, Y., Lin, F. C., Zhu, J., Zhuang, Z. G., Li, Y. S., Tao, J., Qian, L. J., Xu, J. R., & Lei, H. (2008). Whole brain diffusion tensor imaging histogram analysis in vascular cognitive impairment. Journal of the Neurological Sciences, 268(1–2), 60–64. https://doi.org/10.1016/j.jns.2007.11.005.
Zhou, Y., Qun, X., Qin, L. D., Qian, L. J., Cao, W. W., & Xu, J. R. (2011). A primary study of diffusion tensor imaging-based histogram analysis in vascular cognitive impairment with no dementia. Clinical Neurology and Neurosurgery, 113(2), 92–97. https://doi.org/10.1016/j.clineuro.2010.09.007.
Funding
This work was partially supported by Beijing Natural Science Foundation (JQ19024), National Natural Science Foundation of China (81671040, 81970996), Beijing Municipal Science & Technology Commission (Z191100006619046, Z171100000117001) and the Strategic Priority Research Program (B) of the Chinese Academy of Sciences (XDB32020200).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOC 202 kb)
Rights and permissions
About this article
Cite this article
Qin, Q., Tang, Y., Dou, X. et al. Default mode network integrity changes contribute to cognitive deficits in subcortical vascular cognitive impairment, no dementia. Brain Imaging and Behavior 15, 255–265 (2021). https://doi.org/10.1007/s11682-019-00252-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-019-00252-y